The Pink Puffer |.
Anatomic definition: progressive destruction of alveolar septa/ capillaries leading to airspace enlargement and development of bullae. PFT’s show decr DLCO, incr RC and decr FEV/FVC. Link: See COPD | At autopsy, some areas of emphysema are found in the lungs of most persons >60 yo. Defined in pathologic terms on the basis of findings of abnormal permanent enlargement of air spaces distal to the terminal bronchiole, accompanied by the destruction of the alveolar walls without obvious fibrosis. Most use the terms COPD, chronic obstructive lung disease and chronic airflow obstruction (CAO) are synonyms used to describe the minimally reversible airflow obstruction caused by chronic bronchitis, emphysema, or both.
X-ray: incr AP diameter & ant clear space, sternophrenic angle >90 deg or inverted (flattened diaphragm) Pan-acinar (worse at base where blood flow is and alpha-1-Antitrypsin Def) or Centrilobular (smokers, where irritation is). Tx with retinoic acids to increase lung alveoli and regeneration of elastase.
• Lung damage and inflammation of the air sacs (alveoli) will result in emphysema. Emphysema is defined as enlargement of the air spaces distal to the terminal bronchioles, with destruction of their walls. The destruction of air space walls reduces the surface area available for the exchange of oxygen and carbon dioxide during breathing. It also reduces the elasticity of the lung itself, which results in a loss of support for the airways that are embedded in the lung. These airways are more likely to collapse causing further limitation to airflow.
2 types:
– Centroacinar: smokers: area near terminal bronchiole (not alveolar sac). Centrilobular: proximal to central parts of acini (air spaces closer to bronchioles) are affected.
– Panacinar: alpha-1-antitrypsin deficiency: entire acinus (terminal bronchiole thru alveolar sac). Panacinar / panlobular: enlargement of all air spaces (from bronchioles to terminal blind alveoli). This type is associated with alpha-1-antitrypsin deficiency. Less than 5% of emphysema from alpha-1 deficiency. Smoking exacerbates emphysema formation in A1A deficiency. Alpha-1-antitrypsin deficiency: bullae in the lung bases.
Alveolar capillary destruction is due to imbalance between proteases and antiproteases.
– Increased protease activity. Proteolytic elastase from neutrophils (tobacco smoke).
Other: Distal acinar / paraseptal: proximal acinus normal, distal acinus affected.
Irregular: various parts of acinus involved. Associated with fibrosis.
The third most frequent chronic disease of airways and is an irreversible dilation of the airway due to chronic infection or inflammation.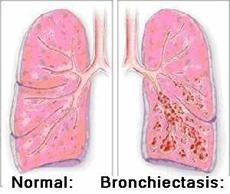
 A chronic condition characterized by irreversible dilation of the bronchi associated with damage of bronchial walls. Persistent pathologic dilatation of the bronchi due to breakdown of bronchial walls.
A chronic condition characterized by irreversible dilation of the bronchi associated with damage of bronchial walls. Persistent pathologic dilatation of the bronchi due to breakdown of bronchial walls.
It involves a vicious circle of transmural infection and inflammation with mediator release. Caused by an infectious insult in combination with impairment of drainage, airway obstruction, and/or a defect in host defense. Can be focal (due to a Fb, broncholith, slow growing tumor) or diffuse. Shares many features with COPD. Widening of the bronchi, sputum overproduction, persistent or recurrent airflow limitations. Access to Abx has decreased the prevalence in developed countries. See Cystic Fibrosis |
ICD-9 Codes: 494 Bronchiectasis
Etiology: a localized, irreversible bronchial dilatation caused by a destructive inflammatory process involving the bronchial walls. 30% unknown (idiopathic), 35% pneumonia/ postinfectious, 5% granulomatous dz, 10% childhood illness (pertussis), 4% genetic/ congenital dz (CF, alpha-1 antitrypsin def, immotile cilia), 11% other (XRT, trauma, Fb, aspiration). Post infectious forms common (viral or bacterial). Many predisposing conditions that ultimately cause inflammation: infection, allergic bronchpulmonary aspergilosis, primary ciliary dyskinesia, immune deficiency, non-TB mycobacterial infections, inhalation injury, recurrent aspiration, allergic bronchopulmonary aspergillosis, Congenital (CF, Kartagener’s/ immotile cilia syndrome, alpha-1-antitrypsin def), post-airway obstruction (foreign body, stricture, neoplasia, external compression), bronchomalacia, TB, sarcoid, radiation, common variable immunodeficiency, yellow nail syndrome. More common in pt’s with hypogammaglobulinemia, AIDS, Young’s syndrome (similar to cystic fibrosis, but do not have increased sweat chloride values, pancreatic insufficiency, abnormal nasal potential differences, or the CF delta F508 mutation). Rheumatic diseases such as rheumatoid arthritis and Sjögren’s syndrome can be complicated by bronchiectasis
S/s: chronic cough (90%), daily sputum production (76%, foul smelling, occasionally blood tinged), dyspnea (72%), hemoptysis (56%), recurrent pleurisy (46%). Crackles (70%), rhonchi (44%), and wheezing (34%) and digital clubbing (3%). PFT’s show an obstructive impairment similar to COPD, but a very low FVC is also seen in advanced disease in which much of the lung has been destroyed.
CXR: tram tracking = parallel infiltrates or linear opacities in the orientation of bronchovascular markings, some in parallel with a thin line of lucency between.
High resolution CT (HRCT) of the chest: the defining test of bronchiectasis as has a sensitivity of 97%. Spiral volumetric CT is also reliable. See airway dilatation, which can be detected by the finding of parallel (tram) lines or end-on ring shadows. Lack of tapering of bronchi in combination with airway dilatation may be more specific than bronchial dilatation alone as some healthy individuals and pt’s with asthma may have small areas of bronchial dilatation. May also see bronchial wall thickening, airways with mucopurulent plugs or debris accompanied by post-obstructive air trapping (“tree-in-bud pattern”). Cysts off the bronchial wall are a feature of more destructive bronchiectasis. A central (perihilar) distribution is suggestive of allergic bronchopulmonary aspergillosis, predominant upper lobe distribution is characteristic of cystic fibrosis or one of its variants, and lower lobe involvement is typical of idiopathic bronchiectasis.
W/u: CBC, IgG, IgA, IgM, HRCT, spirometry or bronchodilator test. Consider RF, IgE, aspergillus precipitins (ABPA), IgG subclasses, alpha-1-antitrypsin level, sinus CT, sputum Cx (bacterial, fungal, mycobacterial), bronchoscopy with Bx (ciliary dyskinesia, focal obstruction, infection), sweat chloride test.
Tx: Adequate systemic hydration. Bronchodilators and inhaled steroids as in COPD, intermittent (rotating) Abx based on sputum and Cx findings (cover H flu & pseudomonas). Empirical oral antibiotic therapy for 10-14 days with amoxicillin or amoxicillin-clavulanate (500 mg q8 hrs), ampicillin or tetracycline (250-500 mg four times daily), or trimethoprim-sulfamethoxazole (160/800 mg every 12 hours) is reasonable therapy in an acute exacerbation if a specific bacterial pathogen cannot be isolated.
Acetylcysteine (20% solution) nebulized to thin the secretions may help on occasion. Chest physical therapy such as postural draining, mechanical clearance techniques using vests to shake the lungs or aerobic exercise for 35 min to keep HR >140.
• Tx with the inhaled corticosteroid fluticasone is an effective therapy for bronchiectasis, particularly disease complicated by Pseudomonas aeruginosa infection (Thorax 2005;60:239-243) (reduced exacerbation frequency & improvement in sputum volume).
• Adding inhaled tobramycin (300 in 5 mL BID) to a conventional course of oral ciprofloxacin (750mg BID) effectively treats Pseudomonas aeruginosa-induced bronchiectasis unrelated to cystic fibrosis according (Chest 2006;130:1503-1510).
• A RCT found that Azithromycin (250mg PO qd x 12 mo’s) given to adults with non-CR bronchiectasis lead to a lower rate of infectious exacerbations (0 vs 2) (JAMA 2013;309:1251-59)….this could result in a better quality of life and might influence survival, but the effects of Abx resistance need to be considered.
• Erythromycin ES 400mg BID gave a modest decrease in pulmonary exacerbations (incidence rate ratio of 0.57) but an increased rate of macrolide resistance (by 25%) (JAMA 2013;309:1260-67).
Mannitol (Bronchitol): a dry powder formulation of mannitol to facilitate mucus clearance in pt’s with CF and thos at risk for bronchiectasis. Orphan drug indication 2/05.
Aerosolized Ciprofloxacin: FDA approved orphan drug designation for the management of bronchiestasis (1/07) and cystic fibrosis (2/06). Designed to prolong the short-acting nature of ciprofloxacin and localize its activity to the lungs, the aerosolized formulation is intended to allow sufficient pulmonary exposure to treat these infections.
Consider a home percussion vest to help loosen airway secretions, reduce Abx use and hospitalization (www.theVest.com), Rx 30 min BID with each session divided into 10min intervals (10min @ 5-10 Hz, then 10min @ 10-15Hz, then 15-20Hz), 16 sizes, fitted by an RT, costs $3,000, Medicare covers.
Powered Percussor System (SmartVest Trimline): FDA approved in 12/05 for use in pt’s requiring percussive therapy to enhance mucus transport in cystic fibrosis, bronchiectasis, obstructive pulmonary conditions and other diseases such as multiple sclerosis and muscular dystrophy. Consists of a portable generator that produces oscillating pressurized air pulses that are delivered through a hose to an inflatable vest, causing it to rapidly inflate and deflate against the pt’s chest wall to mobilize bronchial secretions. (Bronchiectasis. NEJM 2002;346:18)
Noncystic fibrosis bronchiectasis: a highly debilitating chronic condition that results in a progressive decline in lung function. Patients experience inflammation of the airways caused by neutrophil invasion, chronic bacterial infection, recurrent pulmonary exacerbations, and a productive cough.
• Azithromycin is a new option for the prevention of exacerbations in patients with noncystic fibrosis bronchiectasis as the risk for an exacerbation was halved with azithromycin (31% Vs 66% of the placebo group reported at least 1 exacerbation during the treatment period) (Lancet. 2012;380:627-629, 660-667).
An easy-to-use 7-point scale to evaluate disease severity in patients with noncystic fibrosis bronchiectasis has been developed (European Respiratory Society (ERS) 2012 Annual Congress: Abstract LBA 2811. Presented September 3, 2012)….dubbed the FACED score, using the relative weight of 5 variables associated with the 5-year all-cause mortality of bronchiectasis: lung function, age, radiologic extension, microbiologic data, and symptoms.
– In assessing lung function, postbronchodilation forced expiration volume in 1 s (FEV1) below 50% is assigned 0 points and an FEV1 above 50% is assigned 2 points. FEV1 had an odds ratio [OR] of 5.2 (95% confidence interval [CI], 2.8 to 9.8).
– In assessing age, patients 70 years and younger are assigned 0 points and those older than 70 years are assigned 2 points (OR, 4.9; 95% CI, 2.7 to 9.3).
– In assessing radiologic extension (OR, 1.9; 95% CI, 1.1 to 3.5), the involvement of only 1 lobe is assigned 1 point and the involvement of 2 or more lobes is assigned 2 points.
– In assessing microbiologic data, the absence of Pseudomonas aeruginosa colonization (OR, 2.4; 95% CI, 1.3 to 4.6) is assigned 0 points and the presence is assigned 1 point.
– In assessing symptoms (OR, 2.8; 95% CI, 1.5 to 5.2), the absence of dyspnea is assigned 0 points and the presence is assigned 1 point.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








