Board Simulation: Endocrinology
Elumalai Appachi
QUESTIONS
1. The parents of a 10-year-old girl (Fig. 20.1) are concerned about her height. She is shorter than her classmates, and the parents request growth hormone therapy. Which of the following statements is true regarding the diagnosis and management of her condition?
a) A skeletal survey is required to rule out hypochondroplasia.
b) Growth hormone therapy is indicated because she may have growth hormone deficiency.
c) The parents should be reassured that her growth will catch up during the adolescent growth spurt.
d) Chromosomal analysis will reveal the diagnosis.
e) None of the above.
View Answer
Answer
The answer is d. Most patients with Turner syndrome have a 45,X chromosome complement, although 15% display mosaicism (45,X/46,XX). This condition occurs in 1 of 1500 to 2500 liveborn female infants. Most pregnancies with a Turner syndrome karyotype abort spontaneously. The major clinical manifestations, commonly present at birth, include lymphedema of the dorsa of the hands and feet (see Fig. 20.1) and loose skin folds at the nape of the neck. In childhood, short stature, webbing of the neck, a broad chest, cubitus valgus, and extremely convex fingernails are the predominant features. Sexual maturation fails to occur at the expected age. Associated cardiac anomalies include bicuspid aortic valve, coarctation of aorta, aortic stenosis, and mitral valve prolapse. Renal anomalies include pelvic kidney, horseshoe kidney, absence of one kidney, and double collecting systems. Any short female child should be investigated for Turner syndrome. Although growth hormone deficiency has not been established in this syndrome, treatment with growth hormone helps to increase the child’s height. Hypochondroplasia resembles achondroplasia but is a milder disorder. Children with hypochondroplasia display a characteristic phenotype, and radiography is diagnostic.
2. A 2-week-old boy is seen in the emergency department because he has been vomiting for the past 24 hours. On examination, the infant is lethargic and his skin is mottled. He is given two boluses of normal saline solution with no improvement. The infant’s laboratory data include the following values:
a) Na = 121 mmol/L
b) K = 6.1 mmol/L
c) Blood urea nitrogen = 40 mg/dL
d) HCO3 = 12 mmol/L
e) Blood glucose = 40 mg/dL
Appropriate management would include all of the following except:
a) Administering intravenous hydrocortisone
b) Administering 2 to 4 mL/kg of 10% dextrose intravenously
c) Administering dopamine infusion
d) Measuring serum 17-hydroxyprogesterone
e) Administering broad-spectrum antibiotics
View Answer
Answer
The answer is c. Congenital adrenal hyperplasia is an autosomal-recessive disorder. Ninety percent of affected patients have 21-hydroxylase deficiency. Patients with the salt-wasting variety of congenital adrenal hyperplasia present with failure to thrive, dehydration, vomiting, and anorexia. In female infants, virilization of the external genitalia leads to an early diagnosis; the condition is often diagnosed later in male infants with the salt-wasting variety (2-3 weeks of life) because the external genitalia may appear normal. Hydrocortisone (10-20 mg/m2 every 24 hours) is recommended as a replacement therapy and to prevent virilization. Sodium supplementation and the administration of mineralocorticoid are
necessary to maintain a normal electrolyte balance. The infant in question requires another normal saline bolus and the administration of hydrocortisone; dopamine is not indicated.
necessary to maintain a normal electrolyte balance. The infant in question requires another normal saline bolus and the administration of hydrocortisone; dopamine is not indicated.
 Figure 20.1 The girl in question 1. See explanation for question 1 for details. |
3. An 8-year-old girl with insulin-dependent diabetes presents with a 3-day history of abdominal pain and vomiting. She was treated in the emergency department 1 week ago for hypoglycemia. Examination reveals rapid breathing, dry mucous membranes, and poor peripheral perfusion. Appropriate management would include all of the following except:
a) Initiating fluid resuscitation judiciously, with close monitoring of the neurologic status
b) Monitoring serum potassium frequently
c) Remembering that sodium bicarbonate therapy is not routinely indicated and may cause intracellular acidosis
d) Administering 0.1 U/kg of regular insulin subcutaneously
e) Advising her to rotate the sites of insulin injection at the time of discharge
View Answer
Answer
The answer is d. The administration of fluid and electrolytes to replete the intravascular volume and correct electrolyte abnormalities is the most important step in the management of diabetic ketoacidosis. Insulin therapy helps arrest the metabolic derangement and reverses the catabolic state. Intravenous, rather than subcutaneous, infusion of insulin is the standard of care for diabetic ketoacidosis. Because diabetic ketoacidosis causes hyperosmolar dehydration, the administration of 0.9% saline solution is hypotonic, relative to the patient’s osmolality. A gentle and gradual decrease in osmolality is required to prevent the development of cerebral edema, one of the major complications of diabetic ketoacidosis therapy. The administration of a total fluid volume of 4 L/m2 per day is associated with a decreased incidence of cerebral edema. Because the total body potassium is depleted in diabetic ketoacidosis, potassium replacement must be started early in the therapy to avoid life-threatening hypokalemia. Bicarbonate therapy is not routinely recommended during the management of diabetic ketoacidosis because it causes alkalosis, which in turn shifts the oxygen dissociation curve to the left and reduces oxygen delivery to tissues. It also causes intracellular acidosis with the production of carbon dioxide, which diffuses across the blood-brain barrier and exacerbates the cerebral acidosis. The patient in question should rotate the insulin injection sites because her erratic insulin absorption is contributing to the episodes of hypoglycemia and hyperglycemia.
4. The parents of a 2-year-old girl who was brought into your clinic express concern about the development of pubic hair in the child. Appropriate management should include:
a) Measurement of her bone age
b) Reassurance of the parents that the condition is probably benign but should be followed up closely
c) Measurement of serum androgens and 17-hydroxyprogesterone
d) All of the above
e) None of the above
View Answer
Answer
The answer is d. Precocious puberty is defined as the development of secondary sexual characteristics before the age of 8 years in girls and 9 years in boys. Premature adrenarche is the appearance of pubic hair before the age of sexual maturation. It is much more common in girls than in boys and is an early maturational event of adrenal androgen production. Premature adrenarche is a benign condition and does not require therapy. However, if the child shows evidence of a systemic androgen effect (e.g., acceleration of growth, clitoromegaly, advanced bone age, cystic acne), further investigations are warranted. The measurement of androgen and 17-hydroxyprogesterone is necessary to rule out nonclassic forms of congenital adrenal hyperplasia.
5. A 21-month-old toddler is brought to you for a routine physical examination. You note that she has recently gained an excessive amount of weight. Examination shows a markedly obese child with a blood pressure of 130/90 mm Hg. Urinalysis shows glycosuria. Which of the following is the best course of action?
a) Taking a detailed dietary history and advising the family about caloric restriction
b) Ordering an abdominal ultrasound as it is diagnostic
c) Measuring serum Cortisol in the morning and evening to evaluate diurnal rhythm
d) Administering insulin 0.1 U/kg subcutaneously
e) Measuring urinary excretion of free Cortisol
View Answer
Answer
The answer is e. The features of Cushing syndrome, which result from adrenal cortical hyperfunction, are
obesity, hypertension, and glucose intolerance. The most common cause of Cushing syndrome in infants is a malignant, functioning adrenocortical tumor. Most of the tumors occur in children younger than 3 years. Other causes of Cushing syndrome in childhood include primary pigmented nodular adrenocortical disease and nodular hyperplasia, both of which are independent of adrenocorticotropic hormone (ACTH) secretion. ACTHdependent Cushing syndrome is caused by microadenomas of the pituitary and the ectopic production of ACTH in islet cell carcinoma of the pancreas, neuroblastoma, and occasionally Wilms tumor. The clinical manifestations of Cushing syndrome include obesity, masculinization, hypertrichosis, acne, and impaired growth. The diurnal variation of cortisol production is lost in Cushing syndrome, but diurnal variation is lacking in children younger than 3 years. The urinary excretion of cortisol is almost always increased. Ultrasonography may not be able to identify the tumors, and CT scan is required to make the diagnosis. Other findings include polycythemia, lymphopenia and eosinopenia, altered glucose tolerance, advanced bone age, pathologic fracture, and absence of the thymic shadow on chest x-ray films.
obesity, hypertension, and glucose intolerance. The most common cause of Cushing syndrome in infants is a malignant, functioning adrenocortical tumor. Most of the tumors occur in children younger than 3 years. Other causes of Cushing syndrome in childhood include primary pigmented nodular adrenocortical disease and nodular hyperplasia, both of which are independent of adrenocorticotropic hormone (ACTH) secretion. ACTHdependent Cushing syndrome is caused by microadenomas of the pituitary and the ectopic production of ACTH in islet cell carcinoma of the pancreas, neuroblastoma, and occasionally Wilms tumor. The clinical manifestations of Cushing syndrome include obesity, masculinization, hypertrichosis, acne, and impaired growth. The diurnal variation of cortisol production is lost in Cushing syndrome, but diurnal variation is lacking in children younger than 3 years. The urinary excretion of cortisol is almost always increased. Ultrasonography may not be able to identify the tumors, and CT scan is required to make the diagnosis. Other findings include polycythemia, lymphopenia and eosinopenia, altered glucose tolerance, advanced bone age, pathologic fracture, and absence of the thymic shadow on chest x-ray films.
6. A 16-year-old adolescent (Fig. 20.2) is losing weight despite having a good appetite. She is a long-distance runner at school and seems to tire easily. She exhibits emotional lability, and her grades at school have suffered lately. The most appropriate plan of action is to:
a) Order thyroid function tests.
b) Refer her for a psychiatric evaluation.
c) Commence a workup for inflammatory bowel disease.
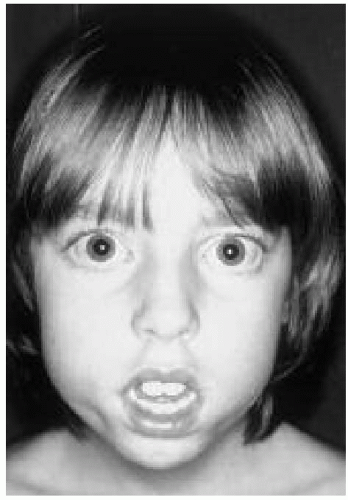 Figure 20.2 The adolescent in question 6. See explanation for question 6 for details.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|


