CHAPTER 14
Atlanto-Occipital Joint Injections
INTRODUCTION
The atlanto-occipital (AO) and atlanto-axial (AA) joints are unique joints in the spine, connecting the cervical region to the base of the skull. The AA and AO joints are an often under-appreciated cause of pain, and should be part of the differential diagnosis of cervical spine pain and occipital headaches.
INDICATIONS
AO joint injections are indicated for:
• The diagnosis and treatment of AO joint pathology, which presents as deep pain in the suboccipital region, often unilateral
![]() Especially after flexion/extension injuries
Especially after flexion/extension injuries
![]() Particularly when movement in flexion and extension causes pain
Particularly when movement in flexion and extension causes pain
• Cervicogenic headaches that are impairing functional life indices (restorative sleep capacity, endurance, and quality of life)
• Persistent upper cervical pain that is leading to escalating opioids to control symptoms
• Persistent occipital neuralgia poorly responsive to occipital nerve blocks
The AO joint primarily refers to the ipsilateral suboccipital and retromastoid region, although pain may also refer to the paracervical, suprascapular, and levator scapular regions.1 The normal AO joint is ellipsoid, and permits passive flexion and extension of about 10 degrees as well as 10 degrees rotation and side bending of about 10 degrees.2 There may be decreased range of motion, crepitance, and abnormal head position. When there is pain with side bending during protraction or retraction, the most likely joint affected is the AO joint. Pain or decreased range of motion when nodding from a full rotation is usually related to the AO joint. Unfortunately, the radiologic diagnosis of AO joint pathology has a high false-negative result, since onset of pain precedes any observable structural abnormalities. Characteristic referred pain patterns from AA and AO joint pathology overlap those patterns from the greater and lesser occipital nerves as well as the pain from the C2/3 facet joint,1 making clinical diagnosis difficult. See Figure 14-1.
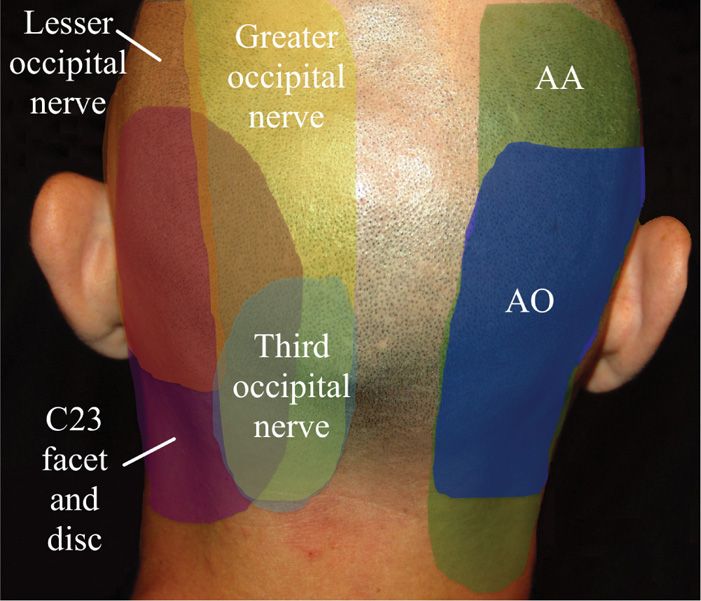
Figure 14-1. Patterns of occipital pain. (Used with permission from Andrea Trescot, MD.)
CONTRAINDICATIONS
• Infection at the injection site
• Coagulopathy
• Cervical spine instability
• Previous cervical fusion at that level
RELEVANT ANATOMY
The first two bones of the cervical spine are unique in their shape and function (Figure 14-2). The C1, or atlas, vertebra is unique in that it does not have a ventral vertebral body, but rather functions as a relay between the occiput and C2. The AO joint is the articulation of the superior articular facet of C1 (the atlas) and the occiput. The AO joint articulates the atlas (C1) with the occiput (C0) and constitutes the C0-1 joint. The AO joint straddles the spinal cord with the foramen magnum on either side and is V-shaped, slanting caudally and medially (Figure 14-3); it holds a volume of 1.0 cc.3
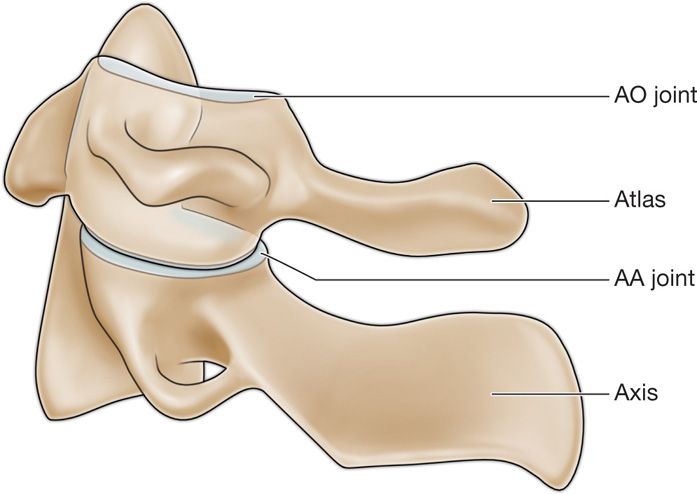
Figure 14-2. Lateral view of AA and AO joints.
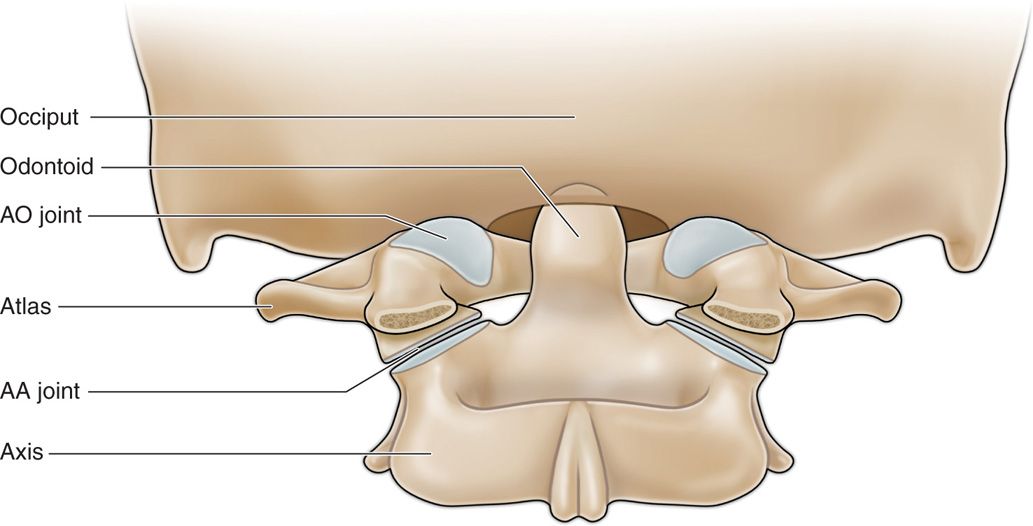
Figure 14-3. AP drawing of AA and AO joints.
The posterior arch of C2 is very deep to the skin and difficult to palpate. The transverse processes are long and perforated by a foramen, which protects the vertebral artery, and the anterior and posterior arches form a triangular conduit for the brainstem. There are grooves in the C1 posterior surface that accommodate the vertebral arteries. The vertebral artery transverses a variable pattern through the wide opening within the transverse process of C2 and travels across the body of C1, running on the lateral one-third of the AA joint dorsally, to enter the foramen magnum medial to the AO joint (Figure 14-4).
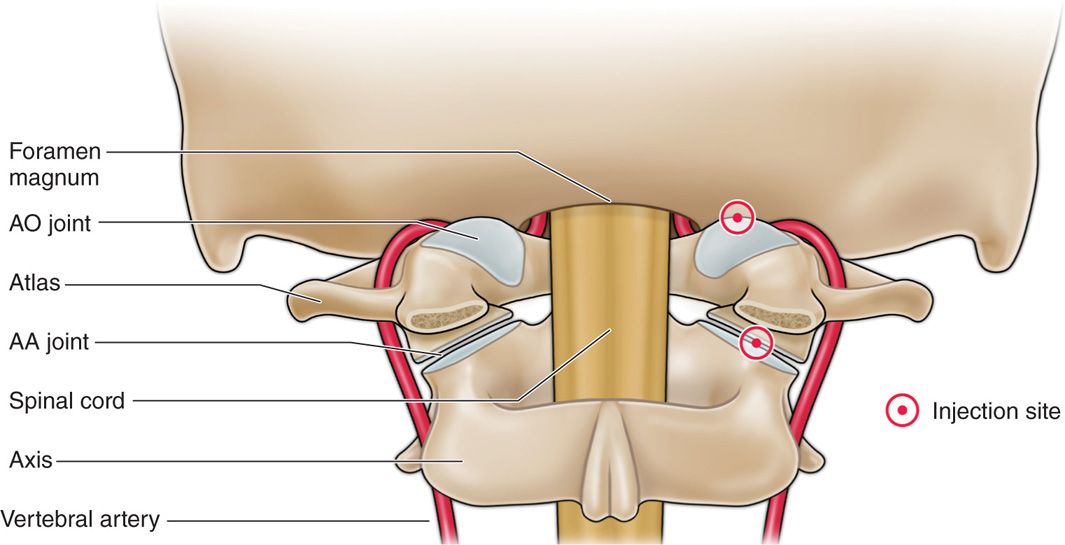
Figure 14-4. Vertebral artery and relationship to AA and AO injection sites. (Used with permission from Andrea Trescot, MD.)
The AO joint shares similar innervation with the AA joint, and is responsible for paracervical myofascial pain, bony joint pain, and intra-articular pain in a variably represented referred pain pattern.
PREOPERATIVE CONSIDERATIONS
A torturous and unpredictable anatomical variance between the vertebral artery and the bony structures (Figure 14-5) suggests that no reliable placement of needle may be expected to be completely safe, and trans-arterial or intra-arterial injections are always a potential disastrous complication; therefore, IV access is mandated. If the patient is anticoagulated, these medications should be stopped. The risk/reward ratio should be in the patient’s favor when assessing when anticoagulation therapy should cease. This requires communication with the patient’s primary care practitioner to further define the risk of bleeding versus the risk of cardiovascular event.
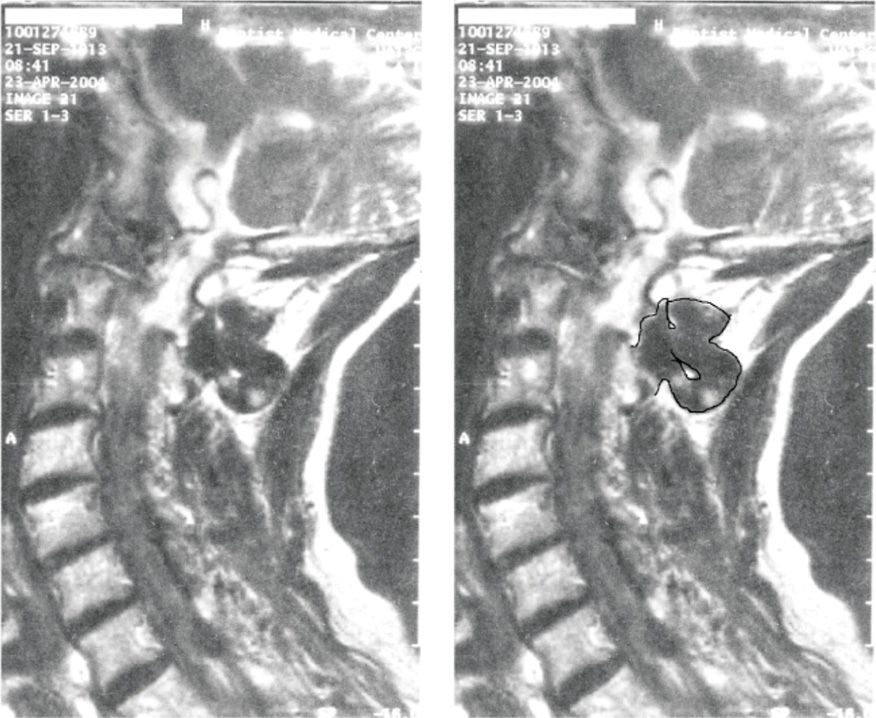
Figure 14-5. Tortuous vertebral artery. (Used with permission from Andrea Trescot, MD.)
FLUOROSCOPIC VIEWS
The fluoroscope is positioned in order to visualize the AO joint as a crisp line. An “open mouth” view may be necessary to adequately visualize the joint (Figure 14-6). An alternative lateral approach places the patient in the lateral position with the symptomatic side up and the head flexed and rotated 45 degrees toward the table. The C2 and C3 segments are aligned and the fluoroscopic beam then angled cephalad or caudad to view the greatest joint opening. From this position, both the AA and the AO joints can be accessed.
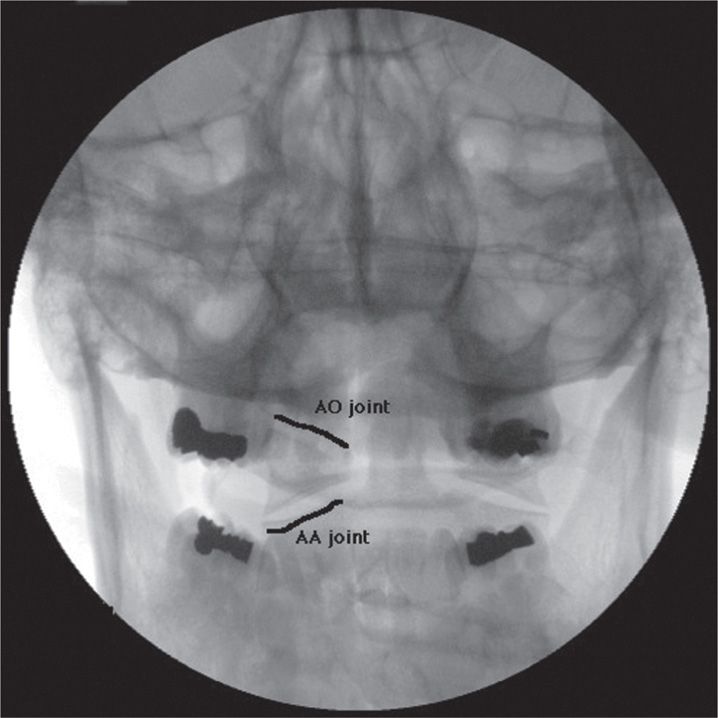
Figure 14-6. Open-mouth view of AO and AA joints. (Used with permission from Andrea Trescot, MD.)
POSITIONING OF PATIENT
The patient is placed in the prone position with the neck slightly flexed and the chest on a pillow, or in the lateral position with the head flexed and rotated 45 degrees for the lateral approach.
SELECTION OF NEEDLES, MEDICATIONS, AND EQUIPMENT
• Needles
![]() 22-gauge 3.5-in Quinke needle or blunt tipped needle with introducer
22-gauge 3.5-in Quinke needle or blunt tipped needle with introducer
![]() Extension tubing
Extension tubing
![]() 3cc syringes (Luer locked)
3cc syringes (Luer locked)
• Medications
![]() Nonionic contrast
Nonionic contrast
![]() Non-particulate steroid
Non-particulate steroid
![]() Local anesthetic (lidocaine, bupivicaine)
Local anesthetic (lidocaine, bupivicaine)
• Equipment
![]() C-arm
C-arm
INTRAOPERATIVE TECHNICAL STEPS
• After a sterile prep and drape, subcutaneous local anesthetic is injected.
• 22g subarachnoid needle (thinner needles are too flexible) is advanced under fluoroscopic control using a “gun barrel” technique to guide the needle to the inferior lateral aspect of the AO joint.
• Once needle contact is made on the inferior edge of the joint line, the needle slides (not losing contact with the periosteum) just off the edge of bone into the joint capsule (Figure 14-7).
• The C-arm is then rotated into a lateral view for confirmation that the needle has entered the joint space (Figure 14-8).
• 0.25 to 0.5 cc of nonionic contrast is then injected, utilizing extension tubing to decrease needle movement. Contrast should spread throughout the joint capsule.
• Venous runoff of the contrast almost always means that the needle is outside the joint, which has a rich vascular plexus (primarily venous).

Figure 14-7. Needle placement (AP) in AO joint. (Used with permission from Andrea Trescot, MD.)

Figure 14-8. Needle placement (lateral) in AO joint. (Used with permission from Andrea Trescot, MD.)
![]() If there is runoff, or spread the contrast into the epidural space, the injection should be terminated.
If there is runoff, or spread the contrast into the epidural space, the injection should be terminated.
• After confirmation of location and negative aspiration, a total of 1 cc of local anesthetic and steroid is injected.
![]() Because of the proximity to vascular structures, concerns regarding intravascular injections of particulate steroid, prudence may suggest the use of a nonparticulate steroid.
Because of the proximity to vascular structures, concerns regarding intravascular injections of particulate steroid, prudence may suggest the use of a nonparticulate steroid.
• The use of a new curve blunt tip “stealth” needle (Epimed) allows for an approach to the suboccipital region from a cephalad approach (Figure 14-9).
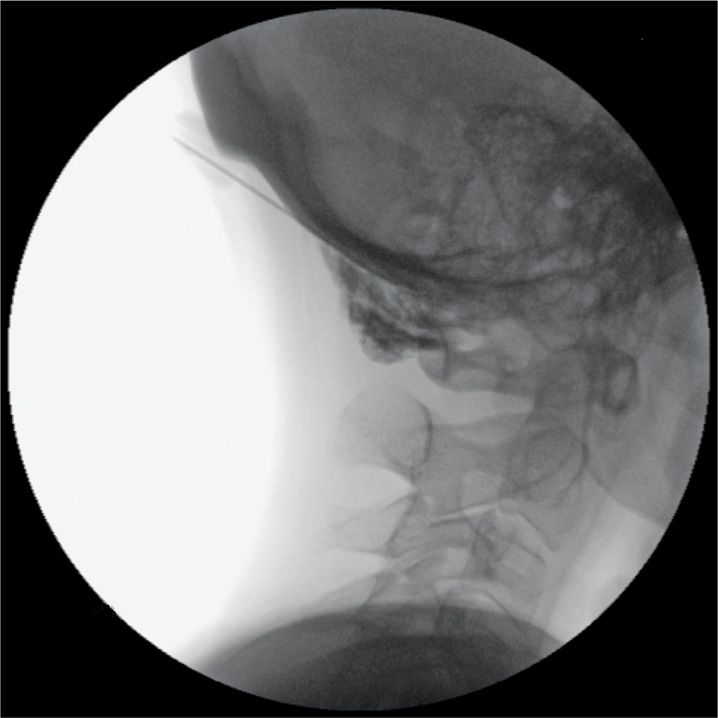
Figure 14-9. Stealth needle placement. (Used with permission from Andrea Trescot, MD.)
POSTPROCEDURE CONSIDERATIONS
• Because there may be a loss of proprioception at the base of the skull with this injection, dizziness and ataxia as well as a sensation of upper neck “weakness” are not unexpected.
MONITORING OF POTENTIAL COMPLICATIONS
• The most dreaded complication of the AO joint injection is an intravascular injection into the adjacent venous plexus, vertebral artery, or carotid artery, with the resultant risk of seizures.
• It is therefore recommended that only a small amount of local anesthetic be injected to decrease the potential for cardiovascular or central nervous system toxicity.
• Anatomically, these joints may share a connection to the epidural space, and careful evaluation of epidural extravasation is necessary prior to injection of local anesthetic to avoid a high epidural or spinal anesthesia.
• Other complications include infections, postdural puncture headache, spinal cord injury, and ataxia.
CLINICAL PEARLS AND PITFALLS
• The AO joint is a more difficult target than the AA joint.
• The AO and AA joints are often evaluated and treated together.
• Although a 25g needle has been described, it is a matter of concern that it is too flexible and would more likely deflect in an undesirable direction.
• Although differential local anesthetic blocks are often recommended in other areas of the cervical, thoracic, and lumbar spine, because of the difficulty in performing the AA and AO injections, it probably is not necessary or appropriate to use “double local anesthetic” techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






