Burns and Inhalational Injury
KEY POINTS
1 For burn victims, the keystones of initial therapy are large-volume crystalloid resuscitation and maintenance of the airway. Commonly, isotonic crystalloid (4 mL/kg/% body surface area burn) is required for volume resuscitation during the first 24 h after a burn injury.
2 Inhalational damage is a very common early injury that is usually best managed initially by intubation and administration of 100% oxygen.
3 Carbon monoxide and cyanide poisoning should be considered in every burn victim. The role of hyperbaric oxygen therapy for carbon monoxide poisoning remains controversial but perhaps is best limited to comatose patients with high carbon monoxide-hemoglobin levels who can be treated promptly. Antidotes are available for cyanide and should be administered to patients with unexplained metabolic acidosis persisting after apparently adequate resuscitation.
4 Severe sepsis is the most common late fatal complication of burns, usually related to Gram-negative rod infection of the burn wound.
5 The hypermetabolic state and compartmental fluid shifts often dramatically alter drug therapy in the patient with burns. In many cases, drug doses must be significantly increased to achieve therapeutic effect.
6 Burn wounds are metabolically taxing, requiring huge amounts of energy and patient work to maintain an often dramatically elevated minute ventilation and cardiac output. Patients with marginal ventilatory status can develop respiratory failure from excessive ventilatory demands.
▪ PATHOPHYSIOLOGY
In serious burns, some tissue is immediately killed by direct thermal injury but adjoining regions that are sublethally injured may be even more important, as they serve as an engine for inflammation. The tissue bordering a major burn generates inflammatory cytokines, oxidants, and lipid mediators that act locally and systemically to increase vascular permeability and clotting and to depress cardiovascular function. These changes result in the familiar clinical findings of fever, leukocytosis, and increased vascular permeability that manifest as hypoproteinemia, edema, and hypovolemia. Similar to the brain adjacent to a cerebral infarct, the “watershed” tissue bordering an acute burn is in jeopardy for additional damage from systemic hypoxia, ischemia due to localized clotting and increased tissue pressure, and infection. Thus, prompt reperfusion of these endangered areas is vital to optimal outcome.
▪ BURN EVALUATION
Mortality rates for burn victims vary widely, depending on the depth and size of the burn, the patient’s underlying health and age, and the occurrence of associated inhalational injury. Most deaths from fires result from smoke inhalation, which usually proves fatal before patients reach the hospital—emphasizing the importance of smoke detection devices. On reaching the hospital, hypovolemic shock and smoke-induced airflow obstruction are prominent early complications; severe sepsis is the most common late fatal complication. Inhalational injury is a major determinant of outcome; its occurrence may double the mortality rate of a burn of any given extent. Not surprisingly, age also is a powerful predictor of mortality. After the airway has been secured and hemodynamics have been stabilized, the patient should be examined carefully to determine the depth and extent of thermal injury, and the burns should be gently washed and dressed. An appropriate examination should be conducted to look for associated traumatic injuries, especially if the burn results from explosion or motor vehicle accident.
Estimation of Burn Size and Severity
Burns are classified either simply by partial or full thickness destruction or by depth of injury (first to fourth degree) (Table 38-1). In adults, the percentage of body surface affected by burn injury can be estimated by the “rule of nines.” This rule assigns percentages of the total body surface area (BSA) to the anterior and posterior surfaces of the head, limbs, and trunk (Fig. 38-1). As another useful measure, the palm of the adult patient’s hand approximates 1% of total BSA. The Lund-Browder chart is used for estimating the extent of the burn in children because their head contributes a disproportionally large proportion of body surface. Estimation of the total area involved by full thickness burns is useful in determining fluid requirements, need for specialized burn unit care, and expected mortality. However, precise grading of burn wound depth is not essential for the nonburn specialist; in most cases it is reasonable to regard any burn more extensive than superficial as serious, particularly if it covers ≥10% of the body. Adults with extensive or severe burns and most burned children require hospitalization. Commonly accepted criteria for hospital admission are given in Table 38-2.
▪ INITIAL MANAGEMENT
Initial management of the patient with severe burns should include a careful assessment of the airway and vital signs to ensure adequate ventilation and perfusion. If carbon monoxide (CO) poisoning is suspected, it is reasonable to obtain a blood sample for CO content and to simultaneously administer 100% oxygen to accelerate the poison’s clearance. Immediately after securing the airway and ensuring oxygenation, repletion of circulating volume should be undertaken; hypovolemic shock is the most common cause of death within the first 24 h after admission.
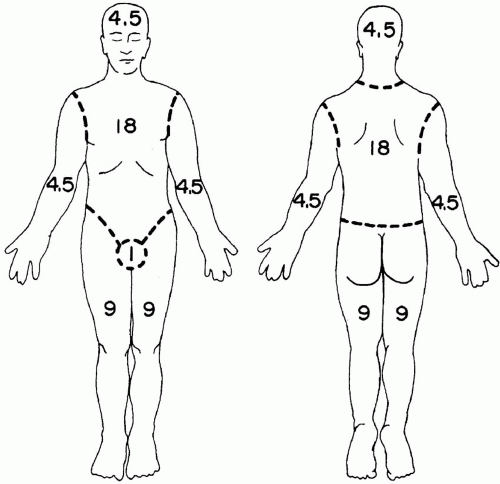 FIGURE 38-1 Burn wound diagram illustrating the surface area of selected body regions. Numbers correspond to percentages of total BSA. |
TABLE 38-1 CLASSIFICATION OF BURNS BY SEVERITY | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||
The optimal endpoints for circulatory resuscitation and how to achieve these goals remain controversial. Many intensivists rely on the traditional indices of heart rate, blood pressure, and urine output, but it has been claimed that some patients remain underresuscitated using these measures. When adequacy of intravascular filling is in doubt, assessment of central venous pressure (CVP) can be helpful. Although some physicians prefer an intensive monitoring strategy that includes measurement of CVP, pulmonary artery occlusion pressure
(PAOP), continuous mixed-venous oxygen saturation (SvO2), and frequent lactate determinations, there are no data to indicate that these measures add value. Even when invasive monitoring is undertaken, recent targets are often lower than those traditionally used (e.g., CVP 8 to 10 cm H2O, PAOP 10 to 12 cm H2O, SvO2 60% to 65%). Measuring PAOP and cardiac output seems most defensible in patients with suspected underlying cardiac impairment, where CVP alone may not provide sufficient information about left ventricular function (see Chapter 3). Difficulties in achieving adequate resuscitation of burn patients frequently can be traced to myocardial dysfunction, often transient, that presumably results from humoral myocardial depressant factors.
(PAOP), continuous mixed-venous oxygen saturation (SvO2), and frequent lactate determinations, there are no data to indicate that these measures add value. Even when invasive monitoring is undertaken, recent targets are often lower than those traditionally used (e.g., CVP 8 to 10 cm H2O, PAOP 10 to 12 cm H2O, SvO2 60% to 65%). Measuring PAOP and cardiac output seems most defensible in patients with suspected underlying cardiac impairment, where CVP alone may not provide sufficient information about left ventricular function (see Chapter 3). Difficulties in achieving adequate resuscitation of burn patients frequently can be traced to myocardial dysfunction, often transient, that presumably results from humoral myocardial depressant factors.
TABLE 38-2 CRITERIA FOR HOSPITAL ADMISSION | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Fluid Therapy
Burns cause hypovolemia as a result of massive shifts of fluid from intravascular to extravascular compartments and by exudation through injured skin. Hemoconcentration (because of intravascular fluid losses) occurs early, but hemodilution is more likely after appropriate fluid resuscitation. Because the hematocrit can change in either direction, it should be checked regularly during resuscitation with a traditional target being ≥30%. Central venous catheterization is often necessary to deliver the volume of fluid required for adequate resuscitation, and whenever possible such catheters should be placed though unburned skin to minimize the risk of subsequent catheter or wound related sepsis.
Three major strategies (i.e., Evans, Brooke, and Parkland) have been advocated for replacing circulating volume (Table 38-3). A central feature of all plans is to administer substantial volumes of salt-containing (typically Ringers lactate) fluid during the initial 24 h. These strategies differ in their reliance on colloid and free water. The Parkland formula is probably the most widely used fluid-replacement strategy, according to which 4mL of isotonic crystalloid per kilogram per percentage of BSA burn is given in the first day. Customarily, one half of the fluid deficit is replaced in the first 8 h, with the remainder administered over the next 16 h. (For purposes of fluid replacement, burn area is usually capped at 50% BSA.) However, patients with concomitant inhalational injury may require more fluid for successful resuscitation (up to 6 mL/kg/% BSA burn). A traditional fluid replacement target has been to achieve 0.5 to 1 mL/kg/h of urine output. It is now recognized that in a substantial number, perhaps half, of cases too much volume is administered. One clinical clue to too much fluid infusion is a urine output consistently exceeding 2 mL/kg/h. Other risks of excessive fluid administration are limb and abdominal compartment syndromes (ACS). ACS is sufficiently common to warrant monitoring of bladder pressure in patients undergoing large volume resuscitation. All fluid-replacement strategies are associated with the development of tissue edema; however, newer strategies using hypertonic (250 mmol/L) saline solution may achieve hemodynamic resuscitation with less swelling. (There is some evidence that hypertonic resuscitation strategies may increase the risk of renal insufficiency.) Although poorly tested, in mass casualty situations where intravenous therapy may not be feasible, oral rehydrating solution may be useful. Following fluid replacement, vasopressors may be needed to maintain adequate cardiac output, blood pressure, and urine flow. High doses of α-adrenergic agonists (e.g., norepinephrine, phenylephrine) should be avoided, if possible, because of their tendency to decrease nutritive blood flow to already injured tissue.
TABLE 38-3 FIRST DAY FLUID-REPLACEMENT STRATEGIES | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
After 24 h, sodium requirements decline and permeability of leaky vessels decreases. Free water and colloid are then administered in larger quantities to maintain circulating volume and electrolyte balance. After the first 24 h, evaporative water losses may be estimated by the following formula: hourly water loss (in mL) = (25 + % area of burn) × (total
BSA in m2). This formula predicts that a patient with a 25% burn and a 2 m2 BSA will lose approximately 100 mL of water per hour. This formula provides the basis for the common recommendation in both the Brooke and Evans fluid strategies to administer roughly 2 L of free water daily. Within the first 12 h of the burn event, colloids offer little advantage over crystalloid because the newly injured vasculature fails to retain even the larger colloid molecules. Despite lack of proven benefit, many physicians still administer albumin to decrease the amount of crystalloid used, especially when the serum albumin concentration falls below 2 gm /dL.
BSA in m2). This formula predicts that a patient with a 25% burn and a 2 m2 BSA will lose approximately 100 mL of water per hour. This formula provides the basis for the common recommendation in both the Brooke and Evans fluid strategies to administer roughly 2 L of free water daily. Within the first 12 h of the burn event, colloids offer little advantage over crystalloid because the newly injured vasculature fails to retain even the larger colloid molecules. Despite lack of proven benefit, many physicians still administer albumin to decrease the amount of crystalloid used, especially when the serum albumin concentration falls below 2 gm /dL.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








