Figure 77-1 Blunt injury to the scrotum.
What To Do:
 Get a clear history of the exact mechanism, the force of the trauma, and the point of maximum impact. Determine if there was any bloody penile discharge or hematuria and whether or not the patient has any preexisting genital disease, such as previous genitourinary surgery, infection, or mass.
Get a clear history of the exact mechanism, the force of the trauma, and the point of maximum impact. Determine if there was any bloody penile discharge or hematuria and whether or not the patient has any preexisting genital disease, such as previous genitourinary surgery, infection, or mass.
 Gently examine the external genitalia with the understanding that intense pain may result in a suboptimal examination. If scrotal swelling is not too severe, try to palpate and assess the intrascrotal anatomy.
Gently examine the external genitalia with the understanding that intense pain may result in a suboptimal examination. If scrotal swelling is not too severe, try to palpate and assess the intrascrotal anatomy.
 When there is minimal pain and tenderness, with normal anatomy, no further evaluation is necessary.
When there is minimal pain and tenderness, with normal anatomy, no further evaluation is necessary.
 There is a high risk for urethral injury in straddle injuries. Obtain a urinalysis. If blood is present in the urine (or at the urethral meatus), perform a retrograde urethrogram and obtain urologic consultation.
There is a high risk for urethral injury in straddle injuries. Obtain a urinalysis. If blood is present in the urine (or at the urethral meatus), perform a retrograde urethrogram and obtain urologic consultation.
 After any significant blunt trauma, when pain or swelling prevents demonstration of normal intrascrotal anatomy, obtain a testicular color Doppler ultrasonograph to help determine the need for urologic consultation and operative intervention.
After any significant blunt trauma, when pain or swelling prevents demonstration of normal intrascrotal anatomy, obtain a testicular color Doppler ultrasonograph to help determine the need for urologic consultation and operative intervention.
 Hematomas can involve the testis, epididymis, or scrotal wall. Patients with intratesticular hematomas fare poorly without exploration. Forty percent of these hematomas result in testicular infection or necrosis, which often requires orchiectomy. Scrotal exploration is warranted if there is compelling evidence of testicular fracture or rupture on scrotal sonography or physical examination. It is most appropriate to explore a grossly abnormal scrotum without ultrasonography when the index of suspicion is high. This should occur when there is a clinical hematocele. This may be evidenced by persistent moderate to severe pain, tender ecchymotic fullness of the scrotal sac, and a testicle that feels enlarged and/or irregular or is difficult to palpate. The presence of a large hematocele on ultrasonography is another indication for exploration.
Hematomas can involve the testis, epididymis, or scrotal wall. Patients with intratesticular hematomas fare poorly without exploration. Forty percent of these hematomas result in testicular infection or necrosis, which often requires orchiectomy. Scrotal exploration is warranted if there is compelling evidence of testicular fracture or rupture on scrotal sonography or physical examination. It is most appropriate to explore a grossly abnormal scrotum without ultrasonography when the index of suspicion is high. This should occur when there is a clinical hematocele. This may be evidenced by persistent moderate to severe pain, tender ecchymotic fullness of the scrotal sac, and a testicle that feels enlarged and/or irregular or is difficult to palpate. The presence of a large hematocele on ultrasonography is another indication for exploration.
 Small hematoceles, epididymal hematomas, or contusions of the testis generally pose little risk to the patient and do not require surgical exploration.
Small hematoceles, epididymal hematomas, or contusions of the testis generally pose little risk to the patient and do not require surgical exploration.
 All posttraumatic lesions should be followed to demonstrate sonographic resolution, because 10% to 15% of testicular tumors first present after an episode of scrotal trauma.
All posttraumatic lesions should be followed to demonstrate sonographic resolution, because 10% to 15% of testicular tumors first present after an episode of scrotal trauma.
 Simple scrotal lacerations can be closed using Vicryl absorbable suture or tissue adhesive (Dermabond).
Simple scrotal lacerations can be closed using Vicryl absorbable suture or tissue adhesive (Dermabond).
 When emergent urologic intervention is not required, provide analgesia (consider nonsteroidal anti-inflammatory drugs [NSAIDs], bed rest, scrotal support, a cold pack, and urologic follow-up [Figure 77-2]).
When emergent urologic intervention is not required, provide analgesia (consider nonsteroidal anti-inflammatory drugs [NSAIDs], bed rest, scrotal support, a cold pack, and urologic follow-up [Figure 77-2]).
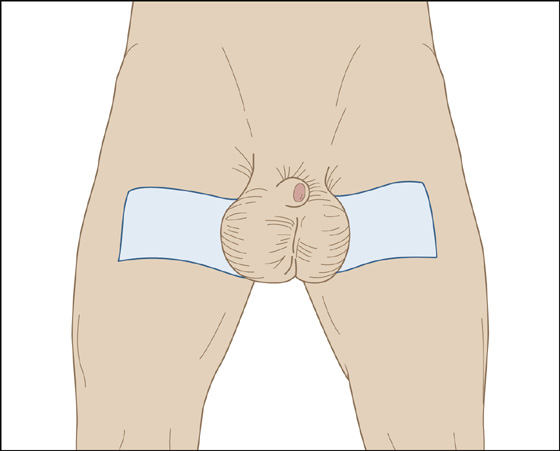
Figure 77-2 Scrotal support.
 Patients should always be instructed to return immediately if pain increases, becomes severe, or is accompanied by vomiting or lightheadedness.
Patients should always be instructed to return immediately if pain increases, becomes severe, or is accompanied by vomiting or lightheadedness.
What Not To Do:
 Do not miss testicular torsion, which is associated with minor to moderate blunt trauma approximately 20% of the time. (See symptoms and signs of testicular torsion in Chapter 79.)
Do not miss testicular torsion, which is associated with minor to moderate blunt trauma approximately 20% of the time. (See symptoms and signs of testicular torsion in Chapter 79.)
 Do not miss the rare traumatic testicular dislocation that results in an “empty scrotum.” The testis is found superficially beneath the abdominal wall in approximately 80% of such cases. Immediate urology consultation is required.
Do not miss the rare traumatic testicular dislocation that results in an “empty scrotum.” The testis is found superficially beneath the abdominal wall in approximately 80% of such cases. Immediate urology consultation is required.
 Do not discharge a patient until he can demonstrate the ability to urinate.
Do not discharge a patient until he can demonstrate the ability to urinate.
Discussion
Blunt testicular trauma occurs from a direct blow to the testes with impingement against the symphysis pubis or ischial ramus. Trauma can result in contusion, hematoma, fracture, rupture, or, rarely, dislocation of the testis. Testicular rupture is a surgical emergency. More than 80% of ruptured testes can be saved if surgery is performed within 72 hours of injury. Complications of testicular trauma include testicular atrophy, infection, infarction, and infertility, which are much more likely with nonoperative management of serious injuries.
If Doppler studies demonstrate a serious injury, early exploration, evacuation of hematoma, and repair of testicular rupture tend to result in an earlier return to normal activity, with less risk for testicular atrophy, infection, infarction, and infertility.
Sonographic findings in testicular rupture include interruption of the tunica albuginea; contour abnormality; a heterogeneous testis with irregular, poorly defined borders; scrotal wall thickening; and a large hematocele. The sonographic appearance of hematomas varies with time. Acute hematomas appear hyperechoic and subsequently become complex, with cystic components. Color Doppler sonography in posttraumatic patients may reveal focal or diffuse hyperemia of the epididymis, which represents traumatic epididymitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


