Fig. 21.1
Pericardial view of the FAST examination. Normal examination (a) contrasted with a positive study (b) with anechoic fluid visible within the pericardial space (arrow)
When the sonographer cannot obtain satisfactory views in the subxiphoid plane, a left parasternal approach may be attempted. The probe should be placed immediately to the left of the sternum at the fourth or fifth intercostal space, initially with the probe marker to the patient’s right side. After obtaining a view of the heart, the probe can be rotated with the marker towards the right shoulder and then the left shoulder, for long-axis and short-axis views, respectively. This technique may be preferred in patients with significant obesity.
Novice operators should bear in mind the following tips:
Examine the interface between the right ventricle and the liver for pericardial fluid and thus tamponade which is the primary objective of this view.
The presence of a small amount of fluid (non-circumferential) may be normal, while the presence of circumferential pericardial fluid along with right ventricular or atrial collapse is alarming.
A pericardial fat pad can be hypoechoic or of mixed echogenicity (contain gray-level echoes) and most commonly is located anterior to the right ventricle.
Obesity, prominent abdomen, abdominal tenderness, gas, as well as pneumoperitoneum/pneumothoraces may obscure the subxiphoid view thus the parasternal long/short axis views may be used as alternatives.
RUQ View
The RUQ view uses the liver as a sonographic window to evaluate for the presence of free fluid in the abdomen. There are four areas to evaluate for free fluid by this view: the pleural space, the sub-diaphragmatic space, Morison’s pouch (potential space between the liver and the right kidney) and the inferior pole of the kidney/paracolic gutter. The probe is placed on the patient at approximately the anterior to mid-axillary line, positioning the probe in the eighth to eleventh intercostal space and parallel to the ribs. Angle the probe counterclockwise to minimize rib shadows if necessary. The probe indicator should be oriented towards the patient’s head. Proper examination of the right upper quadrant should visualize the liver edge, the inferior pole of the right kidney, and Morison’s Pouch (the potential space between the liver and the right kidney, or the hepatorenal space) (Fig. 21.2a). Land marking Morison’s Pouch may be made easier by identifying the bright white fascia of the kidneys (Gerota’s fascia) posteriorly. No single scanning approach will adequately visualize all of the four areas (mentioned in the aforementioned paragraphs) for free fluid and thus subcostal and intercostal approaches are necessary along with maneuvering the probe accordingly. The probe indicator in the subcostal window should point cranially and an effort should be made to scan in the midclavicular line as fluid is dependent. Right intercostal oblique and right coronal views may be used to evaluate for right pleural effusion, free fluid in Morison’s pouch, and free fluid in the right paracolic gutter. The latter may be visualized by placing the transducer in the upper quadrant (coronal plane) and then sweeping it caudally from the inferior pole of the kidney. An awake and responsive patient may be coached on controlling their breathing to allow adequate visualization. Visualization of an anechoic (black) stripe between the liver and kidney (in Morrison’s Pouch) or near the tip of the liver is considered a positive exam (Fig. 21.2b). Novice operators should bear in mind the following tips:
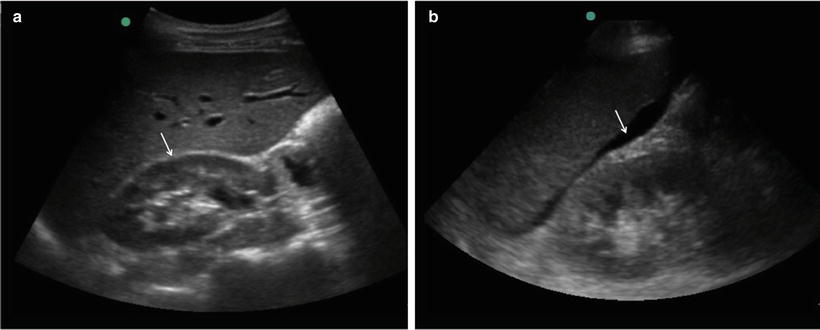
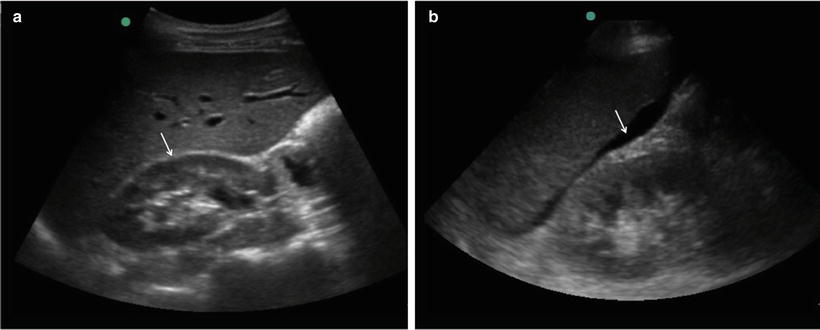
Fig. 21.2
Right upper quadrant (hepatorenal) view of the FAST examination. Normal examination (a) with a clearly visible hepatorenal interface (arrow) contrasted with a positive study (b) with anechoic fluid visible at the hepatorenal interface (arrow)
The perinephric fat should be easily identified as it has an even thickness and is symmetric with the contralateral kidney; perinephric fat is a mimic for hematoma!
The gallbladder, the small intestine, and the inferior vena cava are all mimics for free fluid; use Color/Doppler mode to exclude the presence of a vessel or scan the two-dimensional area of interest carefully and in the context of its neighboring structures.
LUQ View
Proceeding in a clockwise manner to the left upper quadrant, the spleen is used as a sonographic window to evaluate for free fluid in the following four areas: the pleural space, the sub-diaphragmatic space, the splenorenal recess, and the inferior pole of the kidney/paracolic gutter. The probe is placed on the posterior axillary line at the eighth or ninth intercostal space. Again, the probe indicator is pointed towards the patient’s head and the probe may need to be rotated to minimize rib shadows. Examining the left upper quadrant requires visualization of the subphrenic and perisplenic spaces and the left kidney (Fig. 21.3a). The probe must be systematically swept, moved, or angled to visualize all three spaces. Usually the operator has to reach across the patient. The sonographer should sweep the probe usually more posterior and more cephalad than would be expected (think posterior!). The left intercostal oblique and left coronal views may be used to examine for left pleural effusion, free fluid in the subphrenic space and splenorenal recess, and free fluid in the left paracolic gutter. The spleen has a homogenous cortex, an echogenic capsule and hilum. Anechoic (black) blood may be seen between the spleen and kidney (Fig. 21.3b) or often above the spleen and just under the diaphragm with either of these findings being considered a positive test.
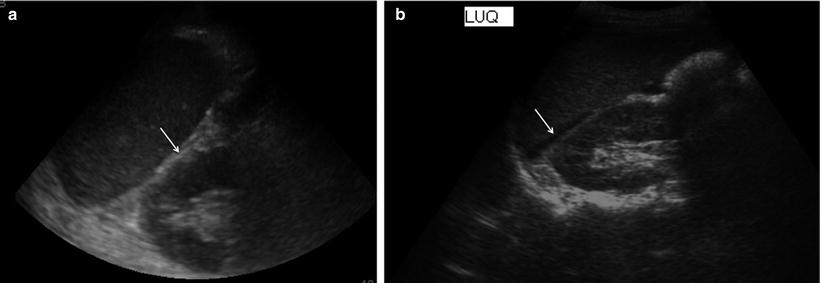
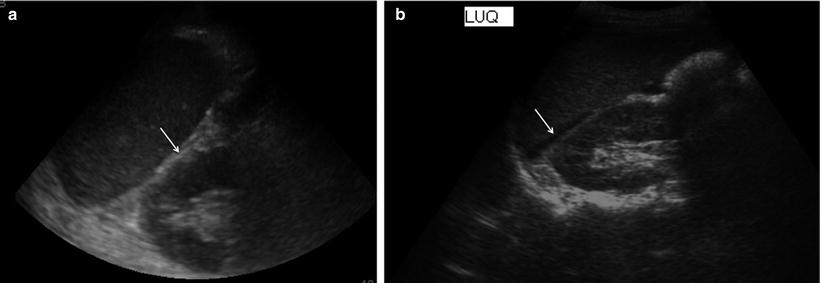
Fig. 21.3
Left upper quadrant (splenorenal) view of the FAST examination. Normal examination (a) with a clearly visible splenorenal interface (arrow) contrasted with a positive study (b) with anechoic fluid visible at the splenorenal interface (arrow)
Novice operators should bear in mind the following tips:
Move the probe posteriorly; angle the probe with the ribs.
Fluid-filled stomach, bowel loops and perinephric fat can all mimic free fluid; thus examine well the two-dimensional area of interest as mentioned in the RUQ view.
Pelvic View
The pelvic view is obtained by using the bladder as a sonographic window to evaluate for free fluid around the bladder (Fig. 21.4a). This is the most dependent part of the abdomen for free fluid accumulation; however the RUQ view remains the most sensitive view for free fluid detection. A high quality pelvic view is dependent on a full bladder, as an empty bladder limits the ability to detect small amounts of free fluid. Because most patients will have a urinary catheter inserted, the examiner may clamp this catheter or instill up to 200 cc of warm isotonic fluid for the purposes of completing an adequate study.
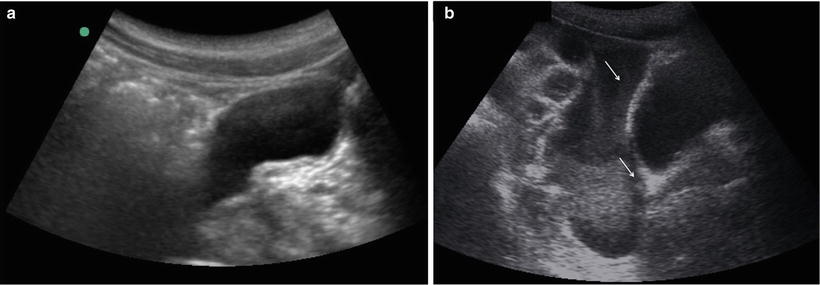
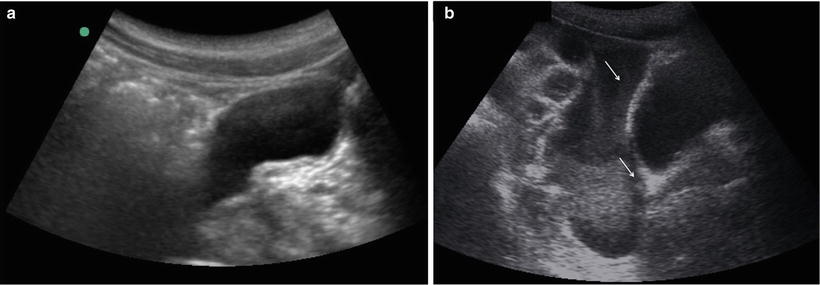
Fig. 21.4
Pelvic view of the FAST examination. Normal examination (a) contrasted with a positive study (b) with anechoic fluid visible in the retro-vesicular space (arrow)
The pelvic view is obtained with a sagittal probe orientation, again orienting the marker towards the patient’s head. The probe should be placed 2 cm superior to the symphysis pubis along the midline of the abdomen, while imaging on both transverse and longitudinal axis should be performed. The probe should be angled down until the prostate or vaginal stripe is identified. When the probe is angled further lower, the two-dimensional image formed will be inferior to the peritoneal reflection. The operator should sweep all planes of the bladder. The probe is swept from right to left or vice versa, paying attention to the retro-vesicular space in males and the retro-uterine space in females for the presence of anechoic (black) free fluid (Fig. 21.4b). As mentioned in previous paragraphs, the presence of anechoic fluid is considered a positive finding. Novice operators should bear in mind the following tips:
In trauma patients the bladder is usually empty and thus clear visualization of the pelvis is often problematic.
Fluid within a collapsed bladder, an ovarian cyst, seminal vesicles, and even the iliopsoas muscles can mimic free intraperitoneal fluid!
Premenopausal women may normally have a small amount of free fluid in the pouch of Douglas.
Reduce the two-dimensional gain for this exam as there is a good chance for observing a posterior enhancement artifact. (A hyperechoic region posterior to the bladder caused by transit of the ultrasound wave through a fluid filled bladder with only limited attenuation.)
When any of the aforementioned views is not clearly visualized, the exam must be scored “indeterminate” rather than negative. If any space in any view demonstrates free fluid, the exam must be scored “positive” regardless of the findings in other spaces, even if the examiner cannot visualize all spaces.
Uses
Blunt Abdominal Trauma
FAST is best studied in the context of blunt abdominal trauma. The Sonographic Outcomes Assessment Program (SOAP) trial, a prospective, randomized study concluded that FAST offered significant benefits including a 64 % reduced time to operative intervention, decreased numbers of Computed Tomography (CT) scans, a 27 % decrease in length of hospital stay, fewer complications, and a significant cost savings [2]. Investigation with FAST has been shown to significantly change management plans in 33 % of applications, including a 28 % reduction in CT scans, and an 89 % reduction in DPL performance [3].
One review compared the FAST to various examinations and investigations in blunt trauma patients, concluding that a positive FAST is better at detecting intra-abdominal injuries than exam findings of rebound tenderness, seatbelt signs, hypotension, abdominal distention, and guarding and also was better than adjunct investigations including reported base deficits, deranged liver enzymes, anemia, or an abnormal chest X-ray. The presence of free intraperitoneal fluid on bedside ultrasonography corresponds to a likelihood ratio of 30 that there is indeed an intraabdominal injury [4].
Perhaps the biggest advantage that FAST provides a Trauma Team Leader is its ready availability as a bedside tool. In circumstances of hemodynamic instability which would normally preclude CT scanning, the sensitivity of FAST is greatly increased. Sensitivity of ultrasound in the hypotensive trauma population approaches 100 % [5, 6]. Even when confronted with an unstable patient, sonographic examinations can be completed within 2–4 min [5, 7, 8]. Up to 90 % of patients with massive hemoperitoneum may be identified by examining only Morison’s Pouch [6], with a mean examination time in one study of only 19 s for patients with positive findings [5].
The point-of-care nature of the FAST exam facilitates repeat exams. When confronted by a negative examination and no immediate indication for surgery repeating the FAST exam can be considered. Studies comparing the sensitivity of repeated FAST after a negative initial study have found that with time—and thus, with bleeding, an increased volume of intraperitoneal free fluid—sensitivity of the exam increases. Repeat examination is also useful in assessing GI injuries which are poorly detected by FAST, increasing the sensitivity of the study from 38 to 85 % when repeated in 12–24 h [9].
While FAST is most often associated with Level 1 trauma centers, the exam has a role in triaging the care of patients from peripheral centers to centers of definitive care. A patient requiring transfer to a trauma center with a positive FAST exam may, given the proper clinical context, be transported directly to an operating theatre which can be prepared in advance of the patient’s arrival.
After considering the evidence, we are left with the conclusion that FAST in the blunt trauma population requires an assessment of hemodynamic stability as a decision point. As we discuss in the “Limitations” section, in the patient who is hemodynamically stable, other diagnostic modalities may yield more definitive diagnoses and subsequent management. FAST can be substituted for diagnostic peritoneal lavage in centers with ready access to an ultrasound device and like DPL [10], FAST serves to alter management primarily in the unstable patient. In a hypotensive population after blunt abdominal trauma, FAST was able to identify 97 % of patients with surgical injuries; in a subset of patients too unstable to undergo CT scanning, 64 % of patients with a positive FAST had surgical injuries whereas zero patients with a negative FAST had surgical injuries [11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






