Fig. 13.1
Artist generated drawing of patient in position for breast ultrasound
Many benign and malignant lesions can be visualized by ultrasound. The differentiation is made by utilizing several criteria.
Margin Analysis
Smooth, sharp margins are more likely to represent a benign finding while irregular, poorly defined margins are more suspicious.
Echogenicity
Anechoic or the complete absence of echoes represents fluid as would be found in a benign breast cyst. Uniform internal echoes represent a solid lesion but are more likely to be benign while very mixed echo patterns are more likely to be malignant.
Acoustic Shadow
The shadow cast may be enhanced, decreased, or unchanged. Benign cysts and fibroadenomas have posterior enhancement while carcinomas often have posterior shadowing. Unchanged patterns are indeterminate.
Growth Pattern
Horizontal growth with a wider than tall pattern is often benign while vertical growth with a taller than wide pattern is often malignant.
Compressibility
Carcinomas are usually hard and resist compression while cysts containing fluid may be compressed. Therefore, varying the pressure on the transducer indicates compressibility and aids in evaluation.
Lymph Nodes
Lymph nodes may be axillary or intramammary, and when benign usually have a distinct image with sharp margins, fatty hilum, side notch, and thin cortex.
After carefully reviewing the ultrasound images and correlating with patient history, clinical breast exam, and other images, a clinical diagnosis is made and a course of management discussed with the patient. Be careful to strictly adhere to criteria for benign lesions. Failure to meet all the criteria may mask a carcinoma. Benign conditions can be followed while indeterminate findings should be aspirated or biopsied. Abscesses may be aspirated, irrigated, and cultures obtained. Suspicious lesions can be evaluated either by FNA, large core, or vacuum-assisted large core biopsy with the guidance of the ultrasound in a minimally invasive manner. This may occur immediately following the diagnostic ultrasound obviating the need to set up a separate time for the procedure.
US Images
(Figs. 13.2–13.7).
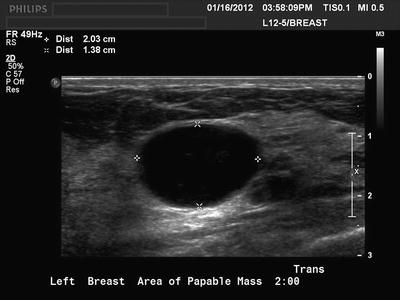


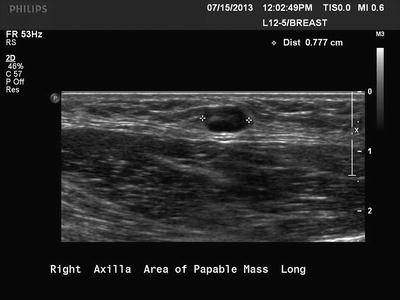


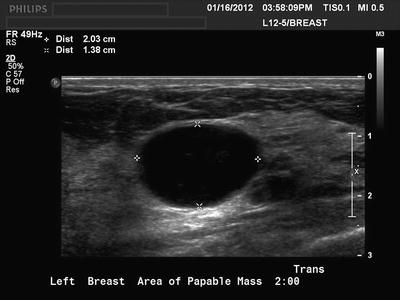
Fig. 13.2
Typical breast cyst with sharp margins, posterior enhancement, horizontal growth pattern, and absence of internal echoes

Fig. 13.3
Indeterminate lesion with partially sharp margins, horizontal growth pattern, internal echoes, and absence of posterior enhancement. This lesion was a benign fibroadenoma on core needle biopsy

Fig. 13.4
Suspicious lesion with sharp margins, vertical growth pattern, internal echoes, and absence of posterior enhancement. This lesion was a carcinoma on core needle biopsy
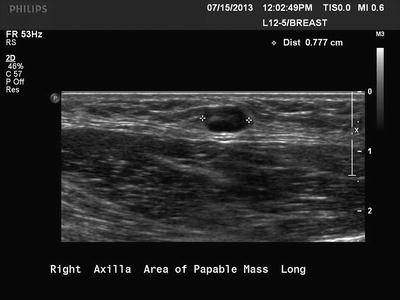
Fig. 13.5
Axillary lymph node with sharp margins, horizontal growth pattern, central hilum, and posterior enhancement

Fig. 13.6
Color Doppler visualizes blood flow in hilum and confirms lymph node

Fig. 13.7
Breast abscess
Breast Intervention
The patient is identified, documented, coagulation status reviewed, and consent obtained. The patient is positioned as in diagnostic ultrasound. The lesion is imaged and a path shortest from skin to spot is chosen. In preoperative wire localization, the wire location can be planned to be placed in a site that allows for optimal surgical incision. The breast is scrubbed with an antiseptic and local anesthetic placed in the skin immediately adjacent to the probe and along the path to the lesion. Remember the ultrasound beam is linear and the needle must be kept parallel to the beam. Placing the index finger of your nondominate hand on the probe in the direction of the ultrasound while your dominate hand guides the needle will help the needle stay parallel. Stabilizing the lesion with the transducer or by your ultrasound technologist can help keep the area taut so the breast tissue does not move during needle placement. During procedures if the transducer is held by an assistant, it will free both your hands for the procedure which will be advantageous. Carefully watch the needle tip to be certain that the target lesion does not move, and that needle does not inadvertently enter undesired nearby tissue such as chest wall or cavity. Gently wiggling the needle will often help you locate the needle tip on the screen and then be sure to keep the needle tip in sight while you advance the needle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








