Biochemistry, Circannual and Circadian Rhythms, Endocrinology, and Immunology of Cluster Headaches
Elisabet Waldenlind
Gennaro Bussone
BIOCHEMISTRY
Histamine and Mast Cells
Horton (64) suggested that cluster headache (CH) was associated with an unusual histamine sensitivity. The histamine levels have been reported to be higher during attacks than between attacks in whole blood (3) but not in urine (136). Increased numbers of mast cells, the main source of histamine, have been found in skin biopsy specimens from the painful temporal region both during and between cluster periods (5,127), but also from the pain-free side compared with control individuals. The mast cells were typically localized perivascularly, but in CH they were also found near cutaneous nerves (94). Increased degranulation, possibly as the response of an axon reflex, during and between cluster periods (5), a few hours after cluster attacks (68), and between attacks (29), as well as a normal degree of degranulation (20,73), has been observed. In basophils from cluster patients, increased degranulation after nitroglycerin challenge in vitro has been shown, a response that was normalized after incubation with lithium solution (129).
Prostaglandins and Leukotrienes
Prostaglandins, leukotrienes, and other eicosanoids have been proposed as possible mediators in the pathogenesis of vascular headache. Prostaglandins are local hormones that are produced at their site of action and have vasoactive properties. Although a tendency toward higher serum levels of prostaglandin E2-like substances during cluster attacks compared with basal values has been shown (117), which might be consistent with vasodilation, nonsteroidal antiinflammatory drugs generally have no therapeutic effect in CH and prostaglandins are not believed to be of primary pathogenetic importance. The leukotriene B4 (LTB4) has the ability to induce hyperalgesia and to enhance vascular permeability, but leukotrienes also have been reported to reduce nociceptive responses to bradykinins (133). During attacks, increased plasma levels of LTB4 analyzed by radioimmunoassay have been reported compared with the pain-free state (134), but with high-performance liquid chromatography the concentration of leukotrienes in cluster patients during and between attacks was below the detection limit of the method (77). During remission, the induced release of LTB4 and LTC4 from circulating basophils was significantly reduced (104) in CH patients compared with healthy controls.
Opioids
Plasma, cerebrospinal fluid (CSF), and platelet concentrations of metenkephalinlike (MET) and β-endorphin-like activities have been studied in patients during different phases of CH and in controls. CSF MET has been reported to be lower during (2,59,60) and between (60) attacks of CH or not to differ (149) compared with control patients. A decrease of CSF MET during attacks may reflect altered antinociceptive functions in CH. Low levels of CSF MET are probably not caused by increased degradation because the activities of enkephalinase and angiotensin-converting enzyme (ACE) in CSF at the lumbar level were not altered in CH patients compared with controls (137). In chronic CH, plasma MET levels have been found to be lower during and after attacks than before the attack (111). In episodic cases higher levels of MET in plasma have been reported during attacks (43,60), and higher (60) or normal levels were found between attacks and during remission (43). The increase in plasma MET during pain may be secondary
to sympathetic activation because MET in circulation is derived mainly from the adrenals, where it is stored with catecholamines. It also may be derived from neutrophils, in which a decrease of MET has been observed parallel to the increase in plasma (44).
to sympathetic activation because MET in circulation is derived mainly from the adrenals, where it is stored with catecholamines. It also may be derived from neutrophils, in which a decrease of MET has been observed parallel to the increase in plasma (44).
As regards β-endorphin concentrations in CSF at the lumbar level, no alterations have been found in samples obtained during and between attacks of CH (60). In plasma, β-endorphin has been reported to be increased during attacks (4) or normal (60) but without a normal circadian rhythmicity in several subjects (48,115). Beta-endorphin in plasma is released mainly from the pituitary gland, where it is synthesized from the same precursor as adrenocorticotropin (ACTH) and β-lipotropin. Lymphocytic β-endorphin is reviewed later in this chapter.
Nociceptin is an opioid neuropeptide with algesic and analgesic properties depending on the site of action. Circulating levels were lowered during cluster periods compared to healthy controls. Lower nociceptin levels were speculated to result in defective regulation of the trigeminal ganglion and insufficient protection against attacks (36).
Neuropeptides, Proteins
Much attention has been focused on the innervation of the cranial vasculature (see Chapter 9). In short, the large intra- and extracerebral vessels including the venous sinuses are supplied by the trigeminal nerve marked by calcitonin gene-related peptide (CGRP), substance P (SP), and neurokinin A (NKA); sympathetic nerve fibers marked by norepinephrine (NE), neuropeptide Y (NPY), and adenosine triphosphate (ATP); and parasympathetic nerve fibers marked by acetylcholine, vasointestinal peptide (VIP), and nitric oxide. The primary afferents of the trigeminal nerve not only transmit nociceptive information but also have efferent properties with the ability to dilate blood vessels, cause extravasation, and release from mast cells.
Local release of neuropeptides from the ipsilateral external jugular vein has been studied in CH. During spontaneous CH attacks CGRP and VIP levels were elevated, whereas there were no changes in NPY or substance P compared with a matched control group (30,56). The CGRP concentrations decreased to normal values within 15 minutes after administration of sumatriptan and oxygen as treatment but remained elevated after pethidine, although there was pain relief. The results indicate that sumatriptan, oxygen, and pethidine relieve pain by different mechanisms. The plasma levels of CGRP also have been reported to be elevated between cluster attacks and to be further increased during nitroglycerin-induced attacks but not by nitroglycerin per se (Fig. 88-1) (39,40) (see also Chapter 95).
Substance P can induce pain when combined with bradykinin, serotonin, or prostaglandins that lower the pain threshold. Activation of substance P fibers of trigeminal or facial nerve origin might explain the pain and the autonomous signs of CH and would be expected to cause an increase of CSF substance P levels, but in samples of spinal fluid from the lumbar level the substance P concentration has been reported to be normal both during (60,135) and between (53,60) attacks. In plasma, substance P is reported to be decreased and its degrading enzyme enkephalinase to be increased during cluster attacks (135). In saliva, CGRP, VIP, and substance P concentrations have been found to be higher during attacks than between attacks, and CGRP and VIP were higher both during and between attacks compared with controls (120).
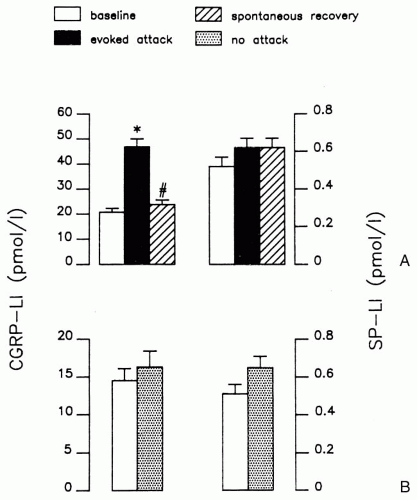 FIGURE 88-1. A: CGRP-Like and SP-Like measured in plasma from the external jugular vein of 12 cluster patients in an active period before nitroglycerin (open columns), at the peak of the provoked headache (solid columns), and after spontaneous remission (dashed columns). B: CGRP-Like and SP-Like measured in plasma from the external jugular vein of 12 cluster patients in remission period before (open columns) and 40 minutes after (dotted columns) nitroglycerin. The columns denote the means ± standard error of mean. Statistical significance (Duncan’s test): *p <0.01 versus values before nitroglycerin and #p <0.01 versus values at the peak of the attack. (Reprinted with permission from ref. 40). |
Endothelin-1 in plasma have been reported to increase during attacks compared to between attacks but with no significant changes of arterial blood pressure (49).
Somatostatin is an inhibitory transmitter peptide found in sympathetic ganglia and in some primary afferent neurons, where it may inhibit substance P release from the C fibers. Somatostatin concentrations in plasma have been shown to be lower during (135) and between (14,135)
cluster attacks as well as during remission (14) compared with controls. An injection of somatostatin appeared to relieve CH pain (135). Somatostatin has venoconstrictive properties (14), which may be of importance for its therapeutic effect. Due to rapid tachyphylaxis, somatostatin is not likely to become a choice for CH treatment.
cluster attacks as well as during remission (14) compared with controls. An injection of somatostatin appeared to relieve CH pain (135). Somatostatin has venoconstrictive properties (14), which may be of importance for its therapeutic effect. Due to rapid tachyphylaxis, somatostatin is not likely to become a choice for CH treatment.
In CH there is an increased morbidity from peptic ulcer and a marked increase of gastric acid secretion during the attack phase. Gastrin levels in plasma have been studied in men between and during cluster periods. When compared with healthy controls, the gastrin levels were significantly higher in CH patients free of peptic ulcer symptoms (118).
Vasopressin has been shown to increase during CH attacks without any concomitant variation of plasma osmolality (47). Pain is one of several inducers of vasopressin secretion via catecholaminergic afferents from the brainstem to the hypothalamus. Serotonin also may trigger vasopressin release. As a potent vasoconstrictor, the increase of vasopressin has been suggested to counteract the vasodilatation associated with the attack (47).
Involvement of Gi proteins in the modulation of pain is widely established and Gi inactivation may produce hyperalgesia and insensitivity to analgesic treatment. Gi proteins inhibit adenylate cyclase and modulate several K+ and Ca2+ channels. In lymphocytes from cluster headache and migraine patients but not in other pain syndromes, a hypofunctionality of Gi proteins has been demonstrated by a reduced capability to inhibit forskolin-stimulated adenylate cyclase activity (52).
Monoamines
Spontaneous cluster attacks often seem to be preceded by a shift of vegetative tone, indicative of increased parasympathetic or decreased sympathetic activity as during relaxation after meals or the working day or in relation to rapid eye movement (REM) sleep. Physical exercise has been shown to reduce the pain of induced attacks, and NE infusion also appeared to alleviate the pain (34). Nitroglycerin-induced attacks seemed to occur after an initial increase of plasma NE had reversed to basal values (66). A further increase in NE occurred during both spontaneous and induced attacks, maybe as a response to vasodilation. Because posture affects NE levels, the evaluation of results during attacks may be difficult (95). When examined before and after 5 minutes of standing, plasma concentrations of NE and epinephrine did not differ between patients in remission and controls, indicating normal postural responses (65). During cluster periods, contradictory results with both increased plasma concentrations of conjugated NE and epinephrine in plasma (93) and decreased concentrations of NE in the morning and at night in comparison with healthy controls were reported (141). The same researchers also found lowered CSF concentrations of vanillyl mandelic acid, homovanillic acid, 5-hydroxyindoleacetic acid, and NE in the active period (141).
Monoamine oxidase (MAO) activity in platelets has been documented in several studies to be lowered during and between cluster periods both in men and women, and when smoking habits are considered, but with no further decrease during cluster attacks (112). The decrease in MAO activity was explained by fewer enzyme molecules (11,142) and lowered Vmax (capacity) with no change in Km (affinity) (147). The enzyme is also more thermostable in CH patients than in controls (147). Because platelet MAO is of the B type, it does not metabolize NE, epinephrine, or serotonin (5-HT), but it may affect these amines indirectly by its decreased ability to catabolize dopamine, tyramine, and other trace amines. MAO is localized in the outer membrane of the mitochondria.
Succinate dehydrogenase (SDH), another membrane-bound mitochondrial enzyme, and the cytoplasmatic enzyme phenolsulphotransferase M (PST M) were analyzed in the same platelets as MAO (96). The SDH activity was significantly lowered in CH, whereas the PST M activity did not differ between patients and healthy controls. In the lowest range of MAO there was an inverse correlation between the activities of MAO and PST M, which was interpreted as a possible control mechanism compensating for a deficiency of one enzyme by another enzyme acting on the same substrates, for instance, dopamine and tyramine. Other platelet functions such as release of β-thromboglobulin and platelet factor 4 were decreased during CH attacks, contrasting with migraine, where increased release is known to occur during headache (22). The fibrinogen-binding properties of platelets from episodic and chronic cluster patients did not differ from those in controls (72). As regards 5-HT uptake into platelets, lowered Vmax and lowered Km (146) or no difference (58) in the kinetic parameters were reported in CH patients compared with controls. Factors such as time of the year (101,146) and medication may explain some differences in the results. Nitric oxide functions were suggested to be involved (22).
Nitric Oxide
The possibility to induce cluster headache attacks during the active period by glyceryltrinitrate, which is an exogenous NO-donor and histamine, which induces NO release from vascular endothelium suggested that NO is a key mediator in cluster headache. Excess NO production or increased activation of NO-ergic pathways might be involved. One study (17) showed that the increase of the NO metabolite nitrite after glycerylnitrate stimulation did not differ between patients during an induced cluster headache attack and healthy controls, and that basal levels of plasma nitrite did not differ between patients and controls. Neither did plasma levels of L-citrulline, a marker of
endogenous NO-production, differ between patients and controls in the basal state. This was judged not to support hyperactivity of the L-arginine-NO pathway in cluster headache. In contrast increased plasma levels of nitrite were reported both in remission and cluster period between attacks as compared to controls. The discrepancies may be due differences in method and numbers of patients (21).
endogenous NO-production, differ between patients and controls in the basal state. This was judged not to support hyperactivity of the L-arginine-NO pathway in cluster headache. In contrast increased plasma levels of nitrite were reported both in remission and cluster period between attacks as compared to controls. The discrepancies may be due differences in method and numbers of patients (21).
Trace Amines
The hypothesis that trace amines such as tyramine, octopamine, and synephrine, closely related chemically to classic biogenic amines, may contribute to the pathogenesis of primary headaches was proposed several decades ago. Trace amines displace biogenic amines from their storage vesicles and have the capability to act as false neurotransmitters. However, despite evidence showing that levels of trace amines in rodent brains are elevated during inhibition of MAO enzymes (MAO-A and MAO-B) or after selective deletion of MAO genes, to date there is no direct evidence supporting the involvement of trace amines in primary headaches.
Recently, however, G-protein-coupled receptors with high affinity for trace amines have been described in rodents and humans. These receptors, called trace amine receptors (TARs), are distinct from the classic biogenic amine receptors and are found in various tissues and organs, including specific brain areas such as the amygdala, hypothalamus, and locus ceruleus. In addition, effects of trace amines, in particular octopamine, on mammalian α2 and β2 adrenergic receptors have emerged. All this opens the possibility that one or more trace amines may in humans behave as neurotransmitters or neuromodulators capable of exerting effects independently or in concert with classic biogenic amines.
A sensitive high performance liquid chromatography (HPLC) method for assessment of trace amines in human plasma and platelets was devised (23). Levels of tyramine, octopamine, and synephrine were, in comparison with healthy control subjects, assessed in patients experiencing CH during both active and remission periods.
In CH, the observation that significantly increased levels of the evaluated trace amines occur during both the remission and the active phases raises the hypothesis that such alterations may reflect the ongoing sympathetic dysfunction. Trace amines are known to be synthesized and stored within the autonomic nervous system. Thus, one possibility is that the increased plasmatic trace amine levels found in CH patients may reflect an increase of tyrosine decarboxylase activity or inhibition of tyrosine hydroxylase (TH) enzyme activity. In support of this hypothesis is the evidence showing that NE, the major product of TH activity, is decreased in platelets in all phases of CH and in plasma and CSF only in the active phase. In addition, the TH enzyme within the autonomic nervous system is the major source of NE in plasma. Another possibility is that the abnormal trace amine levels in CH may reflect hypothalamic dysfunctions. The hypothalamus and locus ceruleus contain, in humans, the highest level of octopamine, and these areas are connected with the autonomic system. Further, low prolactin levels in CH patients in all phases of the disease and after challenge with TRH have been reported. Although these findings may reflect dopaminergic hyperactivity, no evidence has been provided in support of this possibility; an alternative explanation may be an increased level of octopamine turnover in the hypothalamus. Octopamine, in fact, reduces prolactin secretion from lactotrophic cells via nondopaminergic receptors. In addition, hypothalamic abnormalities play a major role in the pathogenesis of CH. A study with positron emission tomography (PET) has demonstrated that regional cerebral blood flow, an index of synaptic activity, is increased during nitroglycerin-induced CH attacks in the posterior area of the hypothalamus (107). The same group, using voxel-based morphometry magnetic resonance imaging (MRI) analysis, has shown an enlarged volume of the gray matter in the same area (108). A new effective treatment, based on stereotactic stimulation of posterior hypothalamus in patients with intractable chronic CH, also supports a hypothalamic involvement (50). Interestingly, TAR-1 mRNA is reported to be expressed in the hypothalamus as well as in the ventral tegmental area, locus ceruleus, and dorsal raphe nucleus, structures that, among other functions, govern the pain threshold.
Recently, PET data of spontaneous CH attacks were published, revealing an activation pattern comparable with that observed in nitrate-induced CH (138).
This emphasizes that CH is not a primarily vascular disorder and that primary headache syndromes can be distinguished on a functional neuroanatomic basis by areas of activation specific to the clinical presentation.
Membranes and Phospholipids
Because a number of membrane-bound functions such as MAO-B, SDH, and PST M enzyme activities and 5-HT uptake in platelets are altered in CH as compared with healthy individuals, it is of interest to examine membrane composition and membrane transduction properties. Therefore, erythrocyte choline concentrations were measured in erythrocytes from CH patients and found to be depressed both during and between cluster periods to values about 50% of those found in controls (26), probably reflecting an abnormality in phospholipid metabolism. Thus, the phosphatidylcholine (PC) content of erythrocyte membranes, from which choline is derived, is increased, suggesting that the decreased concentration of choline could be explained by decreased PC turnover (28). Lithium treatment is known to increase the choline content of erythrocytes. Accordingly, a 12-week course of lithium treatment
normalized the choline content in CH (26), which may be of importance for the prophylactic effect of lithium in CH. Altered receptor-mediated membrane transduction function involving the adenylate cyclase and the polyphosphoinositide (PPI) systems also have been demonstrated in CH (27). Adenylate cyclase, which is linked to surface receptors, is dependent on phospholipid constituents of the membranes for its activity. Accordingly, a significantly lower increase of the second messenger cyclic adenosine monophosphate has been shown in lymphocytes from CH patients than from controls after in vitro stimulation of high-affinity prostaglandin receptors, and a similar trend was shown after stimulation of β-adrenergic receptors (28). The PPI system in platelets stimulated with thrombin has been shown to have enhanced activity in untreated patients and normal activity in lithium-treated patients as compared with controls (27). It has been suggested that the prophylactic effect of lithium could be related to dampening of the activated PPI system to balance the reduced adenylate cyclase activity.
normalized the choline content in CH (26), which may be of importance for the prophylactic effect of lithium in CH. Altered receptor-mediated membrane transduction function involving the adenylate cyclase and the polyphosphoinositide (PPI) systems also have been demonstrated in CH (27). Adenylate cyclase, which is linked to surface receptors, is dependent on phospholipid constituents of the membranes for its activity. Accordingly, a significantly lower increase of the second messenger cyclic adenosine monophosphate has been shown in lymphocytes from CH patients than from controls after in vitro stimulation of high-affinity prostaglandin receptors, and a similar trend was shown after stimulation of β-adrenergic receptors (28). The PPI system in platelets stimulated with thrombin has been shown to have enhanced activity in untreated patients and normal activity in lithium-treated patients as compared with controls (27). It has been suggested that the prophylactic effect of lithium could be related to dampening of the activated PPI system to balance the reduced adenylate cyclase activity.
Further alterations in phospholipid metabolism involve a decreased ability to incorporate 1-14C-arachidonic acid and 1-14C-oleic acid into phosphatidylcholine and an increased ability to incorporate these fatty acids into phosphatidylserine and phosphatidylethanolamine, respectively (45,46). This also may affect membrane function because phosphatidylserine is required to bind the cytoplasmatic enzyme protein kinase C to the membrane during transmembrane signaling. Phosphatidylserine is also a source for polyunsaturated fatty acids in the synthesis of prostaglandins and leukotrienes.
Phosphorus magnetic resonance spectroscopy (31P-MRS) is a noninvasive method by which it is possible to measure high-energy phosphates and the efficacy of ATP production. A defect of brain mitochondrial respiration has been shown in CH both during and after a CH period compared with matched healthy volunteers (98,110). It was also reported that deficient energy metabolism was associated with low free magnesium in the occipital lobes in cluster headache and migraine (99). 31P-MRS of resting gastrocnemius muscle did not differ between patients and healthy controls, but after exercise phosphocreatine recovery was abnormally slow in the patients. The mechanism responsible for the multisystemic mitochondrial impairment is not known. It is suggested that the altered energy metabolism might render the patients more susceptible to metabolic demands during stressful conditions.
Excitatory Amino Acids
Platelets have been studied because they take up glutamate and aspartate by an energy-dependent mechanism similar to that occurring in neurons. Glycine levels in platelets were significantly lower in CH patients than in healthy controls, whereas the levels of aspartate and glutamate did not differ (22), contrasting with the findings in migraine with aura, where the concentrations of all three amino acids were increased. There was no difference in glycine levels during and between cluster attacks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








