BEDSIDE ULTRASOUND FOR SURGEONS
INTRODUCTION
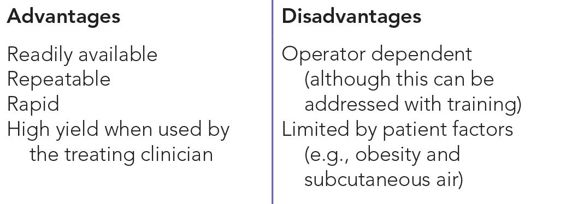
Ultrasound is an available, portable tool that is easy to use and can provide the clinician with essential information for patient care. The use of ultrasound as an extension of the physical examination in surgery has progressively increased over the last decade. This technology applies to a wide variety of surgical specialties and has become a routine tool for evaluating organ systems and for targeting areas for intervention. Table 3–1 summarizes the benefits and drawbacks of ultrasound.
The surgeon using ultrasound must have both basic and specific expertise. This chapter intends to provide a basic summary of ultrasound applications for the general surgeon. It does not replace formal training, and it will not go into detail regarding specialty-based ultrasound such as vascular, endoluminal, thyroid, and breast ultrasound. Basics in the science of ultrasound technology, as well as operator functions, are also addressed in another chapter.
ABDOMINAL AND FOCUSED THORACIC ULTRASOUND
The use of ultrasound for the diagnosis of intra-abdominal injury was first described in 1992 by Tso et al.1 In that initial study, the authors demonstrated that focused abdominal ultrasound examination was both feasible and accurate for the evaluation of bleeding following blunt trauma.1 The Focused Assessment with Sonography for Trauma (FAST) examination was introduced later as the diagnostic test of choice in patients with penetrating injury around the heart, as well as to diagnose intra-abdominal bleeding in hypotensive patients after blunt trauma.2–4 Authors quote a 100% specificity and sensitivity for the diagnosis of intraabdominal fluid, and 99% positive predictive value for the diagnosis of fluid in the pericardium with FAST.4 Its utility has been widely recognized since, and in 1996 the FAST examination was added to protocols for Advanced Trauma Life Support (ATLS) training. Since then, ultrasound evaluation of the pleura for fluid and pneumothorax have also become commonplace in trauma. As clinician facility with ultrasound has progressed, limited point-of-care echocardiography has been proposed for the intensive care unit and has been more recently extended to the trauma bay as a useful hemodynamic monitor.5–7
FOCUSED ASSESSMENT WITH SONOGRAPHY FOR TRAUMA (FAST)
The FAST ultrasound is a simple test to learn, as it can be effectively performed with limited scanning planes. It is important, however, to have knowledge of the relevant anatomy and to have a good understanding of the standard scanning planes. One should also keep in mind that modern grayscale (B-mode) ultrasound images are two-dimensional representations of three-dimensional structures.
The purpose of the FAST examination is to find free fluid (presumed to be blood) in the pericardial, pleural, or intraperitoneal spaces. The study is performed using a low-frequency curvilinear probe, which allows for deep penetration and wide field, both optimal features for viewing intra-abdominal structures. Patients are placed supine, and Trendelenburg positioning will bring any intra-abdominal fluid closer to the diaphragm and increase the chances of visualization. Free fluid is jet black, tends to collect in the most dependent areas, and surrounds the organs. Learning to perform the FAST examination involves learning how to visualize the heart, diaphragm, liver, spleen, and bladder; interpretation hinges on an understanding of where free fluid collects adjacent to these organs.
The volume of intraperitoneal blood detected using FAST depends on the skill of the operator and on the views obtained. Overall, the FAST examination is about 90% sensitive for detecting any amount of intraperitoneal free fluid. A good quality FAST can reliably detect about 200 mL of free intraperitoneal fluid,8 and if good images of the pelvis are obtained, even smaller volumes may be detected. To optimize sensitivity, it is important to obtain good images at multiple intraperitoneal sites.9,10 As mentioned, placing a patient in the Trendelenburg position improves the sensitivity for detecting free fluid in the Morison pouch and pelvic views. Most importantly, the FAST examination is nearly perfect for detecting larger volumes of intraperitoneal bleeding that cause shock and require an emergent laparotomy.3,4
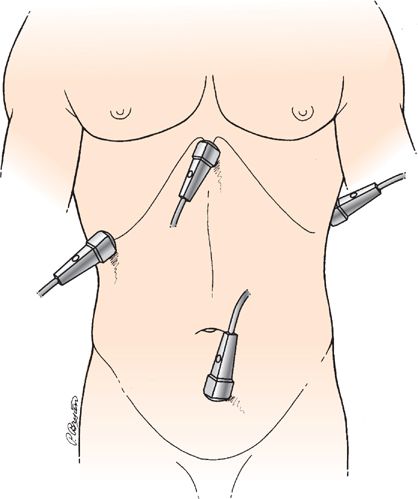
In each view of the FAST examination, the presence of free fluid indicates potential hemoperitoneum or hemopericardium. The views are as follows (Figure 3–1):
Figure 3–1 Probe positions in the FAST examination. (Reproduced with permission from Mattox KL, Moore EE, Feliciano DV. Trauma. 7th ed. New York, NY: McGraw-Hill; 2013.)
• Evaluation of the pericardium through the subcostal window
• Evaluation of the abdominal cavity by visualization of:
• Morison pouch
• Pouch of Douglas
• Splenorenal recess
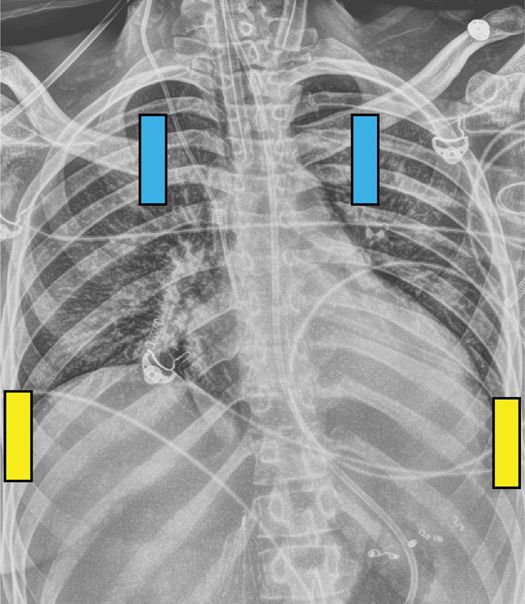
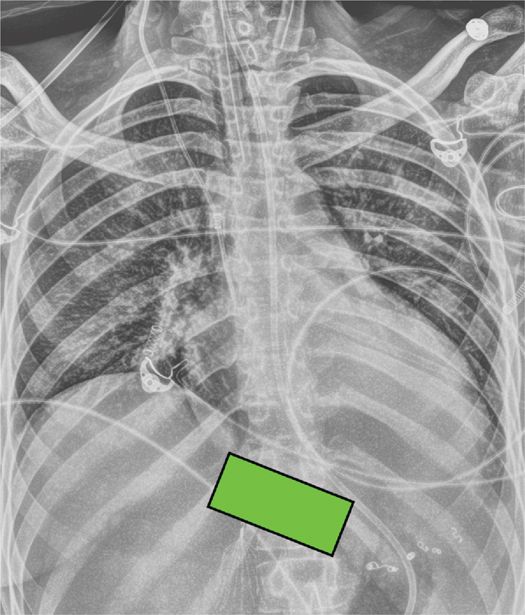
In each of these views, the interface between the viewed organs (liver and kidney, spleen and kidney, ventricular wall and liver, bladder and uterus or rectum) should be bright white. The presence of a jet-black stripe at these interfaces corresponds with blood, i.e., a positive FAST. In an extended FAST, additional views are attained to evaluate the pleura for fluid and pneumothorax (Figure 3–2).
Figure 3–2 Probe positions to evaluate the pleural space. Blue markers indicate position for detection of pneumothorax and yellow markers for detection of pleural fluid.
The following discussion describes the four standard FAST views, as well as the technique for evaluating the pleural space with an extended FAST.
 Pericardial Space (Subcostal View)
Pericardial Space (Subcostal View)
With the patient supine, place the low-frequency probe (1–5 MHz) immediately below the xyphoid, at a 45-degree angle pointing toward the heart. From this window, visualization of the heart chambers, liver, and pericardium can be achieved (Figures 3–3 through 3–5).
Figure 3–3 Probe position to evaluate the pericardial space.
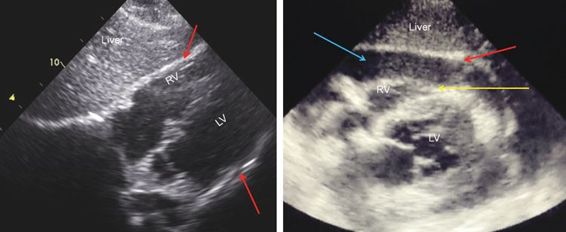
Figure 3–4 Comparison of normal (left) and positive (right) pericardial views on the FAST examination. The bright line designated by arrows in the left image indicates the pericardium. In the setting of effusion, the right ventricular wall (yellow arrow, right image) is separated from the pericardium (red arrow) by a dark stripe (blue arrow). In this image, the right ventricle also appears collapsed, which is indicative of possible tamponade. LV, left ventricle; RV, right ventricle.
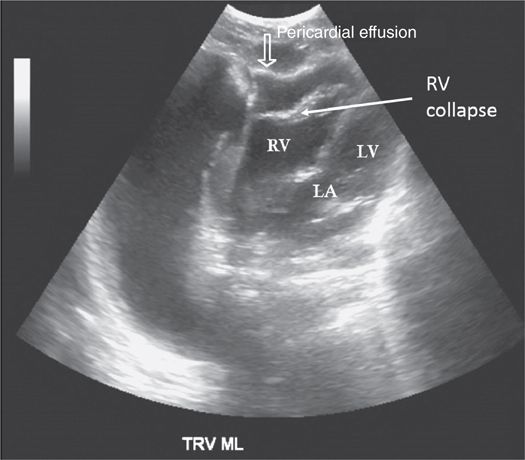
Figure 3–5 Subcostal view demonstrating a pericardial effusion with right ventricular collapse, which is consistent with tamponade. LA, left atrium; LV, left ventricle; RV, right ventricle.
 Morison Pouch (Right Upper Quadrant View)
Morison Pouch (Right Upper Quadrant View)
With the patient supine, place the probe at the 7th or 8th intercostal space vertically in the right flank. This will allow for visualization of the liver, kidney, and Morison pouch to evaluate for the presence of fluid (Figures 3–6 through 3–8).
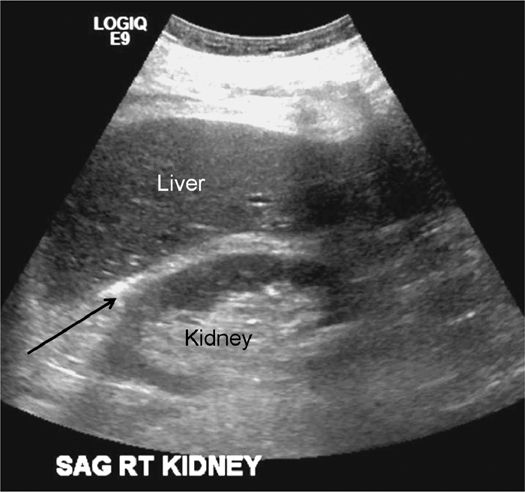
Figure 3–6 Normal FAST examination in the right upper quadrant. The white stripe between the liver and kidney (arrow) may appear black in the setting of hemoperitoneum.
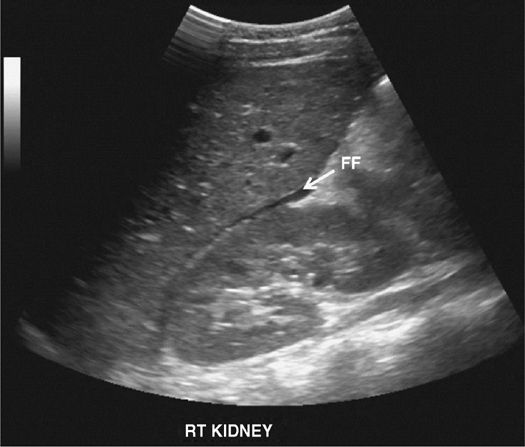
Figure 3–7 Positive FAST with free fluid (FF) in Morison pouch.
Figure 3–8 Positive FAST with free fluid (FF) in the gallbladder fossa.
 Splenorenal Recess (Left Upper Quadrant View)
Splenorenal Recess (Left Upper Quadrant View)
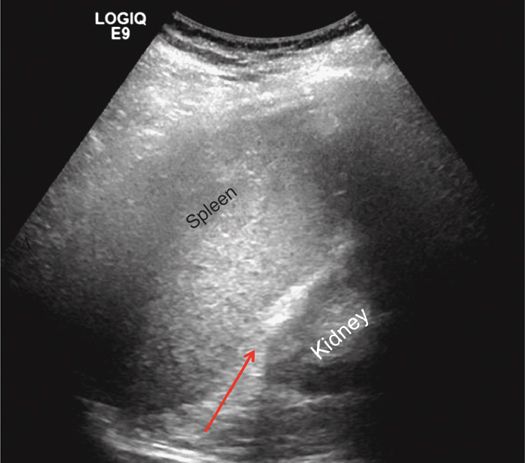
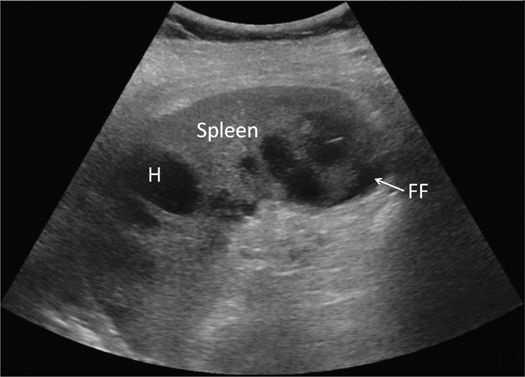
The spleen is usually more posterior and superior than the liver. Aim for the 6th or 7th intercostal space at the mid-axillary line in the left flank to visualize the spleen, diaphragm, and left kidney (Figures 3–9 and 3–10).
Figure 3–9 Normal left upper quadrant FAST view. In the setting of hemoperitoneum, blood may collect in the splenorenal recess (arrow), producing a black stripe between the spleen and left kidney.
Figure 3–10 Positive left upper quadrant FAST. Note the free fluid (FF) beneath the spleen. H, splenic hematoma.
 Pouch of Douglas (Pelvic View)
Pouch of Douglas (Pelvic View)
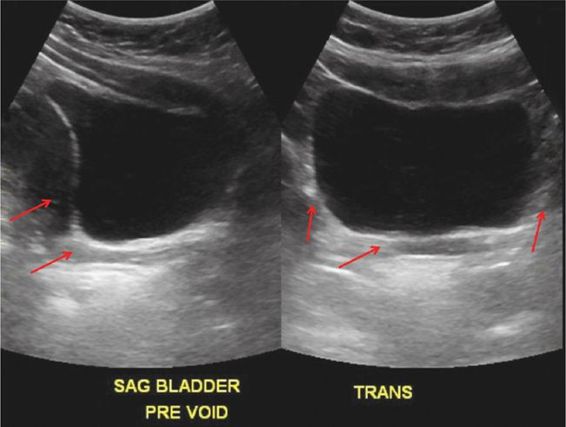
Since visualization of the bladder is sometimes obscured by the bony pelvis, these views are not easy to obtain compared with those in the upper abdomen. Obtaining two views in the pelvis, both transverse and longitudinal, will increase the chances of detecting free fluid.
Perform the longitudinal view first, as it allows for an easier elucidation of the anatomy. Place the probe in the midline just cephalad to the pubic bone, with the marker-dot pointed cephalad. Make sure the probe position is correct by actually placing the probe on the pubic bone and noting a bone shadow on the image. From this position, sliding the probe slightly cephalad will produce a good longitudinal pelvic view. The bladder will be found just superior to the pubic bone and can usually be found even if it is nearly empty. A full bladder will be triangular in shape.
To obtain transverse views, simply rotate the probe 90 degrees, pointing the probe marker to the patient’s right side (Figure 3–11).
Figure 3–11 Normal pelvic FAST in sagittal (left) and transverse (right) views. Arrows indicate possible sites of fluid collection in hemorrhage.
 Visualization of the Pleura
Visualization of the Pleura
Using ultrasound to evaluate for a pneumothorax is a relatively new concept, but it is easy to learn. Since air is a poor conductor of ultrasound waves, the evaluation of the pleura relies on artifacts for the detection of abnormalities.
Pneumothoraces are common in trauma, and more than half are missed on a supine chest radiograph.11–14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree