CHAPTER 99
Boutonnière Finger
Presentation
After jamming the tip of a partially or fully extended finger (resulting in hyperflexion of the proximal interphalangeal [PIP] joint) or with direct trauma over the joint, the patient develops a painful, swollen PIP joint. These injuries are seen in basketball players and martial artists, who use open-hand blocking techniques, as well as when an athlete’s hand is stepped on. Tenderness is greatest over the dorsum of the base of the middle phalanx, and there is diminished extensor tendon strength with pain when the middle phalanx is extended against resistance. The classic boutonnière deformity is rarely present immediately after injury. Radiographs are usually normal.
What To Do:
 Obtain a detailed history of the mechanism of injury.
Obtain a detailed history of the mechanism of injury.
 Perform a complete examination, palpating for point tenderness of the dorsum of the joint, the collateral ligaments, and the volar plate. Test for joint stability in all directions, test sensation, and check for injuries proximal and distal to the PIP joint.
Perform a complete examination, palpating for point tenderness of the dorsum of the joint, the collateral ligaments, and the volar plate. Test for joint stability in all directions, test sensation, and check for injuries proximal and distal to the PIP joint.
 Check for a possible tear of the central slip of the extensor digitorum communis tendon. With the patient’s PIP joint flexed at 90 degrees over a straight edge (such as a countertop), apply resistance to active extension over the middle phalanx. If the central slip is disrupted, the patient will not be able to apply pressure against resistance (Figure 99-1, A to C). It is possible for the patient to extend the injured finger without resistance using the lateral bands of the extensor tendon, causing the distal phalanx to hyperextend. Full passive extension is easily obtained. The distal interphalangeal (DIP) joint is in slight hyperextension at rest.
Check for a possible tear of the central slip of the extensor digitorum communis tendon. With the patient’s PIP joint flexed at 90 degrees over a straight edge (such as a countertop), apply resistance to active extension over the middle phalanx. If the central slip is disrupted, the patient will not be able to apply pressure against resistance (Figure 99-1, A to C). It is possible for the patient to extend the injured finger without resistance using the lateral bands of the extensor tendon, causing the distal phalanx to hyperextend. Full passive extension is easily obtained. The distal interphalangeal (DIP) joint is in slight hyperextension at rest.
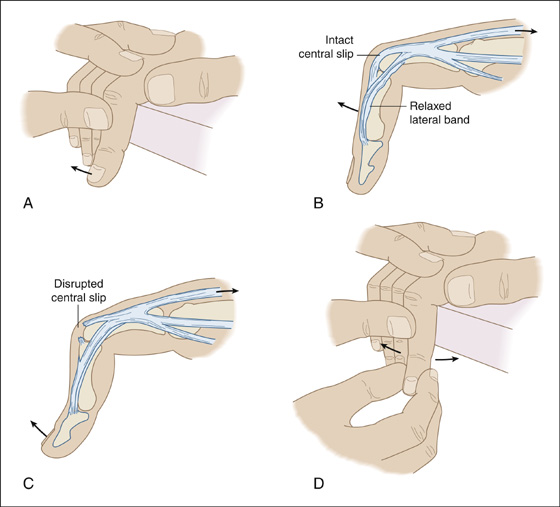
Figure 99-1 Extension against resistance tests for a central slip avulsion (A to C). Varus and valgus stress at the PIP joint tests for collateral ligament instability (D).
 When available, diagnostic high-frequency ultrasonography is a very accurate noninvasive study that can identify central slip injuries in the extensor mechanism of the finger. This can confirm the diagnosis and either allow early initiation of splinting or eliminate the need for prolonged splinting.
When available, diagnostic high-frequency ultrasonography is a very accurate noninvasive study that can identify central slip injuries in the extensor mechanism of the finger. This can confirm the diagnosis and either allow early initiation of splinting or eliminate the need for prolonged splinting.
 Test for collateral ligament stability with varus and valgus stress (Figure 99-1, D).
Test for collateral ligament stability with varus and valgus stress (Figure 99-1, D).
 If avulsion of the central slip of the extensor tendon is suspected, splint the PIP joint in extension. The splint should leave the DIP and metacarpophalangeal (MCP) joints completely mobile, or the collateral ligaments will contract. Active DIP flexion should be encouraged. This action pulls the PIP extensor hood mechanism distally, thereby further approximating the two ends of the ruptured central slip. The PIP joint should remain constantly splinted for 6 to 8 weeks—3 to 4 weeks of static extension splinting (Figure 99-2), followed by 2 to 3 weeks of dynamic extension splinting. Occasionally, it should be splinted for another 8 to 10 weeks, whenever the patient engages in any activity that is likely to cause reinjury.
If avulsion of the central slip of the extensor tendon is suspected, splint the PIP joint in extension. The splint should leave the DIP and metacarpophalangeal (MCP) joints completely mobile, or the collateral ligaments will contract. Active DIP flexion should be encouraged. This action pulls the PIP extensor hood mechanism distally, thereby further approximating the two ends of the ruptured central slip. The PIP joint should remain constantly splinted for 6 to 8 weeks—3 to 4 weeks of static extension splinting (Figure 99-2), followed by 2 to 3 weeks of dynamic extension splinting. Occasionally, it should be splinted for another 8 to 10 weeks, whenever the patient engages in any activity that is likely to cause reinjury.
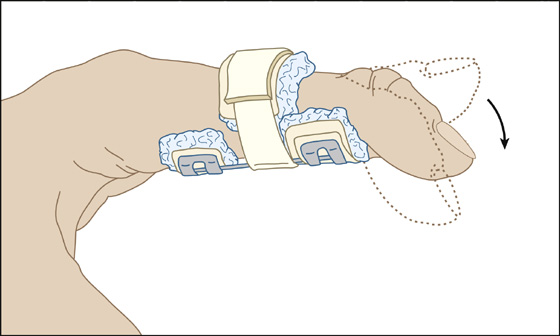
Figure 99-2 Suspected avulsion of the central slip of the extensor tendon necessitates splinting of the PIP joint in extension, while allowing the DIP joint to go through a full range of motion. (Adapted from Ruiz E, Cicero JJ: Emergency management of skeletal injuries. St Louis, 1995, Mosby.)
 Prompt referral should be made to a hand surgeon to evaluate for potential acute operative repair.
Prompt referral should be made to a hand surgeon to evaluate for potential acute operative repair.
 Provide standard acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) along with initial cold compresses and elevation.
Provide standard acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) along with initial cold compresses and elevation.
What Not To Do:
 Do not assume that posttraumatic swelling of a PIP joint represents a simple sprain until testing for extension against resistance.
Do not assume that posttraumatic swelling of a PIP joint represents a simple sprain until testing for extension against resistance.
 Do not overlook associated injuries that may cause joint instability. Such injuries may require immediate orthopedic consultation.
Do not overlook associated injuries that may cause joint instability. Such injuries may require immediate orthopedic consultation.
 Do not be fooled by the patient’s ability to actively extend the PIP joint. In the acute setting, the patient may be able to fully extend through the action of the lateral bands, despite a complete rupture of the central slip.
Do not be fooled by the patient’s ability to actively extend the PIP joint. In the acute setting, the patient may be able to fully extend through the action of the lateral bands, despite a complete rupture of the central slip.
Discussion
The boutonnière (buttonhole) injury or deformity refers to a rupture of the central slip of the extensor tendon at the PIP joint. Similar to the mechanism of injury in mallet finger, there is forced PIP flexion at the same time the PIP joint is held rigidly in extension.
Although the acute manifestations of a disrupted central slip may be limited to swelling and tenderness over the PIP joint, with time the central slip retracts. The lateral bands will slip and displace volarly, becoming flexors of the PIP joint and allowing the joint to herniate dorsally through the defect in the tendon (like a button through a buttonhole), thereby creating a flexed PIP joint. Eventually, a position of flexion at the PIP joint and hyperextension at the DIP joint become fixed, producing the classic buttonhole or boutonnière deformity (Figure 99-3).
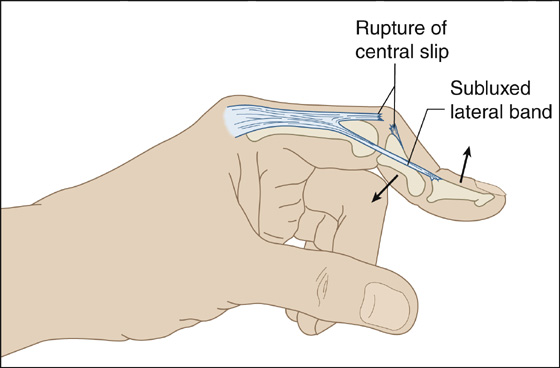
Figure 99-3 Boutonnière deformity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


