FIGURE 1 Schematic drawing showing the innervation of the pelvic floor in males. Although this diagram attempts to show the innervation in humans, much of the anatomic information is derived from animal data. CEL, celiac plexus; DRG, dorsal root ganglion; HGP, hypogastric plexus; IHP, inferior hypogastric plexus; ISP, inferior spermatic plexus; PSN, pelvic splanchnic nerve; PUD, pudendal nerve; Epid., epididymis; SA, short adrenergic projections; SAC, sacral plexus; SCG, sympathetic chain ganglion; SHP, superior hypogastric plexus; SSP, superior spermatic plexus. (From: Wesselmann U, Burnett AL, Heinberg LJ. The urogenital and rectal pain syndromes. Pain 1997; 73: 269–294 [ref. 60]. This figure has been reproduced with permission of the International Association for the Study of Pain® (IASP). This figure may not be reproduced for any other purpose without permission.)
Somatic efferent and afferent innervation to the urogenital floor originates from sacral spinal cord levels S2 to S4. Sacral nerve roots emerge from the spinal cord to form the sacral plexus, and give rise to the pudendal nerve. The pudendal nerve also receives postganglionic axons from the caudal sympathetic chain ganglia. Thus the pudendal nerve carries somatic and autonomic nerve fibers. The pudendal nerve runs medial to the internal pudendal vessels along the lateral wall of the ischiorectal fossa dorsal to the sacrospinous ligament. First a branch splits off to become the dorsal nerve of the penis (or clitoris), then the remaining pudendal nerve fibers distribute a medial branch to the anal canal, dorsal branches to the urethral sphincter, and dorsolateral branches to the anterior perineal musculature. The posterior perineal musculature is supplied by nerves originating predominantly from sacral level S4. Branches of the S4–5 nerve roots form the coccygeal plexus, distributing fibers to the perineal, perianal, and scrotal (labial) skin.
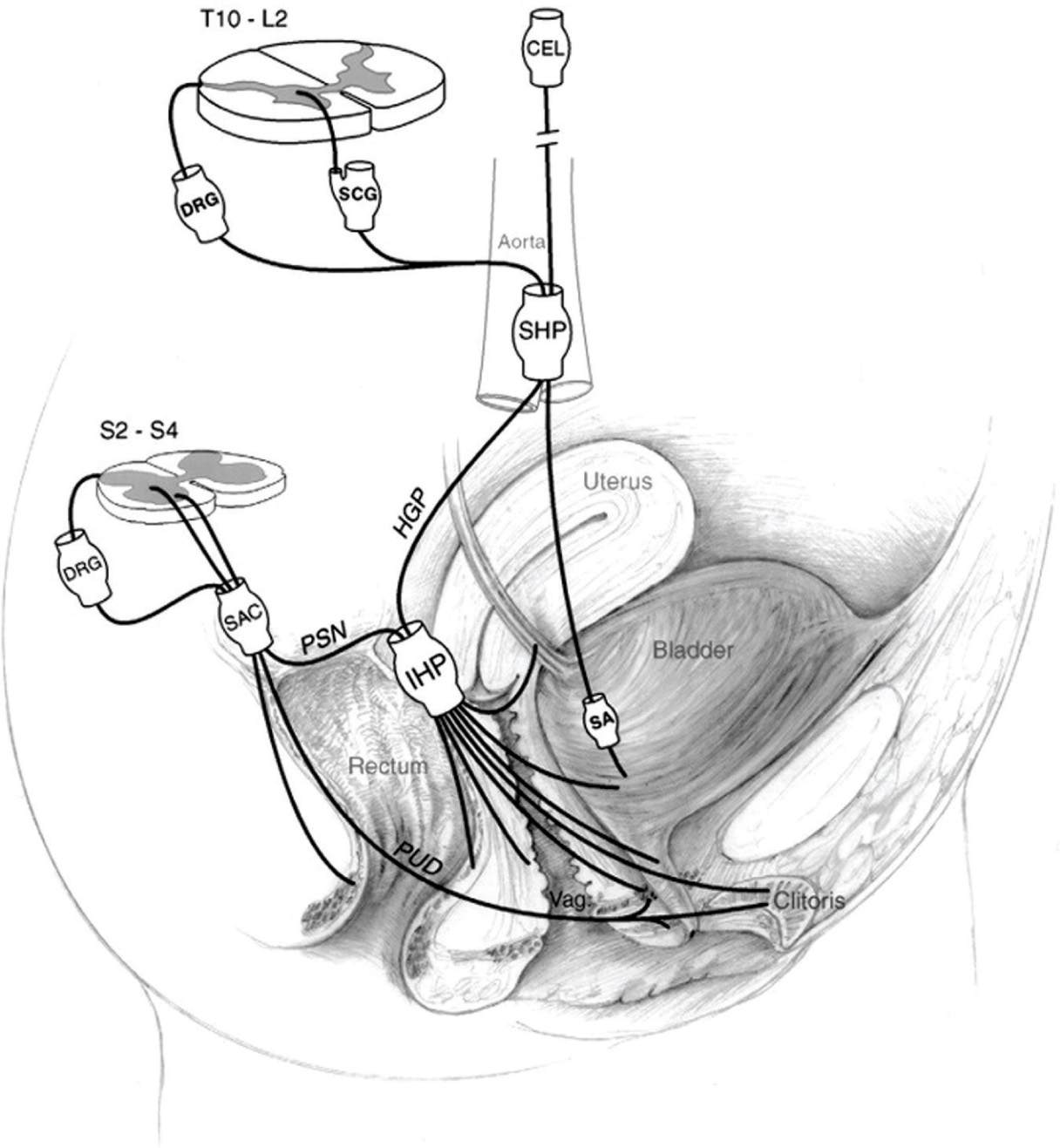
FIGURE 2 Schematic drawing showing the innervation of the pelvic floor in females. Although this diagram attempts to show the innervation in humans, much of the anatomic information is derived from animal data. CEL, celiac plexus; DRG, dorsal root ganglion; HGP, hypogastric plexus; IHP, inferior hypogastric plexus; PSN, pelvic splanchnic nerve; PUD, pudendal nerve; SA, short adrenergic projections; SAC, sacral plexus; SCG, sympathetic chain ganglion; SHP, superior hypogastric plexus; Vag., vagina (From: Wesselmann U, Burnett AL, Heinberg LJ. The urogenital and rectal pain syndromes. Pain 1997; 73: 269–294 [ref. 60]. This figure has been reproduced with permission of the International Association for the Study of Pain® (IASP). This figure may not be reproduced for any other purpose without permission.)
Etiologies and Pathophysiological Mechanisms
At present there is no universally accepted etiology for BPS/IC and proposed etiologies, which are not mutually exclusive include inflammation, mast cell activation, urothelial dysfunction/glycosaminoglycan defects, presence of anti-proliferative factor, autoimmune mechanisms, genetic predisposition and early-in-life experiences [47,49]. As it is increasingly being recognized that BPS/IC shares many aspects with other chronic pain syndromes, neurophysiological mechanisms including peripheral and central sensitization have been explored. These multiple etiologies reflect the heterogeneity of the patient population.
In BPS/IC multiple pain sites are common. Warren et al. [55] explored whether a careful and systematic description of pain of BPS/IC might provide insights to the pathogenesis of the disease. It has been questioned if indeed the generator of pain in BPS/IC is the bladder [55]. The suprapubic site is the usual area of normal bladder filling sensation. This site is the most common pain site in subjects with BPS/IC [20,55]. The best recognized stimulus of visceral pain is distension of a hollow organ [32]. Of patients with BPS/IC, 84% to 90% report worsening of pain with bladder filling, which suggests that the bladder is a visceral organ involved in BPS/IC [51]. These findings might imply that the bladder is in fact the generator of pain in BPS/IC. This is a hypothesis, which was tested by Warren et al. [55]. Clinical observations have documented that in BPS/IC multiple pain sites are common and consistent with these observations, BPS/IC patients in this epidemiological study reported multiple pains. Pain could be consolidated at 4 sites including, suprapubic, urethral, genital and non-genitourinary. The data demonstrated that suprapubic prominence and changes in the voiding cycle are features consistent with BPS/IC, but do not prove that the bladder is the pain generator in BPS/IC and that the pain sites described by patients are referred from it. Women, who in other contexts might have been diagnosed with urethral pain syndrome or vulval pain syndrome, did not differ in pertinent variables from women, who had BPS/IC without pain at these sites.
Early histological examinations of bladder lesions of patients diagnosed with BPS/IC revealed mucosal ulceration, pancystitis and perineural inflammatory infiltrates. However a search for a chronic viral or bacterial etiology rendered negative results [1,19], including a search for bacterial and viral DNA in bladder biopsies from patients with BPS/IC. The surface of the bladder urothelium is lined by a glycosaminoglycan layer and a defect in this protective layer has been proposed to cause the symptoms of BPS/IC, but the etiology of this breakdown in the urothelial barrier and its consequences for the clinical features of BPS/IC are still an issue for debate [47,49]. Morphological studies have demonstrated mast cell proliferation and activation in patients with BPS/IC [43]. Many symptoms such as pain, frequency, edema and ulcerations could possibly be related to mast cell release, and targeted pharmacotherapy to inhibit mast cell activation has been suggested as a therapeutic avenue [43].
Several groups have tried to identify biomarkers to identify patients with BPS/IC and to predict treatment responses. An antiproliferative factor (APF) that profoundly inhibits bladder cell proliferation has been identified in the urine of patients with BPS/IC [28]. It has been proposed that in patients with BPS/IC this peptide inhibits bladder epithelial regeneration following damage, such as that caused by bacterial cystitis [27]. A mouse model of BPS/IC based on AFP inhibition of bladder epithelial repair has been developed recently [26]. Urinary nerve growth factor (NGF) has been reported to be increased in patients with BPS/IC and a decrease in urinary NGF levels was associated with greater pain reduction after treatment, suggesting that urinary NGF levels might be a useful biomarker to detect the severity of the disease in patients with BPS/IC [31].
Numerous receptors have been shown to be increased in bladder tissue of patients with BPS/IC using immunohistochemical staining, including cannabinoid receptor-1, transient receptor potential vanilloid receptor subtype-1, and TRPM8 [33,34,35]. It has been suggested that these receptors might play a role in the pathophysiology of BPS/IC and may provide targets for pharmacological therapy [6]. Molecular studies have recently demonstrated that microRNAs may mediate the down-regulation of neurokinin-1 receptor in BPS/IC [42].
A genetic predisposition to some sub-groups of BPS/IC has been explored. Warren et al. [54] reported that adult female first relatives of patients with BPS/IC may have a prevalence of BPS/IC 17 times that found in the general population. This suggests, but does not prove, a genetic susceptibility of BPS/IC.
It has been observed that anxiety and stress may initiate and worsen urinary symptoms in BPS/IC. Life stress is associated with greater BPS/IC symptoms [41] and stress-related mechanisms can be associated with inflammatory processes within the bladder that sometimes accompany BPS/IC [43].
Psychophysical studies, using a similar approach as in patients with neuropathic pain, have confirmed hypersensitivity to somatic stimuli in patients with BPS/IC [21,30,37]. Consistent with findings in patients with fibromyalgia and IBS, conditioned pain modulation responses were significantly different in patients with BPS/IC compared to healthy controls, indicating that a deficit in endogenous pain inhibitory systems may contribute to BPS/IC [36]. f-MRI imaging studies in women with BPS/IC have demonstrated that these patients present with a sensorimotor component to their pathology involving an alteration in the intrinsic oscillations and connectivity within a cortico-cerebellar network previously associated urinary bladder function [29].
Numerous animal models have been established of bladder pain [summarized in detail in: reference 23], which have employed mechanical stimulation, chemical and infectious agents, as well as specific etiologic factors, such as stress. These models are sometimes used to explore specific etiological aspects of BPS/IC and possible therapies. Rodent models have used overdistension of the urinary bladder, inflammation with intravesical instillation of agents producing both direct signs of visceral pain perception (abnormal behavior) and referred hyperalgesia. Cyclophosphamide-induced cystitis in rats follows administration of the drug intraperitoneally, mimicking the equivalent human condition of cyclophosphamide-induced cystitis, rather than BPS/IC. However, this rodent model has also been used to understand neurophysiological aspects of bladder pain relevant to BPS/IC and to study potential treatments. The advantage of the cyclophosphamide-induced cystitis bladder pain model in mice has allowed genetic studies to be undertaken. Mice that lack the receptor for substance P (NK1) did not develop either primary hyperalgesia after bladder inflammation or referred hyperalgesia. Neonatal bladder inflammation, similar to animal studies modelling other pain syndromes, produces bladder hypersensitivity in adulthood. It is thus proposed that this model may be useful to study early-in-life experiences which might result in BPS/IC in adulthood. An animal model of stress-induced bladder mast cell activation in 1997 [44], has been used by as a model of interstitial cystitis. However, the behavioral aspects of this model, will have to be quantified with respect to pain [23]. A naturally occurring disease has been described in cats, which has many features of BPS/IC in humans [9]. This model has been proposed to study the effects of stressors on the severity of clinical signs as well as newly proposed therapies for BPS/IC patients [8,9].
Comorbid Conditions
Clinical observations suggest, that there is substantial overlap observed between BPS/IC and other pelvic/abdominal pain syndromes. These observations could be explained neurophysiologically by referred visceral pain mechanisms to other visceral and somatic areas with overlapping spinal cord projections (Figs. 1 and 2). In addition, in a report [15] for BPS/IC and fibromyalgia, there is increasing evidence of the co-occurrence of BPS/IC with chronic pain syndromes in other “non-pelvic” body areas, raising the question of systemic alterations of pain modulatory mechanisms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





