Fig. 1.1
The denser the material is, the more it reflects the sonographic waves. Fluid [like bile in the gallbladder (GB)] transmits sound waves and has minimum waves reflected back. This yields a black “anechogenic” image. Stones (S) yield white images with a shadow behind them. Soft tissues, like the liver (L), yield different gray color scales. Fibrous tissue like the diaphragm will be white without a shadow (D)
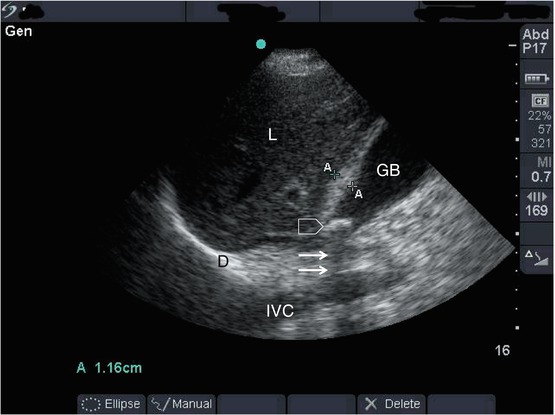
Fig. 1.2
Ultrasound of the right upper quadrant in a patient complaining of right upper quadrant pain to demonstrate acoustic impedance. The gallbladder (GB) and IVC contain fluid which is black. The liver (L) is a soft tissue and is gray in color. The diaphragm (D) is a fibrous tissue which is white without a shadow, and a gallstone which is a solid structure (arrow head) is white with a posterior acoustic shadow (small arrows)
1.3 Ultrasound Transducers
Transducers contain piezoelectric crystals that emit ultrasound. There are different factors that can control the way these ultrasound waves are sent:
1.
Continuity: Emission of ultrasound waves can be either interrupted or continuous. Emission of ultrasound waves as pulses will have two periods: a period in which the pulse is sent and another period in which reflected waves are received to generate brightness (B) mode images. Continuous emission of ultrasound waves is used for the Doppler mode.
2.
Frequency: By modifying the frequency in which waves are sent, it is possible to have different applications controlling mainly the depth and resolution of the images. Frequency and resolution have an inverse relationship. The lower frequency is, the poorer the image resolution, but the greater the depth of wave penetration. Higher frequency probes have less depth penetration but have the advantage of higher resolution.
The transducer frequencies commonly used for abdominal exam are between 2.5 and 5 MHz. This implies that for obese patients and deep structures, probes of low frequencies should be used. In contrast, probes of high frequency (10–12 MHz) should be used for superficial structures.
3.
Shape of the surface of the probe: Ultrasound waves are sent vertical to the surface of the probe. By curving the surface, it is possible to widen the area of the studied field. It is understandable that the lateral resolution in the deeper structures will be less when using this type of probes. Lateral resolution is the ability of ultrasound to differentiate between two objects located perpendicular to the ultrasound beam. These probes are called convex array probes (Fig. 1.3). When the surface is kept flat, the waves will be parallel with each other, and the lateral resolution will be much better. These are called linear array probes. These probes usually have high frequencies of 10–12 MHZ indicating that their penetration is less than others, but they have excellent resolution. That is why the shape of the image of the linear array probe is rectangular compared with the convex array probe images which will be wider in the area located away from the probe.
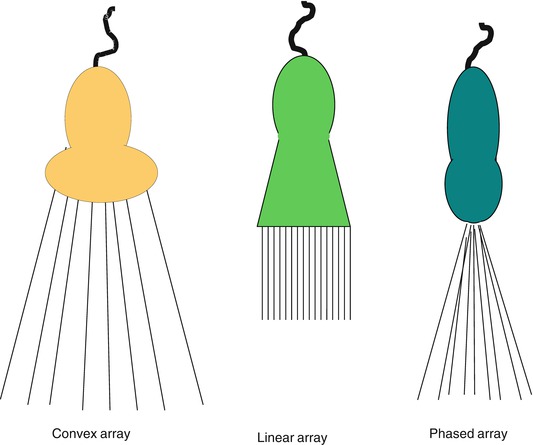
Fig. 1.3
Changing the shape of the surface of the probe and its size has resulted in different types for different applications
4.
Surface area of the probe: It is important to have no barrier between the studied structures and the ultrasound waves. For example, the ribs will not permit ultrasound waves to pass through them when imaging intrathoracic structures through the thoracic wall and will have a shadow behind them. The phased array probe has a small surface that will enable the examiner to visualize the heart between the ribs (Fig. 1.3).
5.
Orientation of the probe: Each piezoelectric crystal in the probe is represented on specific points on the screen. Each probe will have a marker to identify a specific side of the probe. The operator should know the probe side before starting any diagnostic or interventional procedure. This side should be confirmed practically by putting gel on the surface and moving the index finger on it to see which side it represents. It is advisable as agreed standard to have the marker that represents the right side of the screen upward toward the head of the patient in the sagittal or coronal sections (Fig. 1.4) and to the right side of the patient in transverse sections (Fig. 1.5). This will save time as emergency physicians will do both abdominal and thoracic images in emergency conditions and there is no time to change the setting. The rule of thumb is that “the right side of the patient should be on the right side of the screen.”
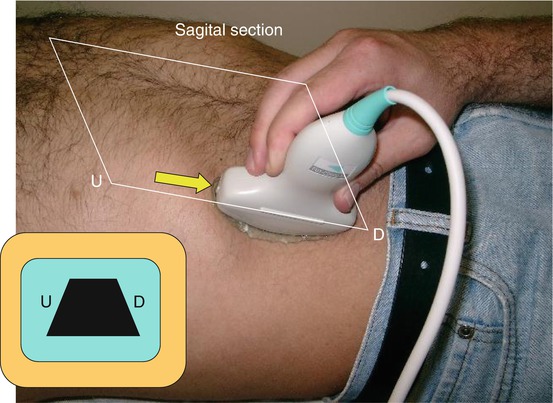
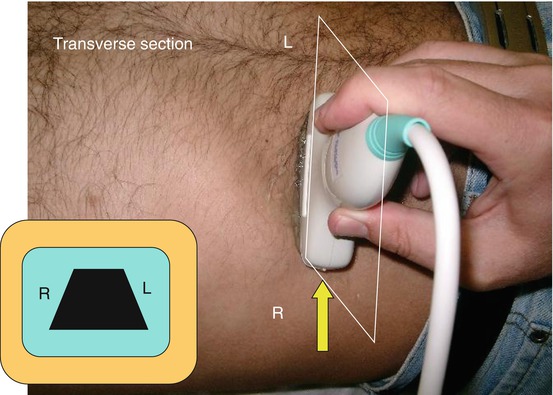
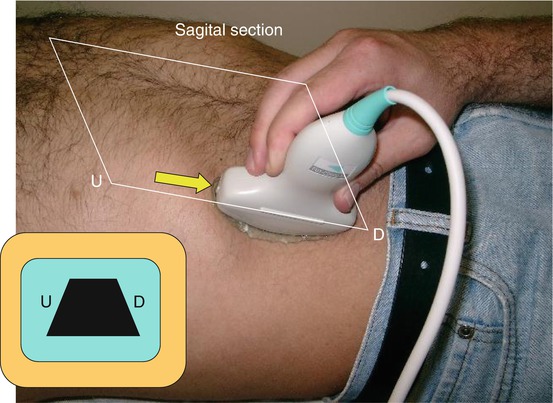
Fig. 1.4
Sagittal section of the abdominal examination. The probe marker (arrow) should point upward. The upper part of the abdomen (U) should be to the right side of the screen. U upward or proximal, D down or distal
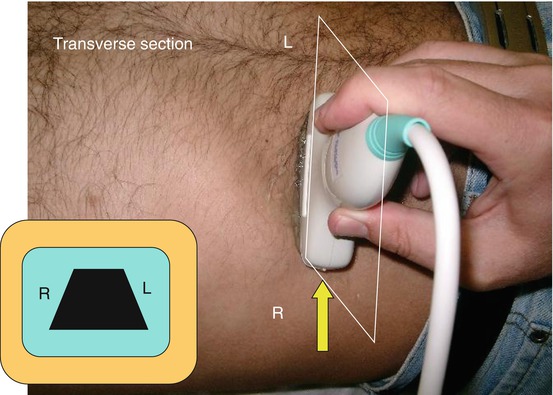
Fig. 1.5
Transverse section of the abdominal examination. The probe marker (arrow) should point to the right. The right part of the body (R) should be to the right side of the screen. R right, L left
6.
Get Clinical Tree app for offline access

Slicing the body to get images: It is important to appreciate that the B mode is a two-dimensional (2D) section that depends on the anatomical site of the slice. The body can be sliced at different planes depending on the position of the probe. Sections can be sagittal, coronal, transverse, or oblique. These thin slices are of less than 1 mm each. This implies that we are visualizing only a thin section of the body. Figure 1.6 demonstrates this principle. If the gallbladder shown in this image is sectioned vertically, then it will appear as a single cavity. If it is transected transversely on the plane shown in Fig. 1.6, then it will appear as two cavities and possibly misinterpreted as an intraperitoneal collection. If the transverse planes are moved to be more proximal, then it will be appreciated that this is a continuous cavity.
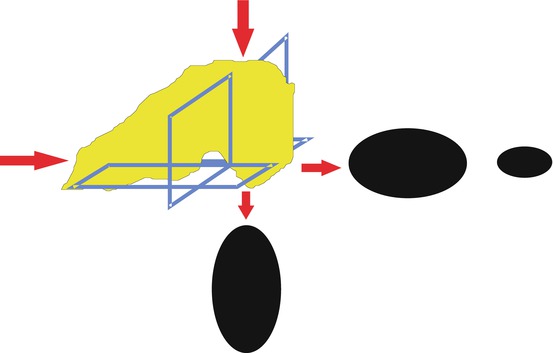
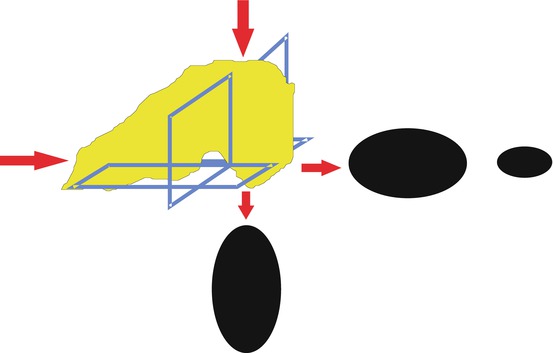
Fig. 1.6




A schematic diagram demonstrating different sonographic images produced when the body is sliced by ultrasound at different planes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







