11
Burns
Introduction
Despite legislative attempts to improve safety and increase public awareness, patients with burn injuries remain a significant proportion of trauma patients attending emergency departments (EDs) (Herndon 2007). Each year in the UK, it is estimated that 175 000 people visit EDs with acute burn injuries and some 13 000 of them need admission to hospital (Dunn 2000). Add to this the number of individuals treated as outpatients and in community and primary care settings, and the scale of the problem becomes apparent (Moss 2010). Although the chances for survival following the massive trauma of a major burn have improved steadily over the last 25 years, there are still 300 deaths in hospital each year in the UK (National Audit Office 2010, NHS Clinical Advisory Group 2010).
The care provided in the first few hours after injury is crucial (Wiebelhaus & Hansen 2001) and without pertinent and urgent treatment the chances of surviving a major burn are greatly reduced. Burn injuries should be thought of as more than ‘skin deep’: they represent a complicated assault on the body’s vital organs and systems. Management of major burn injuries must reflect this, and through effective organization and prioritization of care, potentially life-threatening problems can be dealt with successfully, or in some cases avoided in the first instance.
Assessment
First aid can overlap the initial ED management of burn injuries, especially when first aid has not been commenced at the scene of the incident. Decisions and treatment received at the scene, particularly the quality of first aid, often have a profound effect on mortality and morbidity (Dunn 2000). In a stressful situation confusion often exists over what constitutes safe first aid, particularly for the layperson.
Appropriate action can be summarized as:
• safe removal from the source of the burn – rescuers should be aware of any potential risk or immediate danger from the environment, to themselves, before attempting to remove the casualty
• arresting the burning process by application of cold water to reduce residual heat in body tissues or to remove corrosive substances
• protection of damaged skin from desiccation and infection.
During this period it is important to obtain a brief, accurate history of the event (Settle 1995). Establishing what, where, when, why and how injuries happened will enable appropriate, prioritized care to be commenced promptly.
This can be taken from the patient, relatives or ambulance crew (Box 11.1).
Airway and breathing
The first priority in the management of a burn-injured patient is immediate assessment of the patient’s airway for patency and maintenance (Jones 2003). Inhalation injury and respiratory complications are two of the leading causes of fatality in the early period following burn injury (Zassan et al. 2010). The early detection and treatment of airway or breathing problems must be paramount in the patient’s overall management. Thermal inhalation (direct heat) and chemical inhalation injuries pose the greatest threat to airways and breathing with an incidence of 20–30 % and at least 30 % of patients with inhalation injury die (Smith et al. 1994). A direct heat injury will be evident soon after injury. Unless steam inhalation has occurred, the damage is usually limited to the upper airway. Direct heat injury causes face, neck and intraoral burns and leads to a rapid development of oedema, resulting in complete airway obstruction within hours (Wilding 1990).
Chemical inhalation usually involves the by-products of combustion. The most worrying toxins are those that asphyxiate patients, depriving them of oxygen, carbon monoxide (CO) and cyanide (Jones 2003). The chemicals affect the lower airways, causing alveolar damage, pulmonary oedema and surfactant insufficiency. They reduce the circulatory availability of oxygen because carbon monoxide has a much greater affinity for haemoglobin (Hb) than oxygen, and subsequently induce acidosis. Chemical inhalation should be suspected following a loss of or altered consciousness, history of fire within an enclosed or confined area, the presence of intraoral burns and soot in the mouth, nose and sputum, and where a confirmed history of smoke inhalation exists.
During the airway assessment, also check for cervical spine injury and take appropriate precautions. If you need to open the airway and you suspect a cervical spine injury, use a combined jaw thrust and spine immobilization manoeuvre. Apply a hard cervical collar if indicated, even if it goes over the burn (see also Chapter 7).
In less severe cases, where there is no direct evidence of airway involvement, close and careful observations should be continued as symptoms may become apparent over the next 24 to 48 hours (Muehlberger et al. 1998). The ED nurse should not be misled by the apparent mildness of symptoms. This is often an inaccurate indicator of the degree of damage occurring, and the patient’s condition should be continually reviewed for increasing shortness of breath, feelings of tightness, wheezing or hoarseness. The patient’s chest should be adequately visualized for respiratory effort and bilateral movement. Percussion and auscultation should be performed to determine adequate air entry, and to detect wheezing, signs of pulmonary oedema and lower airway obstruction.
All patients with suspected inhalation injuries should be given high-flow 100 % oxygen as soon as possible (McParkland 1999). The administration of high levels of oxygen, via either mask or endotracheal tube, greatly reduces the half-life of carboxyhaemoglobin (COHb) and increases its rate of elimination from the body. This reduces systemic hypoxia. Measuring this can prove difficult in the ED, because the usual methods such as oxygen saturation monitoring are rendered ineffective as they do not distinguish between oxy- and carboxyhaemoglobin (Wiebelhaus & Hansen 2001). The actual diagnosis of an inhalation injury is often difficult to confirm in the initial stages of care. Investigations include immediate arterial blood gas analysis as a baseline for the evaluation of the patient’s pulmonary status, with sequential arterial blood gas measurements to confirm CO elimination (Campbell 2000). Oxygen saturation monitoring should not be used until blood gas analysis reveals that COHb concentrations have reached a normal level.
Measurement of COHb and cyanide levels is important, but results are not always immediately available to ED staff. Fibre-optic bronchoscopy is valuable as a secondary investigation to confirm the presence of soot in the lower respiratory tract (Muehlberger et al. 1998). Because of the difficulty in diagnosis, objective observation and reporting of respiratory changes by the emergency nurse provide the subtle indicators needed to decide the treatment needed. Burn injuries result in a significant increase in respiratory tract secretion as part of the histamine response. If the patient has a compromised airway or is intubated, regular suctioning may be necessary to clear the airway of excessive secretions. Circumferential full-thickness burns to the neck and chest may compromise the mechanism of breathing and necessitate emergency escharotomy (Settle 1995). Chest X-rays are usually obtained, but they do not often show early signs of respiratory problems, although they may highlight other injuries.
Circulation
The patient with major burns will develop severe hypovolaemic shock within 3–4 hours from the time of injury, unless adequate fluid resuscitation measures are initiated (Settle 1995). Damage to the capillary network in the skin leads to loss of water, proteins and electrolytes from the circulation into the interstitial compartment (Hettiaratchy & Dziewulski 2004). There are three reasons for this: wound secretion, evaporation and localized oedema. In severe cases, generalized oedema in surrounding, apparently uninjured, areas also occurs. The oedema occurs because of changes in permeability of capillaries and tissues affected by heat. Fluid consists mostly of dilute plasma, which increases the viscosity of the remaining intravascular fluid and slows or stops blood flow to capillaries. Poor tissue perfusion increases the extent of the burn because of low oxygen (Cook 1997). If this process is left unchecked, severe shock is likely, but given the predictability of fluid loss, the principal aim of care is to anticipate it and compensate with fluid resuscitation (Settle 1995). The greatest amount of fluid loss in burn patients is in the first 24 hours after injury.
Loss of circulating volume always occurs following a major burn injury. Cardiac output is reduced by about a third within the first hour of injury (Cook 1997). Normal compensatory mechanisms allow homeostasis to be maintained initially, but fluid resuscitation is vital if this is to be maintained. Rapid initial transfusion may result in little improvement. It does, however, reduce the impact of a further reduction of cardiac output around six hours post-injury. Although haemoglobin becomes more fragile and has a shorter lifespan following a significant burn injury, blood transfusion is not recommended in initial management as it may increase the viscosity of intracellular fluid. Haemolysis will occur in transfused blood, therefore reducing its effectiveness.
Fluid replacement
Intravenous (i.v.) access with large-calibre i.v. lines must be established immediately in a peripheral vein (American College of Surgeons 2008). If possible, place two large-bore i.v. devices through unburned skin. If placement of the i.v. cannula is in a burned area, ensure the cannula is correctly and securely inserted into the vein, as swelling will push the hub out and may cause infiltration.
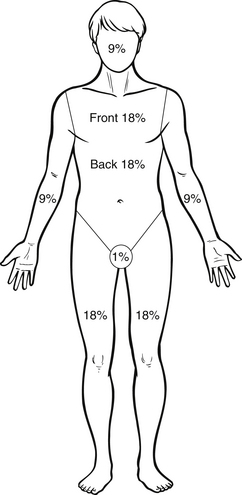
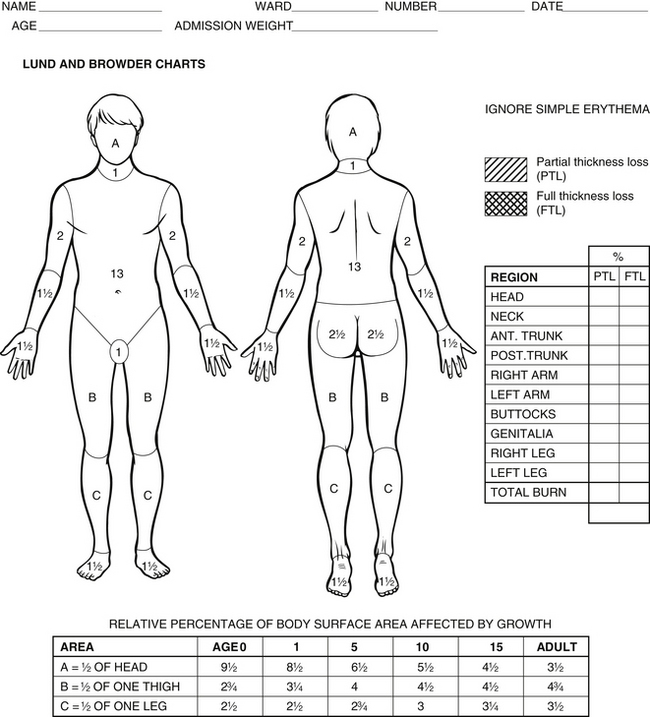
To accurately determine the amount of fluid required, it is necessary to assess the area of body surface damaged by burn injury. The ‘rule of nines’ (Fig. 11.1) is a convenient tool for a quick initial assessment. The rule of nines cannot be used for children because a child’s body has different proportions. The Lund–Browder (1944) assessment guide (Fig. 11.2) enables a more accurate assessment, as it allows for surface area variations with age. If the surface area burned exceeds 15 % in adults or 10 % in children and the elderly, intravenous fluid resuscitation is indicated: over 20 % and this resuscitation becomes urgent (Wiebelhaus & Hansen 2001). It is also possible to estimate the patient’s likelihood of survival based on the percentage area of body burned (Table 11.1).
Table 11.1
Statistical values of mortality with age and percentage area of body burned
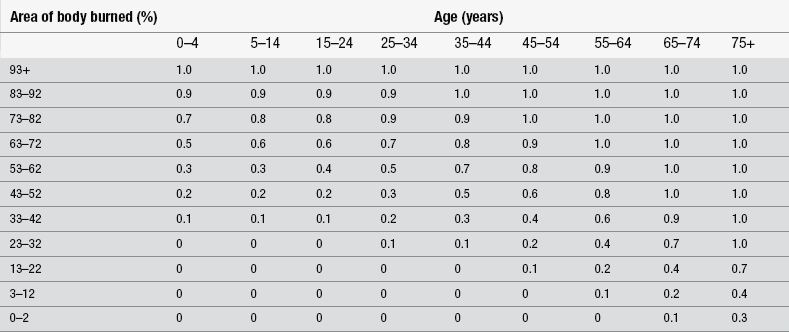
01 = 10% mortality; 0.9 = 90% mortality.
(After Bull, JP. (1971) Revised analysis of mortality due to burns. The Lancet, 298 (7734), 1133 – 1134.)
The Parkland formula
This calculates the amount of fluid required in the first 24 hours. Children require maintenance fluid in addition to this (Boxes 11.2, 11.3).
At the end of the 24 hours, colloid infusion is begun at a rate of:
and maintenance crystalloid is continued at a rate of:
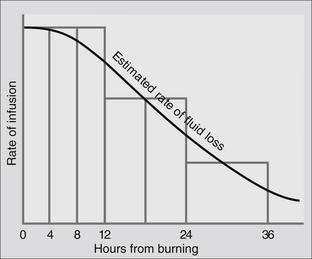
A fluid resuscitation formula can help to reduce inaccuracies in fluid replacement, particularly when assessment has to be made by inexperienced staff, but these formulae only act as a guideline for infusion. Actual amounts of fluid administered should reflect the condition of the patient. The amount of fluid given should be continuously adjusted according to the individual patient’s response, to maintain a urinary output of 0.5–1 mL/kg/h (adult) or 1–1.5 mL/kg/h (child) (American College of Surgeons 2008) and other physiological parameters (pulse, blood pressure and respiratory rate) (Fig. 11.3).
There is no agreement on the type of fluid that should be used for resuscitating the burn-injured patient. Colloids have no advantage over crystalloids in the initial management to maintain circulatory volume (Heittiaratchy & Papini 2004). In the UK, Hartmann’s solution (sodium chloride 0.6 %, sodium lactate 0.25 %, potassium chloride 0.04 %, calcium chloride 0.027 %) is the most commonly used crystalloid. Crystalloids are given to supplement that used by metabolic requirements, which tend to increase following injury. In adults, 50 mL/h of sodium base crystalloid should be given to maintain metabolic function. In children, fluid replacement should be titrated by the child’s weight (Wilson 1997) (Box 11.2). Colloid use is controversial. However, a lot of protein is lost through the burn wound, so there is a need to replace this: some units introduce colloid after 8 hours, as the capillary leak begins to shut down; others wait 24 hours. Fresh frozen plasma is often used in children and albumin in adults (Heittiaratchy & Papini 2004).
Secondary survey
In the resuscitation phase, even seemingly well patients with a major burn should be kept nil by mouth because of the risk of developing paralytic ileus. If this occurs, gastric aspiration via nasogastric tube may be necessary to prevent persistent vomiting. During resuscitation, frequent monitoring is necessary to detect changes and to attempt to maintain the patient’s stability. By using several indicators to give a picture of the patient’s overall condition, appropriate clinical decisions can be made.