Key Clinical Questions
What are the different types of plain chest radiographs and when would you order them?
What are the limitations of the anteroposterior (AP) film?
How does the chest radiography differentiate between different types of pneumonia from atelectasis?
What are the radiographic changes you should look for when considering acute, potentially life-threatening causes of chest pain?
What radiographic abnormalities require follow-up?
Introduction
Chest radiographs provide a snapshot of the patient’s physiologic health and insights into a wide variety of systemic diseases. This chapter, as well as Chapter 108 on advanced chest imaging, provide the clinician with a systematic framework for ordering, interpreting films and reports, and consulting the expertise of radiologists.
The majority of hospitalized patients routinely have chest radiographs on admission or prior to surgery; they are also obtained to evaluate acute signs and symptoms, and to assess the possibility of a complication following a procedure. Chest X-rays are also used to monitor critical illness in the intensive care unit (ICU), response to therapy as in congestive heart failure or pneumonia, and stability of pulmonary nodules. Clinicians should always provide radiologists with sufficient information to interpret a radiograph in the clinical context of the patient. Otherwise, the radiologist may generate a wide differential diagnosis that may lead to unnecessary additional imaging or overlook subtle signs of infection in an immune compromised host. Consideration of chest radiographic findings that support the new diagnosis of a systemic disease almost always benefits from direct consultation with the radiologist; a study requisition does not allow an interchange of specific clinical information that can alert the radiologist to findings that might otherwise be ignored. Figures 107-1 and 107-2 show the normal structures that contribute to the radiographic appearance of the chest.
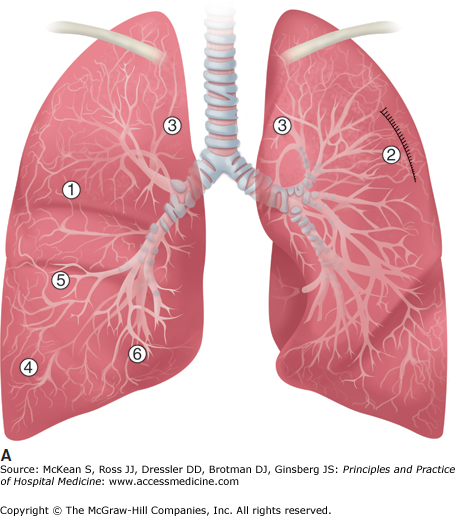
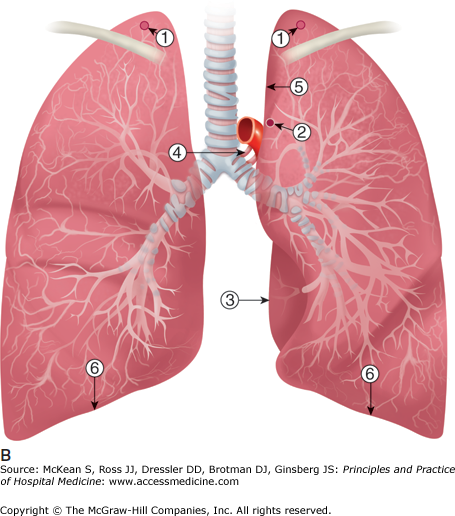
Figure 107-1
(A) Normal chest radiograph anatomic schematic drawing of fissures on PA radiograph. 1, minor fissure; 2–4, major fissure; 5, superior accessory fissure; 6, inferior accessory fissure. (B) Normal chest radiograph anatomy schematic drawing of structures on PA radiograph 1, normal apical opacity; 2, aortic nipple; 3, descending aortic interface; 4, air in esophagus; 5, aortic pulmonary stripe; 6, diaphragm.
Baseline radiographs
|
The clinician can minimize unnecessary test ordering and delays in diagnosis by recognizing the indications for different types of radiographs and their limitations. The interpretation of any radiographic test begins with assessing the adequacy and technical quality of the film(s) in view. The degree of inspiration affects the appearance of the lower-zone vessels that seem more prominent with poor inspiration. The right hemidiaphragm should reach the anterior end of the right sixth or seventh rib or the posterior end of the ninth rib on full inspiration. Then the examiner should carefully inspect the heart, lungs, mediastinum, and chest wall and, whenever possible, compare the current radiograph with prior images. The bones should be examined for fracture and metastatic disease. Rib fractures in particular may indicate more severe pulmonary injury than is readily apparent from the plain film. Although the standard chest radiograph may provide information about the overall health of the bones, special views should be obtained to properly assess the thoracic spine and shoulder joints in cases of trauma or infection. Table 107-1 summarizes the different types of chest projections, indications, and technical considerations. Although a posteroanterior (PA) radiograph provides more information than an anteroposterior (AP) projection, the patient must be able to cooperate and be clinically stable in order to be transported to another area in the hospital for acquisition. Due to magnification based on distance from the image data collector or film, the heart will appear larger on bedside AP chest radiographs and also in obese individuals. Hence, an AP image may suggest heart failure (upper lobe diversion, cardiomegaly, wide mediastinum, and high hemidiaphragms) in patients without fluid overload and significant pulmonary pathology may not be obscured. An AP film is also more likely to miss a small pneumothorax due to anterior collection of air, and diffuse shadowing may signify either poor inspiration or a posterior pleural effusion. Therefore, a PA radiograph may be required for more definitive diagnosis and is the preferred initial study.
| Type of Film | Indications | Technical Considerations |
|---|---|---|
| Posteroanterior radiograph | Preferred image unless patient unstable to evaluate acute signs and symptoms of the chest | Patient stands with anterior chest against film cassette; exposure is full inspiration. |
| Anteroposterior radiograph | Alternative to PA chest for unstable patients |
|
| Lateral view | To localize an abnormality seen in another view; to identify abnormalities obscured by the heart or costophrenic recess | |
| Lateral decubitus view | To identify a small pleural effusion or to distinguish from pleural thickening; to determine if raised hemidiaphragm due to subpulmonary hemothorax; to confirm clinical impression that pectus excavatum with depressed sternum is cause of unusual cardiac contour or cardiomegaly | Patient lying with his abnormal side down |
| PA inspiration- expiration views | To identify pneumothorax; expiration to identify inhaled foreign body when gas trapping is evident | |
| Apical lordotic views | To examine the lung apex usually obscured by clavicle and upper ribs |
The examiner should also routinely check for the presence and position of any invasive medical equipment such as central lines, feeding tubes, or endotracheal tubes (Table 107-2 and Figure 107-3).
| Support Device | Optimum Placement | Proximal Limit | Distal Limit | Common Malposition |
|---|---|---|---|---|
| Endotracheal tube | Middle of intrathoracic trachea | Tip even with top of clavicle | Tip 2 cm from carina | Tip in right mainstem bronchus |
| Central venous catheter | Superior vena cava | Brachiocephalic vein | Cavoatrial junction | Right atrium; interrior vena cava; azygous vein following arch posteriorly; internal mammary vein with slight lateral direction; persistent left superior vena cava can be acceptable depending on vessel size |
| Peripherally inserted central catheter | Depends on use; localization will change with arm position | Arm for long term peripheral access | Cavoatrial junction | Visiting Nurse Association (VNA) service may require superior vena cava |
| Swan-Ganz catheter | Right or left main pulmonary artery | Right ventricle | Interlobar descending pulmonary artery | Distal placement only when wedged |
| Nasogastric tube | Stomach | Side vent marker needs to be distal to gastroesophogeal junction |
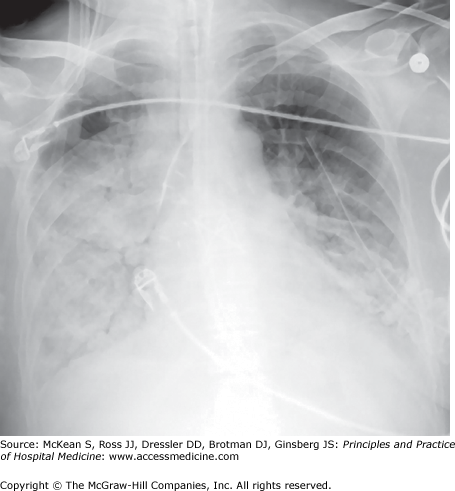
Figure 107-3
ICU patient with dense consolidation and air bronchograms well seen in right lung base corresponding with pneumonia. Support lines include endotracheal tube, left subclavian central venous catheter and left chest tube placed for pneumothorax that may be due to line placement or barotrauma in setting of multi-organ system failure with injury pulmonary edema present.
Chest Radiographic Terminology
The Fleischner Society Lexicon (Tuddenham, 1984) is the standard reference resource for chest radiographic terminology (Table 107-3). The term opacity is used to describe the addition of substances to lungs that results in lighter gray to white appearance of normally dark gray lungs. The term density is not used because density is a photographic term for increasing blackness in the image.
| Descriptive Term | Differential Diagnosis |
|---|---|
| Infiltrate pathologic term often used clinically but not radiographically) | A relatively acute development of a diffuse process that includes little if any consolidation, corresponds with acute interstitial pneumonia (AIP), injury pulmonary edema, corresponding to clinical diagnosis of adult respiratory distress syndrome (ARDS) |
Solitary pulmonary nodule
|
|
Atelectasis
|
|
Kerley A lines
| Distension of anastomotic channels between peripheral and central lymphatics of the lungs. |
Kerley B lines
|
|
Kerley C lines
| Thickening of anastomotic lymphatics or superimposition of many Kerley B lines. |
The Heart
The simplest measurement of the cardiac silhouette, the transverse diameter of the heart, compares the measurements of the widest width of the heart with the widest width of the thorax on standard PA chest radiographs. Cardiomegaly is a nonspecific finding in fluid overload states. The heart may enlarge from baseline without meeting criteria for cardiomegaly, be normal in the setting of acute lung injury, or enlarged for other reasons. Viewing images with prior plain films provides a more reliable assessment of the presence of cardiomegaly due to a wide range of normal and abnormal heart sizes. An important sign of a possible pericardial effusion, separation of epicardial and pericardial fat, should prompt comparison with prior films to determine if there has been rapid enlargement and development of a globular configuration. A characteristic cardiac contour may suggest left ventricular enlargement, but right ventricular enlargement will, for the most part, be indistinguishable from right ventricular displacement in an enlarged heart. It takes at least two years of untreated hypertension to result in a hypertensive cardiovascular silhouette with ectasia of the aorta and more horizontal axis of the heart on PA chest radiograph. For patients with “labile” hypertension, the presence of target end organ damage would be an indication for treatment. Calcification and a change in contour may suggest left ventricular aneurysm, and bulging of the lower third of the left cardiac border may signify aortic valve disease. Prominence of left heart boarder or posterior enlargement of the left atrium may suggest the possibility of mitral stenosis.
Pericarditis Compare current chest radiograph with prior chest radiographs to determine if there is
|
The Lungs
Forty percent of the lung area and 25% of the lung volume may be obscured by the heart and mediastinum on a PA or AP chest radiograph. Both lungs should be equal in size. Fissures should not be wider than hairline. The outline of the hemidiaphragms is usually smooth, arcuate, with the highest point medial to the midline of the hemithorax. Normally, airways are invisible unless they are abnormally thickened or pass through an area of consolidation. Consolidation is the hallmark of airspace disease. Air bronchograms are seen on projection radiographs as lucent tubular branching structures within a larger opacity produced by confluent filling of airspaces by fluid and other substances (Figure 107-3). Volume loss in the region may also contribute to the opacity.
Some terms suggest a broad differential diagnosis that can be considerably narrowed by the clinical context. Large irregular opacities may result from consolidation, lobar collapse, carcinoma, pleural abnormalities, or chest wall lesions. Single or multiple nodular opacities may reflect malignant causes (primary bronchogenic carcinoma, solitary or multiple metastasis) and benign causes (granulomas, atriovenous malformations (AVMs), intrapulmonary bronchogenic cysts, bronchial atresia, and traumatic hematomas. Collapse is often reserved for lobar collapse but by definition, atelectasis is correct at all levels whether a subsegment, segment, lobe or complete atelectasis of the entire lung. The differential diagnosis for collapse is most importantly an obstructing lesion -endobronchial tumor can be lung cancer (including carcinoid that has recently been reclassified as a flavor of lung cancer); endobronchial metastasis (particularly breast, GI tract and renal cell carcinoma); foreign bodies (for example, a peanut); and secretions as mucoid impaction (particularly important in an intubated patient). Pneumonia can occur with collapse related to secretions and particular pneumonias may be more likely to be associated with atelectasis—especially aspiration pneumonia. Atelectasis commonly occurs in the postoperative setting due to low lung volumes. In babies, atelectasis can also reflect decreased surfactant—unusual in adults. Radiographic clues to the presence of atelectasis include: crowding of airways and vessels within the lobe, crowding of ribs shift of mediastinum and other structures, raised hemidiaphragm, compensatory hyperexpansion of ipsilateral lobe and contralateral lung. Additional terms are presented in Table 107-3.
|
The Mediastinum
Mediastinal contour anormalities
|
The mediastinum is divided into radiographic compartments that differ somewhat from the anatomic divisions of the mediastinum.
The anterior mediastinum includes the retrosternal clear space seen on lateral chest radiograph. Radiologists may use either the anterior surface of the aorta or the anterior wall of the trachea as the posterior boundary of this compartment.
The middle mediastinum extends from this boundary to 1 cm behind the anterior surface of the vertebral bodies on the lateral view.
The posterior mediastinum extends posteriorly from the middle mediastinum to the posterior chest wall. The structures in this region all lie posterior to the mediastinum.
Although not a compartment, it is sometimes useful to apply the term superior mediastinum to the region above the aortic arch. The vascular pedicle can be clinically important, especially in the setting of congestive heart failure. It is assessed on the frontal view with greater magnification expected on bedside anteroposterior radiographs than standard posteroanterior radiographs. Distention of the azygous vein to greater than 11 mm in diameter along right side of trachea just above bifurcation signifies pulmonary vascular engorgement.
The hila are often considered with the mediastinal structures. The border-forming structures are the pulmonary arteries. The left pulmonary artery is approximately 2 cm higher than the right pulmonary artery. This slope is sometimes referred to as the hilar angle. It may be altered as in the case of right upper lobe volume loss elevating the right hilum. The direction of the right and left central pulmonary artery differs resulting in expected mild asymmetry. The upper limit of normal currently used on CT scans for the main pulmonary artery is 24 mm with borderline to 29 mm. The upper limit of the normal range in size of the right interlobar descending pulmonary artery most easily measured on chest radiographs is 16 mm for a man and 14 mm for a woman. Increased intravascular pressure can be temporary as in the case of pulmonary edema or long-standing as in the case of pulmonary artery hypertension.
A mediastinal mass in the anterior mediastinum may be a thyroid mass (continuous with the thyroid gland causing deviation of the trachea), a thymoma or thymic cyst (typically marginated and sometimes lobulated), lymphoma and small-cell lung cancer (which may involve multiple lymph note groups), or a germ cell tumor (sometimes evidenced by fat, hair, and teeth). Middle mediastinal masses include tumors involving the esophagus, thyroid, and lymph nodes, duplication cysts including bronchogenic cysts (most frequently at the bifurcation of trachea and central airways, sometimes paraesophageal or intraparenchymal), lymphadenopathy, pericardial cysts (characteristically adjacent to the heart, especially in the cardiophrenic sulcus and smoothly marginated), intrathoracic goiter (with heterogeneous tissue), tracheal tumors, and vascular variants. Posterior mediastinal masses may represent neurogenic tumors and extramedullary hematopoiesis, esophageal abnormalities, and neurogenetic tumors.
In an otherwise healthy adult, bilateral, noncalcified hilar adenopathy suggests sarcoid. In a patient with a prior history of malignancy, the presumption has to be malignancy. Most common malignancies that cause hilar adenopathy include bronchogenic carcinoma, lymphoma, bronchial carcinoid, and extrathoracic primary tumors metastasizing to the chest. Nonmalignant causes include pulmonary arterial or venous dilation or tortuosity, cysts, granulomatous adenopathy, and benign tumors. Reactive and malignant adenopathy may be radiographically indistinguishable unless there is obvious calcification. Vascular abnormalities are often asymmetric and can simulate adenopathy. The first step is to compare with prior films. Consultation with a radiologist and serial review of images will facilitate differentiation of hilar lymphadepathy from pulmonary artery enlargement.