Links: Risks | S/s | Triggers | Dx | Classification & Control | Tx | Referral & Prognosis | MEDS / Pharmacotherapy | Peak Flow | MDI Use | Exercise Induced | Other Types & Resistant | Acute Exacerbations | Pregnancy | Ddx | Allergic (Occupational Asthma) | Obstructive |
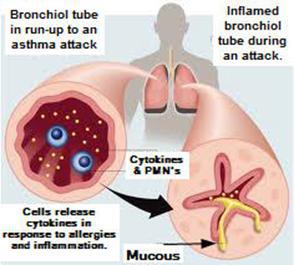 Roughly 6% of the population has asthma. Chronic inflammatory d/o –> episodic cough/ wheeze/ dyspnea. Intermittent reversible airway obstruction and hyper-responsiveness. Airways inflammation with eosinophils, lymphs, mast cells that release cytokines modulate the cells that leads to smooth muscle dysfunction (hyperactivity and bronchoconstriction). Has multiple pathogenic mechanisms, multiple triggers. Has complex genetic inheritance with strong environmental influences. Will lose reversibility with time if get chronic airway remodeling. Reversible airflow limitations, various triggers. Never fully outgrow.
Roughly 6% of the population has asthma. Chronic inflammatory d/o –> episodic cough/ wheeze/ dyspnea. Intermittent reversible airway obstruction and hyper-responsiveness. Airways inflammation with eosinophils, lymphs, mast cells that release cytokines modulate the cells that leads to smooth muscle dysfunction (hyperactivity and bronchoconstriction). Has multiple pathogenic mechanisms, multiple triggers. Has complex genetic inheritance with strong environmental influences. Will lose reversibility with time if get chronic airway remodeling. Reversible airflow limitations, various triggers. Never fully outgrow.
• Childhood asthma is more likely to relapse at, or persist into, early adulthood among individuals who are young at asthma onset, are sensitive to house dust mites, have airway hyperresponsiveness, females (at age 26yo 12.6% of males Vs 16.6% of females still reporting wheezing) and smokers or and dust-mite or cat allergies at age 13 (NEJM 2003;349:1414-22), 21% reported transient wheezing.
• Younger women have the highest incidence of adult-onset asthma (2005 Am Thoracic Soc Conference. Poster 507. Presented May 23, 2005) (overweight and smoking increased the risk).
• Asthma prevalence begins to switch genders at the onset of puberty (about age 11 to 12), when the condition becomes more common in girls researchers found (Am J Respir Crit Care Med 2008;178:321-22)…..The researchers said the correlation between Tanner stage and responsiveness is probably related to hormonal changes, specifically involving estrogen and progesterone…..They dismissed dysanapsis — the differential growth rates affecting lung size and airway size — as a likely mechanism because gender differences reach a peak at about age 18.
PP: There are many factors including host and environmental factors that influence susceptibility to development of asthma in predisposed individuals, precipitate asthma exacerbations, and/or cause sx’s to persist (allergens, respiratory infections, exercise and hyperventilation, weather changes, sulfur dioxide, food, additives, drugs). Inflammation (increased activity of mast cells, eosinophils, PMN’s and T-lymphocytes) leads to airway hyperresponsiveness, resulting in –> bronchoconstriction, airway edema, mucus plug formation and airway wall remodeling (long-term changes). Assessment using hyperpolarized helium-3 magnetic resonance imaging (H3HeMR) suggests that focal changes in regional airflow obstruction tend to stay in the same location within the lungs of pt’s with asthma (J Allergy Clin Immunol 2007;119:1072-1078) (methacholine challenge repeated in 1 to 16 months).
• Intermittent periods of worsening airway inflammation, indicated by exacerbations in asthma, lead to excess lung function decline (Eur Respir J 2007;30:452-456)….prevention of exacerbations should be the primary end-point in asthma therapy.
• Nitrative stress in the form of highly reactive nitrogen species (RNSs) may play a role in the pathogenesis of refractory asthma (J Allergy Clin Immunol 2008;121:355-360)…..in sputum leukocytes it had a significant negative correlation with airway caliber as represented by %FEV-1.
• Widespread antibiotic use in childhood may have increased asthma risk by eradicating H pylori (J Infect Dis 2008;198)…..the presence of H. pylori is linked to less wheezing (odds ratio 0.73) and dermatitis, eczema, or rash (OR 0.73) according to the NHANES population study.
Airway Wall Changes: Airway smooth muscle hypertrophy. Angiogenesis. Basement membrane thickening. Epithelial cell destruction. Increased submucosal vascularity. Subepithelial collagen deposition.
ICD-9 Codes:
493.0 Asthma without status
493.1 status asthmaticus
493.0 Extrinsic asthma (allergic)
493.1 Intrinsic asthma
493.9 Asthma, unspecified
519.11 acute bronchospasm.
519.19 other diseases of trachea and bronchus
Risks: a decr risk if exclusively breast fed the 1st 4mo of life. Incr risk if live in urban area, incr time indoors with poor ventilation and indoor allergens, incr body mass index (BMI), allergic rhinitis. Pre- or postnatal passive smoking greatly increases the risk of asthma or respiratory sx’s in adulthood (Am J Respir Crit Care Med 2005;172:61-66). Obesity presents a major risk for asthma (J Allergy Clin Immunol 2005;May), mechanisms still undetermined, but increased abd and chest wall mass is associated with reduced functional residual lung capacity and this may also affect lung growth in children.
Increasing prevalence: average person spends >90% of time indoors, less fresh air circulation in modern houses. More cooking with gas stoves. More outdoor air pollutants. Less consumption of fish (omega-3 fatty acids are anti-inflammatory). Allergies and sinusitis are more common, both of which lead to inflammation in the airways. Twice as prevalent in children living at sea level Vs the mountains (800-1,200m). There has been a steady rise in the incidence of allergic and autoimmune dz’s (MS, Crohn’s, DM 1, asthma, eczema) in developed countries over the past 3 decades. “Hygiene Hypothesis“: The modern changes in the type and degree of stimulation from the microbial environment with improvement in public health and hygiene may increase the predisposition of chronic allergic conditions in childhood (NEJM 2002;347:869, 911).
• The single best predictor for asthma” is sensitivity to mite allergens, this sensitivity is also seen in >50% of children with atopic eczema, education and house dust mite allergen reduction measures (mite-impermeable mattress covers, removing carpet from child’s room) appear to reduce the incidence of dust mite sensitization in high-risk toddlers and preschoolers (Arch Pediatr Adolesc Med 2002;156:1021-1027).
• Beginning in puberty, asthma prevalence increases among girls, thus it is important to inquire about breathing difficulties and allergies, particularly in females and certain ethnic groups (Native American, black or Hispanic) (Pediatrics 2003;111:1046-54). Bronchiolitis in infancy is associated with an increased risk (30% vs 11% of controls) of asthma later in life (Arch Pediatr Adolesc Med 2004;158:1070-1076).
• While the intake of Vit-E during pregnancy seems to reduce the risk of asthma and eczema in early childhood, intake of Vit-C may actually raise the risk (Am J Respir Crit Care Med 2005;171:121-128).
• A continuing high incidence of asthma past childhood (adult-onset) is most pronounced among females and is linked to increased BMI (Chest 2005;127:1928-1934).
• A rapid rate of growth in length, particularly in small newborns, might be involved in the etiology of asthma (Thorax 2005;60:549-554).
• Paternal history of asthma helps to determine the natural history of asthma in children (Am J Respir Crit Care Med. 2005;172:552-558) (genetic contribution of the father is associated with airway hyperresponsiveness). Adults with asthma are 2-fold as likely than the general population to report a number of chronic medical conditions, including diabetes, arthritis, heart disease, stroke, cancer, or osteoporosis (Chest 2006;129:285-291). Exposure to at least one course of Abx’s in the first year of life may increase the risk of asthma later in childhood according to a meta-analysis (Chest 2006;129:610-618) (lingering q’s include reverse causation, site of infection, and type of Abx’s used). Exposing children early in life to dust and other microbial agents could protect them from developing asthma (J All Clin Immun 2006;April 18) (researchers initially assessed children’s exposure to microbials at 3 mo’s of age and then followed the children, all of whom have atopic mothers and live in the Netherlands, to age 4). There is an increased asthma risk among cleaners or individuals in other jobs in which they are involved in cleaning chemical use (Curr Opin Allergy & Immuno 2006;16:85–90). Smoking increases the risk for asthma in adolescents, especially for those without a history of allergies, according to the results of a prospective cohort study (Am J Respir Crit Care Med. 2006;174:1094-1100) (those who smoked at least 300 cigarettes a year had a RR of 3.9).
• Use of antibiotics during the first year of life (especially more than 4 courses and for non–respiratory-tract infections) increases the risk for asthma by the age of 7 years (Chest. 2007;131:1753-1759)….”we can neither confirm nor refute the causative role of antibiotics in the development of asthma”…..the association was especially strong in rural areas, in the absence of maternal asthma, in the absence of a dog during the birth year, and with broad-spectrum cephalosporin use.
• In a study of 62,000 Danish mothers, the children of those who ate peanuts and tree nuts while pregnant were less likely to develop asthma or allergies (J Allergy Clin Immunol 2012;online June 29).
• Nurses and cleaners are roughly twice as likely as people with other jobs to develop asthma (Lancet 2007;370:295-297,336-341)…exposure to certain cleaning chemicals, bioaerosols, mites, agricultural products, and latex in the workplace. Airway pathology is more common among women with oligomenorrhea than among women with normal menstrual cycles (J Allergy Clin Immunol 2007;120:557-564)….women with menstrual irregularity seem to be at greater risk of asthma and impaired lung function. Pesticides may increase the risk of allergic asthma for women who work on farms, especially those not exposed early in life (Am J Resp and Crit Care Med 2008;Jan 01).
• Physical or sexual abuse may more than double the odds of a child having asthma according to a study of children in Puerto Rico (Am J Respir Crit Care Med 2008;178:453-459)…..asthma appears to be a greater risk for children who have experienced traumatic and stressful events. Daily consumption of nut products during pregnancy increases the risk of childhood symptoms of asthma (Am J Respir Crit Care Med 2008;178:124-131)…..”Maternal diet during pregnancy has the potential to affect airway development and to promote T-helper-2-cell responses during fetal life.”….Children of mothers who reported daily consumption of nut products had an increased risk of wheeze (odds ratio [OR] for daily versus rare consumption, 1.42), dyspnea (OR, 1.58), steroid use (OR, 1.62), and asthma symptoms (OR, 1.47)….These associations were independent from the child’s diet. Gene variants (polymorphisms in chromosomal region 17q21) appear to contribute to early-onset asthma, but not later-developing forms according to a study on 372 families (NEJM 2008; DOI: 10.1056/NEJMoa0806604).
• Retrospective results suggest a relation between acetaminophen use in infancy and development of asthma (OPR = 1.46)(Lancet 2008;372:1039)…..Use in the previous 12 months showed a significant dose-response association with asthma symptoms (ORs ranged from 1.61 for use once in the past year to 3.23 for monthly use)…..Acetaminophen use also was associated with increased risk for eczema and rhinoconjunctivitis symptoms…….However, an association does not necessarily prove cause and effect as the analysis could not control for two important variables — reporting bias (parents of wheezing children might be more likely to give them acetaminophen) and recall bias (parents of children with asthma might be more likely to recall giving the drug).
• Wheezing rhinovirus illnesses in early life may predict development of asthma in high-risk children according to a prospective study (Am J Respir Crit Care Med. 2008;178:667–672)…..OR = 2.6 for wheezing with RSV, 9.8 for rhinovirus (RV), and 10 for both RV and RSV. Childhood asthma was found to be associated with birth during months with high spore or pollen concentrations (odds ratio = 3.1), and another with TV watching for 2 or more hours per day (Thorax 2009;64:353 and 321). Children who are born when there are high spore or pollen concentrations in the air are at increased risk for early wheezing at age 2 years (Thorax. 2009;Published online February 24).
• Infants who grow up in inner-city environments are exposed to different respiratory viral pathogens than infants who grow up in suburban setting….Those differences in exposure may help explain why kids from urban areas appear to be at higher risk for development of asthma as they progress into childhood (J Infect Dis. Published online September 25, 2012)…..infants living in inner-city settings had had fewer viruses detected overall, suggesting there may be other factors, such as environmental pollutants, exposure to toxins, allergic reactions, or exposure to bacteria, that trigger development of respiratory illnesses…..secretions obtained from inner-city infants when they were ill with respiratory symptoms showed lower rates of human rhinovirus (24.1% vs 36.0%; P < .001) and respiratory syncytial virus (6.1% vs 9.7%; P = .07). However, the rate of adenovirus alone was significantly higher in inner-city infants (4.8%) than in suburban infants (0.7%; P < .001).
• The risk of early childhood wheezing is increased in children with high exposure to spores and pollen in the first 3 months of life according to data from 514 children in Salinas Valley (Thorax 2009;64:353-358)……”The ambient spore concentration in the first 3 months of life was positively associated with Th1 levels and Th1:Th2 ratio, and early-life pollen concentration was negatively associated with Th1 levels at age 2 years.”
• Increased duration of television viewing in early childhood – as a proxy measure of sedentary behavior – is associated with the development of asthma later in childhood (Thorax 2009;64:321-325)…..those who watched more than 2 hours/day were almost twice as likely to be diagnosed with asthma by 11.5 years of age compared with children who spent less time in front of the TV (adjusted odds ratio 1.8).
• Chlorine kills germs in swimming pools, but it may also contribute to risk for asthma and nasal allergies (Pediatrics 2009;124:Oct)…..Children with allergic sensitivities (atopy), the odds for asthma increased with the lifetime number of hours spent in chlorinated pools, reaching sevenfold to 14-fold when chlorinated pool attendance exceeded 1,000 hours compared to adolescents who had less than 100 hours of chlorinated pool exposure…..The researchers note that chlorine and its by-products can irritate the skin, eyes, and upper respiratory tract. “The chlorine-based oxidants in water or air floating at the pool surface cause some airway changes and promote the development of allergic diseases,” they write in the study.
• Daycare in early childhood may not prevent later asthma and allergy, thereby challenging the “hygiene hypothesis,” according to the results of a prospective study with 3963 children (Am J Respir Crit Care Med. 2009;180:491–498)……Compared with children who had no use of daycare, those exposed to early daycare (from birth to 2 years) had more wheezing in the first years of life, but less wheezing and corticosteroid use between 4 and 8 years of age. However, this transient reduction in airway symptoms between age 4 and 8 years occurred only among children without older siblings……”We found no evidence for a lasting protective effect of daycare on the prevalence of asthma symptoms, allergies, or bronchial hyperresponsiveness.”
• Women with waist measurements >88 cm had higher risk for asthma than women in the same BMI categories but with smaller waist measurements (Thorax 2009 Aug 25;e-pub ahead of print). HRT with estrogen has been linked to an increased risk (HR = 1.21) for the development of asthma after menopause (Thorax. Published online February 7, 2010). In adults with asthma, low vitamin D levels are linked with lower lung function, increased propensity for bronchospasm, and reduced response to glucocorticoids (Am J Respir Crit Care Med 2010;online Jan). Folate deficiency may increase the risk of asthma and shortness of breath according to data on 6784 adults (ages 30 to 60) (Allergy 2010;online April 26th).
• People who regularly feel stressed out by their jobs may have a higher risk of developing asthma than those with a more-relaxed work atmosphere a study on 5,100 adults they followed for nearly a decade suggests (Allergy 2010;published online April 27th). …..Among those with high job stress, 2.4% developed asthma during the study period, compared with 1.3% of men and women who reported little on-the-job stress……Less-healthy lifestyle did not appear to account for the relationship, the researchers note, so it’s possible that there are direct effects of chronic stress on the hormonal and immune systems that contribute to asthma development — by, for example, making the airways more prone to inflammation in response to an environmental trigger.
• Maternal use of acetaminophen during pregnancy or giving a newborn broad-spectrum antibiotics during the first week of life was associated with a 60% increased risk of wheezing in preschoolers, whereas introducing fish into a child’s diet before age 9 months was associated with a 40% reduced risk (Acta Paediatrica. 2011;100:1567-1571).
Reduced Risk: Children who eat large amounts of whole grain products and fish may have a reduced risk of asthma (Thorax 2006;61:1048-1053) (no clear associations between intake of citrus fruits, vegetables, and dairy products). Men taking low-dose aspirin (325 mg) every other day have a 22% lower risk for receiving an initial asthma dx according to a RCT (Am J Respir Crit Care Med. 2007;175:120-125)….the magnitude of the reduction in risk for newly diagnosed adult-onset asthma was greater among the subgroups who never smoked (31% reduction in risk) and among men younger than 45.9 years (61% reduction in risk).
• Maternal distress in early life plays a role in the development of childhood asthma, especially if it continues beyond the postpartum period, according to the results of a longitudinal study with 13,907 pt’s (Am J Respir Crit Care Med. 2008;177:142-147)…..Risk factors associated with maternal distress in the first year were maternal asthma, urban location, low income, more than 20 healthcare visits, up to 1 sibling, lower respiratory tract infection, nonrespiratory tract infection, and antibiotic use….Risk factors associated with childhood asthma were maternal asthma, male sex, urban location, more than 20 healthcare visits, up to 1 sibling, lower respiratory tract infection, nonrespiratory tract infection, and antibiotic use.
• Women taking low-dose aspirin (325 mg every other day) had 10% reduction in risk for new-onset asthma during 10 years of follow-up according to data from the Women’s Health Study (Thorax 2008;e-pub ahead of print)……persisted after adjustment for age, smoking status, levels of exercise, postmenopausal hormone intake, and randomized vitamin E assignment…..BMI, however, did have an effect: Women in the aspirin group with BMI >30 showed no decreased risk for asthma.
• Low-dose aspirin may lower a woman’s risk for asthma according to analysis of the Women’s Health Study with roughly 37,000 asthma-free health professionals aged 45 or older were randomized to receive 100 mg of aspirin or placebo every other day (hazard ratio=0.90)(Thorax Published Online First: 13 March 2008). Intake of apples and fish by women during pregnancy may have a protective effect against childhood asthma and allergies according to a longitudinal (5yr) birth cohort study with 1253 participants (Thorax. 2007;62:772-778)…..Maternal intake of apples had a protective effect on the children against ever wheezing (odds ratio [OR] for the highest vs lowest tertile, 0.63; 95% confidence interval [CI], 0.42 – 0.95), ever having asthma (OR, 0.54; 95% CI, 0.32 – 0.92), and clinician-confirmed asthma (OR, 0.47; 95% CI, 0.27 – 0.82). Maternal intake of fish had a protective effect on the children against clinician-confirmed eczema (OR for 1 serving per week vs never, 0.57; 95% CI, 0.35 – 0.92).
Hx: Have you had attacks of wheezing? (high pitched respiratory whistling sound when breathing out) Troublesome cough at night or upon awakening? Awakened with difficulty breathing or coughing? Wheeze after physical activity/ exercise induced (EIA)? Seasonal sx’s? Chest tightness after exposure to airborne allergens or irritants? Do your colds “go to the chest” or take more than 10 days to resolve? Are your sx’s relieved when medications are used? PM sx’s always worse (diurnal variations: decr cortisol & epi, with histamine in middle of night). Often worsening sx’s at night awaken the pt. Throat clearing can be first sign of pediatric asthma (NEJM 2003;348:1502-1503).
S/s: See Acute Exacerbations | Wheeze | Episodic cough/ wheeze/ dyspnea. With mild reactive airway disease, prolongation of exhalation without wheezing may be the only sign. Allergy sx’s common. Pt’s with mild acute asthma are able to lie flat. In more severe cases, the pt will assume a sitting position. As the severity increases, the pt will increasingly assume sitting in the tripod position. If symptomatology becomes more severe, profuse diaphoresis occurs. The diaphoresis presents concomitantly with a rise in PCO2 and hypoventilation. In the most severe form of acute asthma, the pt may struggle for air and/or be bradypneic, profusely diaphoretic, and willing to lie recumbent. Ability to speak/staccato speech. Central cyanosis. Stridor. Inspiration-expiration ratio will reveal prolongation of the expiratory phase. (1:1 mild, 1:3 severe). Subcutaneous emphysema. Accessory muscle use, in children, assess supraclavicular and intercostal retractions, accessory muscle use, and nasal flaring.
• History of atopy (odds ratio, 4.44) and exercise-induced asthma (OR, 3.94) predicted persistent asthma in preschool children with wheeze (BMJ 2008;336:1423)…..53% of those with both factors, 17% of those with one factor, and 11% of those with neither factor developed asthma.
Psych: Roughly one-third (32.3%) of patients with asthma use psychotropic medications, including antidepressants (13.7%), anxiolytics (26%), and hypnotic (13%) agents, and 15.1% used at least two of the three classes in the past year according to a study using pharmacy data on 866 pt’s in France (mean age was 37.4 years; 55% were women) (Ann Allergy Asthma Immunol. 2008;100:230-236)(“Asthma patients commonly experience mental distress, that may be a consequence of asthma”)…..the likelihood of using such medications increases as asthma control decreases….Other predictors of psychotropic drug use were older age, female sex, smoking status, and dispensing of antacids or antireflux treatment. Psychological factors (stress) may lead to acute asthma attacks in certain patients (Ann Allergy Asthma Immunol 2008;100:426-432)…..perceived asthma triggers accounted for 12.5% to 37.3% of the variance in Asthma Symptom Checklist hyperventilation-hypocapnia symptoms…..In susceptible patients, hyperventilation “can constrict the airways and lead to typical asthma symptoms”.
Posttussive emesis is a probable sign of asthma in children (American Academy of Asthma, Allergy and Immunology (AAAAI) 2009 Annual Meeting: Poster 17. Presented March 14, 2009)….The prevalence of physician-diagnosed asthma was 23%, occurring in 33 children…..Of those, 48% reported a history of posttussive emesis…..”We think it’s a simple, mechanical thing,” he explained. “There is a flattening of the diaphragm, which compromises the stomach and puts pressure on it, causing it to empty…..”Another possibility is that the airway obstruction pushes air into the esophagus. There is a significant obstruction at the tracheal-esophageal junction in these kids.”
Asthma Triggers: Options include avoiding the trigger entirely, limit exposure to the trigger if it cannot be avoided, or take an extra dose of bronchodilator before/after trigger exposure. Common triggers include inhalant allergens, tobacco smoke, indoor/outdoor pollutants and irritants, workplace exposures, GERD, rhinitis, sulfite sensitivity, and medication sensitivities and allergies. Some triggers are unavoidable, such as upper respiratory tract illnesses, exercise, hormonal fluctuations, and extreme emotion, and patients should be taught to adjust their management accordingly. Upper respiratory tract viruses have been isolated in 80-85% of asthma exacerbations and in 39-64% of COPD exacerbations (Chest 2006;130:1203-1210)…. may result from imbalances in an already disturbed adaptive immune response (as get increased IL-6, IL-8, and RANTES levels in the sputum). Asthmatics appear more susceptible to respiratory virus infections at they produce lower levels of a type of immune cell proteins (interferons) needed to fight off infection from colds and other viruses (J Exper Med 2005;April).
• Days of the year with the highest pollen counts also tend to see a greater number of emergency department visits for people with asthma (J Allergy Clin Immunol 2012;online July 30th)…..The main pollen culprits tied to the increase in hospital visits came from oaks and grasses, whose levels spike in the spring.
• In children, avoidance of tobacco smoke exposure is the most beneficial environmental modification. Hyperresponsiveness (assoc. with atopy) as 80% of children (50% of adults) have +skin test reaction to common indoor aeroallergen such as to dust mites (warm humid areas, avoid chemical reduction methods as harmful in children), cockroach feces (Blattella germanica and Periplaneta americana), Alternaria mold (cold damp areas), cats/ dogs (–>can persist for years after animals are gone, keep them out of the bedroom and wash them weekly). Sensitization to molds (Alternaria alternata and Cladosporium herbarum) is associated with severe asthma (Sensitization to airborne molds and severity of asthma: Cross sectional study from European Community respiratory health survey. BMJ 2002;325:411-4).
• Allergic rhinitis is ubiquitous in children with asthma and may play a contributory role. Rats (Rattus norvegicus) and mice (Mus musculus). Exposure to airborne endotoxin at levels found indoors can increase the airway response to inhaled allergen in pt’s with atopic asthma (J Allergy Clin Immunol 2003;112:1241-1242).
• Among viral wheezing illnesses in infancy and early childhood, those due to rhinovirus are most strongly associated with the development of asthma (Am J Respir Crit Care Med 2008;178:667-672)……An increased risk of developing asthma at age 6 years was associated with wheezing with RSV (odds ratio, 2.6), rhinovirus (OR, 9.8), or both (OR, 10.0) from birth to 3 years of age.
Other: ASA & NSAIDs (Celecoxib, COX-2 agents appears safe but best to observe first dose in the office with Epi and albuterol Nebs nearby, Chest 2002;121:1812-7, J All Clin Imm 2003;111:1116-21), tartrazine (yellow #5 dye, orange), Sulfites in foods (as an antioxidant), metals (chromium, nickel), TDI (toluene, in varnish, paints, plastics), organic dust (wood dust, barn and grain dust, powder from latex gloves), Chemicals (platinum salts, ethylenediamine, phthalic anhydride, diisocyanate in plastics and paints). Grasses (early summer/ fall), tree pollen (spring), weeds (late summer, fall). Cold air, exercise (can cause bronchospasm in up to 80%), laughter, emotionally upset, stings, bites. NSAIDs (7% bet bronchospasm from), menses (premenstrual asthma may benefit from OCP’s). Women with asthma are not at greatly increased risk of having exacerbations or visiting the emergency department during the perimenstrual period (Thorax 2005;60:806-809). 25% of women get worsening asthma during pregnancy (wks 29-36) which usually improves during the last 4 wks. Hyperthyroidism tends to worsen asthma.
Nonspecific irritants (CO, ozone, NO2, particulates, perfumes, SO2). Exposure to ozone at levels below current EPA standards is strongly associated with asthma exacerbation in children with severe asthma (JAMA 2003;290:1859-1867,1915-1916), for every 50 parts per billion increase in 1-hour ozone level, the likelihood of wheezing and chest tightness increased by 35% and 47%, respectively, among asthmatic children using maintenance medication. Asthma exacerbations increased in severity after exposure to high levels of nitrogen dioxide (NO2) during the week before the start of respiratory viral infections (Lancet 2003;361:1939-44), the NO2 may not have been the true causative agent but rather a marker for other pollutants.
• There is no association with the risk of asthma and childhood vaccines such as DpT, OPV, MMR (Ped Infect Dis J 2002;21:489). Melatonin (stimulates incr production of IL-1, IL-6, and TNF-alpha) supplements may exacerbate asthma sx’s (Am J Respir Crit Care Med 2002;166:1055-1061). Glucosamine-Chondroitin supplements may worsen sx’s (J Am B Fam Pract 2002;15:481-4).
• The prevalence of snoring in preschool children is ~10.5% for both genders, snoring is associated with both nocturnal cough and asthma (Chest 2003). New research conducted by Belgian scientists suggests that regular indoor pool use by children and the concomitant inhalation of gases produced by chlorination agents (nitrogen trichloride) is associated with an elevated risk of asthma (Lung hyperpermeability and asthma prevalence in schoolchildren: unexpected associations with the attendance at indoor chlorinated swimming pools. Occup Environ Med 2003;60:385-394), the authors suggest a future move toward non-chlorine-based disinfectants in order to minimize pool users’ exposure to potentially harmful chemicals.
• There appears to be an association between asthma and increased risk of a range of mental d/o’s such as anxiety d/o, specific phobias, panic d/o and social phobia (Arch Gen Psychiatry 2003;60:1125-1130). Pt’s whose asthma begins in childhood is more frequently allergic than those whose asthma began as adults, adult-onset asthma is associated with more rapid loss of lung function (J Allergy Clin Immunol 2004;113:430). Domestic exposure to volatile organic compounds (VOCs, particularly true of benzene), from sources such as solvents and cleaning products, even at accepted levels, may raise the risk of asthma in children (Thorax 2004;59:756-751). Asthmatic children who experience stressful life events such as illness, death, separation and divorce, are at increased the risk (by a factor of 4.69) of having an asthma attack immediately following the event and again 5 to 7 weeks later (Thorax 2004;59:1046-1051).
• More than half of pt’s with asthma can have an attack triggered by laughter (2005 Am Thoracic Soc Conference: Poster F54. Presented May 24, 2005) (probably involves movement in the airways as well as an emotional reaction). Bacteria in household dust (particularly those found on bedroom floors) produce endotoxins that may trigger asthma and asthma-related sx’s such as wheezing (Am J Resp Crit Care Med 2005;Sep).
• While sx’s of rhinosinusitis are associated with asthma sx’s, they have no effect on disease severity based on a meta-analysis of 2519 pt’s with asthma (CHEST 2005 annual meeting. Nov 2005). Adults with a history of childhood asthma frequently have irreversible deficits in lung function (J Allergy Clin Immunol 2005;116:1213-1219)….longer duration of childhood asthma, greater methacholine sensitivity, and premature birth increased the likelihood of abnormal spirometric results in adulthood.
• A national study with >15,000 pt’s found that victimization and missing school due to feeling unsafe are both independently associated with an increased risk for asthma exacerbation among adolescents (Am J Public Health. 2006;96:802-804). Oral prednisolone (2 mg/kg/d divided TID x 3 days) reduces relapses in young children with a first or second episode of wheezing associated with rhinovirus or elevated blood eosinophils (>0.2 x 10^9), but not with RSV (Pediatr Infect Dis J 2006;25:482-488)…confirms that rhinovirus-induced early wheezing as a new major risk factor for recurrent wheezing / school age asthma.
• Sensitization to certain mold allergens appears to increase the risk of severe asthma (Ann Allergy Asthma Immunol 2007;98:153-156)…positive results for molds were seen in 98% of the asthma pt’s and 66% of controls. ….”allergy to Aureobasidium pullulans indoor mold was associated with more severe asthma and sensitization to another indoor mold, Helminthosporium, was associated with asthma exacerbations requiring hospitalizations.”
• Using common household cleaning sprays and air fresheners at least once a week may increase the user’s risk of developing adult asthma, wheezing, or other breathing problems (Am J Respir Crit Care Med 2007;176:731)(RR = 1.49)….does not apply to non-spray cleaners, such as liquid stain removers and washing powders. Gaining just 5 pounds during 1 year resulted in an exacerbation of asthma, particularly in those with poorly controlled asthma (ACAAI: Abstract 23. Presented November 11, 2007).
• Infants younger than 1 year who live within 400 m of a source of diesel exhaust have double the risk for persistent allergic wheeze by the age of 3 years than infants who live farther away (Academy of Allergy, Asthma & Immunology 2008 Annual Meeting: Abstract 252. Presented March 15, 2008)….If the living environment also has a high risk for indoor allergens, this risk is more than 4-fold higher.
• Installation of efficient, nonpolluting heating systems (heat pump, wood pellet burner, or flued gas heater) led to improvements in asthma symptoms but not lung function compared to less-effective heating systems (unflued gas heaters and plug-in electric heaters) (BMJ 2008;337:a1411). The results of a study suggest that even in rural areas, ozone appears to have an adverse effect on childhood asthma (Allergy 2009:1046-1055). Changes in weather (temperature and humidity fluctuations) are linked to asthma exacerbations in children, according to the results of a 2-year, retrospective study (Ann Allergy Asthma Immunol. 2009;103:220–224).
• Neuroticism and interpersonal conflict may increase the risk of developing asthma in middle-aged adults (Allergy 2009;64:1444-1450)…..breaking off a life partnership increased the risk of asthma development by more than twofold. More-frequent burger consumption is associated with a higher prevalence of wheezing in children (>3x/week = odds ratio 1.42 compared with never or occasionally); consumption of fish, fruit, and vegetables might be protective (Thorax 2010;65:516)…..The antioxidants in fruits and vegetables can have protective effects on the immune system and n-3-polyunsaturated fatty acids in fish have anti-inflammatory properties since high burger consumption, but not meat consumption, was associated with wheezing, the risk might be related to lifestyle factors associated with frequent burger consumption (i.e., consumption of fast food or trans fatty acids).
• Dust blown from faraway deserts may accumulate in the air to levels great enough to contribute to children’s asthma attacks (Am J Respir Crit Care Med 2010;online July 23)…..The dust, which contains quartz and other substances and microorganisms that may cause airway inflammation, is transported globally; dust from the Sahara in Africa, for example, can be carried across the Atlantic to the Americas……underscore the importance of keeping an eye on local air quality (mineral-dust levels in the air >1 mg per cubic meter)……there may be no advisories on desert dust specifically, particulate matter — especially coarse dust particles known as PM10 — also rise on heavy-dust days….a hazy sky is a good initial clue that levels of particulate matter are high that day…..AIRNow, at http://www.airnow.gov.
Guidelines Managing the Environment in Pediatric Asthma:
See Allergy Section. Dust mite, pets and seasonal allergy control methods. Children who have airway hyperresponsiveness to histamine and concomitant atopic manifestations have an increased risk of developing asthma by the time they become adults (Chest 2006;129:309-316). To reduce exposure to dust mites, encase all pillows and mattresses on which the child sleeps with impermeable covers. Wash bedding in hot water weekly to remove allergens. If a child with asthma is allergic to animals, find new homes for cats, dogs, and rodents. Eliminate rats or mice if observed in the home. Use interventions for cockroach control, including fixing all water leaks and storing food and trash in closed containers. To reduce mold and mildew, moisture in the house should be minimized; one approach is use of a dehumidifier. Homes and cars should be smoke-free.
Treat the pt’s Allergies: The use of air filters is associated with fewer sx’s among pt’s with allergies and asthma (Chest 2002;122:1535-1542). For pt’s with both pollen-induced rhinitis and asthma, both intranasal and inhaled fluticasone are needed to ameliorate all of their sx’s (Allergy 2005;60:875-881)…..only inhaled provided significant improvements in FEV1 and morning peak flow. Good asthma management requires appropriate tx of allergic rhinitis (Chest 2005;128:3140-3147). Tx of chronic rhinosinusitis leads to improvement in concomitant asthma (Eur Respir J 2006;28:68-74).
Sinopulmonary (Nasobronchial) reflex: inflamed sinus/ upper airway –> heightened airway reactivity, postnasal drip can seed the lungs, mouth breathing from nasal obstruction, systemic absorption of inflammatory cells. All pt’s with the new dx of asthma should be evaluated to determine if the have concomitant sinusitis as it is a common cause of bronchial hyperresponsiveness (Chest 2003;123:757-64).
GERD: For patients with minimal heartburn proton pump inhibitors (Nexium; 40 mg BID x 6 mo) do not appear to be beneficial for poorly controlled asthma according to a RCT on 412 adults (NEJM 2009;360:1487)……even the subgroup of patients with acid reflux documented by pH monitoring did not benefit (nor did it worsen upper airway symptoms) from esomeprazole.
• Use of a proton-pump inhibitor (lansoprazole) in children with poorly controlled asthma does not improve their symptoms according to a study on 300 asthmatic children without symptomatic gastroesophageal reflux (JAMA. 2012;307(4):373-380)…..Among the 115 children with esophageal pH studies, the prevalence of GER was 43%.
• Esomeprazole 40 mg (qd or BID) was of no benefit on 968 pt’s with asthma according to a RCT (Am J Respir Crit Care Med 2010;181:1042).
• It seems that asthma increases the risk of developing GERD, rather than vice versa (Chest 2005;128:85-93) (pathophysiologic mechanisms unkown)…based on a study of >9,000 pt’s, finding a link between asthma and a subsequent first dx of GERD, concentrated in the year following asthma dx. “Gastric asthma” in the past has been proposed due to acid irritating nerves to induce asthma sx’s. Since up to 50% of pt’s with asthma have GERD, the most cost effective way to r/o cause is to give a 20mg/d trial of Omeprazole X 30d. If not responding, get a 24h pH test, if + then treat with 60mg of Omeprazole qd.
• Aggressive tx of GERD in children with asthma appears to reduce the need for asthma medications (Chest 2003;123:973-975,1008-1013). Consider in any pt with asthma that occurs for the first time in adulthood; asthma that gets worse after meals, lying down, or exercise; asthma that gets worse at night; and obese body habitus.
• GERD is common (prevalences as high as 82%) among pt’s with asthma, but typical sx’s may be absent (Chest 2004;126:1490-1494,1398-1399) (unstable asthma and some medicines commonly used for asthma tx may promote GERD, the role of GERD as an asthma trigger remains to be solved).
• Treating pH probe positive GERD in pt’s (omeprazole) with severe asthma did not significantly improve respiratory sx’s of 68 pt’s in one study (CHEST 2005;127:1227-1231).
• A RCT with 700 pt’s potent acid-suppressive therapy (Nexium 40mg BID) resulted in only marginal benefit among asthma pt’s — even those with both GERD and nocturnal asthma sx’s (Am J Respir Crit Care Med 2006;173:1091-7) (small improvement in evening PEF, no change in morning PEF).
Vs Reactive Airway Dz (RAD) –> temporary, usually just after an URI.
Dx (adult or child): a clinical dx that incorporates genetic predisposition and clinical sx’s with objective measures of lung function. Episodic sx’s of airflow obstruction. Difficulty breathing. Chest tightness. Cough (worse at night). Sx’s occurring or worsening at night, awakening the pt. Sx’s occurring or worsening with exercise, viral infections, changes in weather, strong emotions, or menses; or in the presence of animals, dust mites, mold, smoke, pollen, or chemicals. Wheezing. Nearly a third of adults diagnosed with asthma may not actually have the condition (CMAJ 2008;179:1121-1131)…..”Asthma should not be diagnosed based on symptoms alone.”…need spirometry pre and post bronchodilator, and perhaps a methacholine challenge if indicated”.
Spirometry is needed to establish a dx: Airflow obstruction (reduced FEV1 and FEV1/FVC ratio) at least partially reversible Have a decr FEV1 that increases >12% (or 200 mL) after 2 puffs of bronchodilator = reversible airflow obstructive dz. Which is also seen in emphysema, chronic bronchitis, bronchiectasis, upper airway obstruction. May also see a diurnal variation in PEF of >20% over 1-2 weeks.
• Don’t diagnose or manage asthma without spirometry (Five Things Physicians and Patients Should Question. American Academy of Allergy, Asthma & Immunology. Choosing wisely initiative of the ABIM. Online April 2012)….Clinicians often rely solely upon symptoms when diagnosing and managing asthma, but these symptoms may be misleading and be from alternate causes. Therefore spirometry is essential to confirm the diagnosis in those patients who can perform this procedure. Recent guidelines highlight spirometry’s value in stratifying disease severity and monitoring control. History and physical exam alone may over- or under-estimate asthma control. Beyond the increased costs of care, repercussions of misdiagnosing asthma include delaying a correct diagnosis and treatment.
Pearls:
• PFT Patterns with Acute Asthma: Reduced expiratory flow (FEV1/FVC < 70%). Significant response to bronchodilator (12% from baseline or 200cc increase).
• Asthmatics may have normal PFTs between attacks….dx then requires a provocation test (20% fall in FEV1 with low-dose methacholine).
• Other: See normal to increased TLC (hyperinflation). Normal or mild increased DLCO.
• A study of office setting FEV1 measures and asthma outcomes in 417 children (mean age, 9 years) with mild-to-moderate chronic asthma concluded that FEV1 percentage of predicted is an excellent measure of disease severity (Pediatrics 2006;118:e347-55)…..children with FEV1 from 80% to 99% of predicted had almost twice as many sx-free days as children with FEV1 below 60% of predicted (62 days vs. 35 days).
• Serious asthma exacerbations, daily sx scores, and nocturnal awakenings also were significantly associated with lower FEV1 measures. The 2007 NAEPP guidelines recommend the use of spirometry in practices that are regularly caring for patients with asthma as it provides additional information that is useful in monitoring asthma. Only two visits to the pulmonary function lab — one for pre- and post-bronchodilatory spirometry and one for a methacholine challenge test — are necessary to confirm an asthma diagnosis in over 90% of patients (Eur Respir J 2010;January 14th online issue).
Additional Evaluation:
1. Bronchoprovocation: Avoid if FEV1<65% predicted. Exercise challenge, histamine, Methacholine (Provocholine) –> tests for bronchial hyperactivity.
2. Allergy testing. Immunotherapy can be considered if there is clear evidence of sx’s and exposure to an unavoidable allergen, especially if sx’s occur all year and are difficult to control with meds.
3. GERD Tx: up to 80% of adults with asthma have GERD, even if no sx’s, consider trial of Prilosec 40mg/d X 3 mo to look for improvement. Esomeprazole 40 mg BID improves morning peak expiratory flow in pt’s with moderate to severe asthma that requires tx with both inhaled corticosteroids and long-acting beta2-agonists (LABAs) (WCOG 2005.Abstract R.0042. Sept 2005).
4. Exhaled nitric oxide (FENO): See FENO |
5. Sputum Eosinophils: In children with asthma, sputum eosinophils are significantly increased (> 2.3%) in relation to the prior frequency of asthma episodes, as were levels of eosinophilic cationic protein (ECP, >220 ng/mL)(Thorax 2003;58:116-121).
• The presence of eosinophils is associated with more asthma sx’s and lower lung function than the absence of such cells (J Allergy Clin Immunol 2004;113:101-108).
• Sputum eosinophil counts (induced, at 2wks), predict asthma control after discontinuation of inhaled corticosteroids (J Allergy Clin Immunol 2005;115:720-727).
• In pt’s with symptomatic asthma, low eosinophil levels in sputum are associated with a poor response to inhaled corticosteroids (Chest 2006;129:565-572).
6. Other: CXR to r/o other pathology, ENT exam to r/o nasal polyps or sinus dz.
Aspirin-induced asthma: Seen in 4-44% or asthma pt’s. Sx’s typically begin 30 min – 3hrs after ingestion of aspirin. Most are sensitive to all NSAIDs but not to acetaminophen (7% cross-sensitivity). On the aspirin provocation challenge, a positive test was defined as a >20% reduction in FEV1 within 3-4 hours (Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ 2004;328:434-40).
IgE levels are associated with lower baseline lung function and more severe asthma among African American, Mexican, and Puerto Rican pt’s (J Allergy Clin Immuno 2007;120:13)….54.7% of asthmatic pt’s with high IgE had previously been hospitalized compared with 44.1% of those with low IgE. The degree of atopy in children who have asthma in childhood appears to be an important factor in determining whether the condition will persist in later life (J Allergy Clin Immunol 2005;115:61-66) (subjects in remission had a lower serum IgE in childhood (412 ng/mL) than did those with intermittent asthma or persistent asthma 968-1236 ng/mL).
• A “significant portion” of asthma in Americans exists independent from total or specific IgE levels according to data from the National Health and Nutrition Examination Survey (NHANES)(J Allergy Clin Immunol 2009;124:447-453)…..the median total IgE level was 40.8 kU/L. The prevalence of current asthma was 8.8% and the prevalence of atopy, as defined by 15 specific IgEs, was 42.5%…..the prevalence of asthma was higher among atopic than nonatopic subjects (12.9% vs 5.8%)….Roughly 62% of asthmatics had 1 or more positive specific IgE findings, and the adjusted odds ratio for the association between atopy and asthma among this population was 2.41.
Sputum pH: Examination of induced sputum shows that pH is lower in asthmatics than in healthy subjects, and is lowest in poorly controlled asthma (Am J Respir Crit Care Med 2007;175:905-910) (pH was 7.54 in healthy subjects, 7.28 in those with controlled asthma and 7.06 in pt’s with poorly controlled asthma).
Other: An electronic nose that senses volatile organic compounds (VOCs) in exhaled breath can distinguish pt’s with asthma from normal controls (J Allergy Clin Immunol 2007;120:856-862)….”Smellprints” of pt’s with mild asthma were distinguished from those of young controls with 100% accuracy, the authors report, and smellprints of pt’s with severe asthma were distinguished from those of controls with 90% accuracy…..less effective in discriminating pt’s with mild asthma from pt’s with severe asthma.
Psychiatric Aspects: Roughly one-third (32.3%) of patients with asthma use psychotropic medications, including antidepressants (13.7%), anxiolytics (26%), and hypnotic (13%) agents, and 15.1% used at least two of the three classes in the past year (Ann Allergy Asthma Immunol. 2008;100:230-236)(“Asthma patients commonly experience mental distress, that may be a consequence of asthma”)…..the likelihood of using such medications increases as asthma control decreases….Other predictors of psychotropic drug use were older age, female sex, smoking status, and dispensing of antacids or antireflux treatment.
Classification ( 4 steps):
Asthma severity is children >5yo and adults is determined by: Reported impairment over the previous 2 to 4 weeks (sx frequency). Current FEV1 and FEV1/FVC values. Number of exacerbations requiring oral glucocorticoids per year. Peak flow readings can assist as well. See Stepwise Approach for Asthma Management |
1. Mild Intermittent: Daytime sx’s <2x/wk. Use of short-acting beta agonists to relieve sx’s <2x/wk. <2X/mo nocturnal sx’s. Asymptomatic in between exacerbations, which only last hours –> days. FEV1 between exacerbations consistently normal (>80% of predicted normal). FEV1/FVC ratio between exacerbations that is normal (based on age-adjusted values). One or no exacerbations requiring oral glucocorticoids per year.
Note: a person with asthma triggered only during vigorous exercise (EIA) might fit into this category even if exercising >2x/wk. An asthmatic who’s sx’s arise only under certain infrequently occurring circumstances (cat allergy or during a viral URI) are also considered to have intermittent asthma. If these various elements are discordant, the pt’s asthma should be categorized at the level of the most severe. If use >1 albuterol MDI/yr have >mild dz.
2. Mild Persistent: Rule of 2’s: Sx’s >2X/wk, but less than daily use of MDI (rescue inhaler). 3 or 4 nocturnal awakenings with PM sx’s/mo. >2 canisters/yr used per year. Minor interference with normal activities. FEV1 (>80%) and FEV1/FVC (based on age-adjusted values) are normal. PEF variability 20-30%. Two or more exacerbations requiring oral glucocorticoids per year. These pt’s usually need a initiation of daily long-term controller medication such as an antiinflammatory for “dual” therapy. It is estimated that mild asthma accounts for 40% to 70% of diagnosed asthma, and that 25% to 30% of mild asthma is persistent (J Allerg Clinical Imm 2007;118:4).
3. Moderate Persistent: daily sx’s which affect activity. Uses daily beta-agonists. Exacerbations >2X/wk. Nocturnal sx’s >1/wk. Some limitation in normal activity. FEV1 60-80%. FEV1/FVC is 95 to 99% of normal (based on age-adjusted values). Two or more exacerbations requiring oral glucocorticoids per year. PEF >30% variability. Peak expiratory flow monitoring is recommended in pt’s with moderate or severe persistent asthma.
4. Severe Persistent: Symptoms of asthma throughout the day (continual sx’s). Need for short-acting beta agonists for symptom relief several times per day. Extreme limited physical activity. Nightly nocturnal sx’s. FEV1 <60% of predicted. FEV1/FVC <95% of normal (based on age-adjusted values). Two or more exacerbations requiring oral glucocorticoids per year. PEF variability >30%.
Eosinophilic asthma: defined by one of the following: sputum eosinophilia of 3%, peripheral eosinophil count of 0.3×109/L, markedly elevated exhaled nitric oxide, or prompt deterioration of asthma control with a 25% drop in steroid therapy.
5-Item Asthma Control Test:
5 Q’s about the functional impact of asthma, sx’s and albuterol use for age >12yo. Validated with spirometry. Supported by the Am Lung Assoc. All q’s rated 1 to 5, 1 = all of the time, 5 none.
1. In the past 4 wks how much of the time had your asthma kept you from doing as much
2. In the past 4 wks how often did you have SOB, coughing, wheezing.
3. In the past 4 wks how often has it awakened you at night.
4. In the past 4 wks how often have you used your rescue inhaler.
5. In the past 4 wks how would you rate your control.
Scores >19: suggests good control.
Score 16-19: suggests < good control.
Scores <16: suggests poor control.
The ACT accurately identifies pt’s with poorly controlled asthma and tracks changes over time (J Allergy Clin Immunol 2006;117:549-556) (71.3% sensitive and 70.8% specific in classifying pt’s with poorly controlled asthma, the results indicate. PPV and NPV for this cutoff level were 72.6% and 69.3%, respectively).
7 Item Asthma Control Test:
To identify children 4 years old to 11 who have inadequately controlled asthma. The children are asked: the child selects answers that range from a sad face to a smiley face, to indicate the level of impact their asthma is having on their life.
–How is your asthma today?
–How much of a problem is your asthma when you run, exercise or play sports?
–Do you cough because of your asthma?
–Do you wake up during the night because of your asthma?
The caregiver is asked questions on the impact of the child’s asthma during the last for weeks, including:
–How many days per month did your child have any daytime asthma sx’s?
–How many days per month did your child wheeze during the day because of asthma?
–How many days per month did your child wake up during the night because of asthma?
Most people (55%) with moderate to severe asthma in the US live with poorly controlled disease according to a survey of 1812 pt’s (AAAAI 63rd Annual Meeting: Abstract 28. Presented February 25, 2007)…significantly higher rates of healthcare utilization, with more frequent unscheduled physician visits, emergency department visits, hospitalizations, and missed days of work or school in the past year (P < .001 for all). They were also more likely to have gastroesophageal reflux disease, chronic sinusitis, and hypertension, factors that the investigators concluded were predictive of uncontrolled asthma.
Good Asthma Control:
Characteristic | Controlled | Partly controlled (Any present in any week) |
Daytime sx’s | None (2 or less / week) | >2x / week |
Limitations of activities | None | Any |
Nocturnal sx’s / awakening | None | Any |
Need for rescue / “reliever” tx | None (2 or less / week) | >2x / week |
Lung function (PEF or FEV1) | Normal | < 80% predicted or personal best (if known) on any day |
Exacerbation | None | >1x / year or 1 in any week |
NOTES: Higher lung function level in childhood and a higher subsequent increase in FEV1 are associated with asthma remission later in life (Thorax 2004;59:925-929).
Levels of Asthma Control:
Controlled Asthma
Daytime symptoms: Twice or less per week.
• Limitations of activities: None.
• Nocturnal symptoms/awakening: None.
• Need for reliever/rescue treatment: Twice or less per week.
• Lung function (PEF or FEV1): Normal.
Partly Controlled Asthma
• Daytime symptoms: More than twice per week.
• Limitations of activities: Any.
• Nocturnal symptoms/awakening: Any.
• Need for reliever/rescue treatment: More than twice per week.
• Lung function (PEF or FEV1): < 80% predicted or personal best (lung function is not a reliable test for children 5 years and younger)
Uncontrolled Asthma
• Three or more features of partly controlled asthma present in any week.
• The occurrence of an exacerbation should be considered as a symptom of uncontrolled asthma and requires further evaluation of asthma status.
Adapted from: The Global Initiative for Asthma (GINA). 2009 Update of the GINA Report http://www.ginasthma.com. Accessed
Oct 12, 2011.
Tx: Links: Goals & Compliance | Stepwise Approach for Asthma Management | Step 2 to 5 & Stepping Down/up | F/u Q’s | Acute Exacerbations (Adult and Peds) | MEDS | Peak Flow | MDI Use | Spacers | Nebulizer | Dry Powder Use | Action Plan | Classification | Other / Alternative / Thermoplasty | Referral & Prognosis | Triggers |
Goals: Freedom from sx’s (control / prevent chronic sx’s). Normal activity levels. Prevent exacerbation’s that lead to ED & hospitalizations. No loss of school or work. Satisfaction with care. Best possible lung function (maintain near normal PFT’s). Provide optimal pharmacotherapy with minimal or no adverse events Consider immunotherapy.
• Asthma control is defined as the degree to which treatment can ameliorate or eradicate the features of asthma regarding both current clinical control and future risk (Am J Respir Crit Care Med. 2009;180:59-99)……future risk is important for three reasons: first, because some medications can improve symptoms while not treating the underlying disease; second, because some patients are at increased risk of asthma attacks despite having few symptoms; and third, because medication side-effects should be taken into account when deciding a patient’s need for treatment.
Info: Immunize all with influenza. Give all >18 yo the pnuemococcal (PPSV23) vaccine as pt’s are at increased risk of invasive pneumococcal disease. Weight reduction in obese persons leads to significant improvement in pulmonary function, sx’s and health status. Avoid living near busy roads. Minimize exposure to outdoor air after 4pm when it is usually at its worst. Safe to scuba dive is sx’s under good control, use bronchodilator prior to dive.
Stepped care and co-management of the dz to create a partnership between clinician and pt are the basis of tx. If using their quick relief inhaler (short acting beta agonists = SABAs) >2X/wk then need the addition of a long-term “control” med. If getting a increased / significant flair(s), then initiate tx at a higher level than current dz, then step down tx intensity if asthma is well controlled for 2-3 mo. Develop written asthma action plans with pt’s so they know what to do for daily tx and for acute exacerbations. Once controlled for 2-4wks, gradually reduce (step down) doses to level required to maintain control. Step up care just before anticipated onset of sx’s (allergy season). Steroids will take 3-6wks to wash out. If taking PO steroids, reduce to QOD.
Asthma Defies “One Size Fits All” Tx: Many patients (47%) with mild-to-moderate asthma have persistently noneosinophilic disease and thus tend not to respond anti-inflammatory treatment with an inhaled corticosteroids aimed as treating an eosinophilic disorder (Am J Respir Crit Care Med 2012;185:612)……These patients all had similar symptoms, reversible airflow obstruction, and airway hyperreactivity, but only those with airway eosinophilia responded to steroid treatment. This explains why many of our patients do not do well with current asthma treatments, although we don’t yet know what to offer these patients. Unfortunately, sputum cytology is best performed in research settings — and neither blood eosinophilia nor exhaled nitric oxide is an adequate surrogate marker.
Compliance: Review the daily self-management plan frequently. If asthma control is not achieved using one delivery device, it may be beneficial for pt’s to switch to another device or delivery system. Ask “What worries you the most about your asthma medications?”.
• Pediatric pt’s with asthma, prescribed daily controller medication, frequently miss taking their medication when they should (a median of only 45% of prescribed doses was taken) (J Pediatr 2005;146:157-159,171-182).
• A survey of 200 pt’s found that 50% needed to restrict physical exercise, 33% had used beta-agonists two or more times in the preceding week and 33% were told by their physicians to use controller medication on as-needed basis (Ann Asthma Allerg Immunol 2007;98:322-328)….Cost of tx was cited as the biggest barrier to adherence. Inadequate education in proper controller medication use was not a perceived barrier despite a high frequency of improper use…. patients who have a say in their asthma tx plans may be more compliant with daily controller medication regimens.
• Inner-city asthma sufferers who take herbal remedies tend to have worse symptoms and to use their inhalers less (Ann Allergy, Asthma & Immunology 2010;104:132-138).
Stepwise Approach for Asthma Management:
1. Assessment and Monitoring: Multiple measures of the current level of impairment include frequency and intensity of sx’s, markers of lung function, and limitations of daily activities. Determination of future risk should consider risk for exacerbations, progressive loss of lung function, or adverse effects associated with antiasthma medications. Some pt’s with good daily functioning when evaluated may still be at high risk for frequent exacerbations. F/u Q’s | S/s of asthma | Classification & Level of Control |
2. Pt Education: It is essential to teach pt’s appropriate skills to self-monitor and manage their asthma. A written asthma action plan is needed for each pt, which should include instructions for daily tx as well as strategies to detect and manage asthma exacerbations. Pt’s often remain asymptomatic as the peak flow drops significantly, thus must actively head off exacerbation’s. See Peak Flow Monitoring | The pt’s normal PEFR value is used to construct a personalized “asthma action plan,” which provides specific directions for daily management and for adjusting medications in response to increasing symptoms or decreasing PEFR. Parents of kids with asthma don’t always realize when their children’s treatment is inadequate a drugmaker-funded survey suggests (Eur Resp J 2011;June 23)……”Physicians cannot just ask the parent ‘how is your child doing?’…..found kids whose parents worry about medication side effects are more likely to have poorly controlled asthma……They say this suggests parents need more education about asthma medications.
3. Control of Environmental Factors and Other Asthma Triggers: Isolated measures to limit exposure to allergens and other triggers are seldom sufficient. Asthma control is often improved by treating chronic diseases including rhinitis and sinusitis, gastroesophageal reflux, overweight or obesity, obstructive sleep apnea, stress, and/or depression. See Triggers | See Allergy Module for Eval & Tx of Allergic Disorders |
4. Pharmacotherapy: As in previous asthma guidelines, advocates a stepwise approach to control asthma, increasing medication dosages and types as needed, and decreasing them whenever possible, based on the level of asthma control.
Step 1 = Mild intermittent = Two or less days per week or Two or less nights per month. Pt’s with occasional daytime sx’s of short duration.
Tx with a short-acting beta2 agonists as needed.
Step 2 = Mild persistent = >2days/wk; < once per day or >2 nights per month. These pt’s should have a 2-pronged approach to asthma control. This includes medications to control asthma and prevent exacerbations during the long-term, as well as fast-acting medications to control acute sx’s on an as-needed basis. For all age groups, inhaled corticosteroids are the most effective medication for long-term control. Can also use leukotriene receptor antagonists and cromolyn for long-term control, long-acting beta-agonists as adjunct therapy with inhaled corticosteroids, and omalizumab for severe asthma.
• Tx with Step 1 and low-dose inhaled corticosteroids (preferred tx) or inhaled cromoglycate or leukotriene modifier or theophylline or nedocromil (Tilade). Influenza vaccination should be provided to pt’s with asthma when vaccination of the general population is advised, however, routine influenza vaccination of children and adults with asthma does not appear to protect them from asthma exacerbations or improve asthma control.
• Intermittent symptom-based therapy may be successful in a select group of pt’s with long-standing mild persistent asthma (Mild persistent asthma: Is any tx needed? J Allerg Clinical Imm 2007;118:4).
Step 3 = Moderate persistent = Daily or >1 night/wk. The preferred therapies are either low-dose inhaled corticosteroids + a long-acting inhaled beta agonist or medium dose inhaled corticosteroids. Tx Step 1 and low- to medium-dose inhaled corticosteroids and long-acting inhaled beta2 agonists (preferred tx) or increased dose inhaled corticosteroid or low- to medium-dose inhaled corticosteroid and either a leukotriene modifier or theophylline.
• Reliever medication plus one or two controllers. For adults and adolescents, combine a low-dose inhaled glucocorticosteroid with an inhaled long-acting beta2-agonist either in a combination inhaler device or as separate components. Inhaled long-acting beta2-agonist must not be used as monotherapy. For children, increase to a medium-dose inhaled glucocorticosteroid.
• Patients who have a poor response to asthma treatment are 3 times as likely to also have moderate-to-severe rhinitis (Allergy. 2008;63:564-569)…….Asthma and rhinitis share common physiologic pathways and have been linked as clinical entities…..Between 46% and 100% of patients with asthma also have rhinitis, and up to 33% of patients with rhinitis have asthma.
Step 4 = Severe persistent = Continual or frequent. Where possible, pt’s not controlled on Step 3 tx’s should be referred to a health professional with expertise in the management of asthma.
Tx Step 1 and high-dose inhaled corticosteroid and long-acting inhaled beta2 agonists (preferred tx) and, if needed, systemic corticosteroids.
Step 5 Reliever medication plus additional controller options. Addition of oral glucocorticosteroids to other controller medications may be effective but is associated with severe side effects. Addition of anti-IgE tx to other controller medications improves control of allergic asthma when control has not been achieved on other medications. Fatal & Resistant Asthma |
Stepping Down Tx: when asthma is controlled.
• When controlled on medium- to high-dose inhaled glucocorticosteroids: 50% dose reduction at 3 month intervals.
• When controlled on low-dose inhaled glucocorticosteroids: switch to once-daily dosing.
• When controlled on combination inhaled glucocorticosteroids and long-acting inhaled beta 2-agonist, reduce dose of inhaled glucocorticosteroid by 50% while continuing the long-acting beta 2-agonist. If control is maintained, reduce to low-dose inhaled glucocorticosteroids and stop long-acting beta 2-agonist.
Stepping Up Tx: in response to loss of control. No single treatment regimen is best for all children requiring asthma step-up therapy, according to a randomized crossover study (NEJM 2010;online March 2)..compared 250 µg fluticasone BID salmeterol twice daily + 100 µg fluticasone twice daily; the leukotriene-receptor antagonist montelukast once daily plus 100 µg fluticasone twice daily.
• Rapid-onset, short-acting or long-acting inhaled beta 2-agonist bronchodilators provide temporary relief.
• Need for repeated dosing over more than one/two days signals need for possible increase in controller therapy
• Use of a combination rapid and long-acting inhaled beta 2-agonist (e.g., formoterol) and an inhaled glucocorticosteroid (e.g., budesonide) in a single inhaler both as a controller and reliever is effecting in maintaining a high level of asthma control and reduces exacerbations.
• Doubling the dose of inhaled glucocortico-steroids is not effective, and is not recommended.
**Ref: (National Heart, Lung, and Blood Institute. Published online August 29, 2007. http://www.nhlbi.nih.gov/guidelines/asthma/index.htm) (2009 Update of the GINA Report, Global Initiative for Asthma, http://www.ginasthma.org)
F/u: SEARS:
S: Sx’s: nocturnal (awakening, coughing) in past 2mo?
E: exercise (how doing).
A: absenteeism (school/work): exacerbations frequency/ duration.
R: Rescue inhaler use/ frequency of refills.
S: SE’s of meds. Current peak flow use & personal best peak flow.
Decr Stress –> 15min daily massage. Free educational game for age 7-15 available at www.starbright.org.
• There appears to be an association between mood disturbances or social isolation and incident hospital admissions for asthma (Allergy 2007;62:554-560)…..highlight the potential importance of taking account of psychosocial factors, including availability and quality of support networks, in guiding long-term asthma management.
• A program of breathing and relaxation exercises known as the Papworth method eases the symptom scores (P=0.007), anxiety (P=0.006) and depression (P=0.03), and improved hypocapnic sx’s of asthma significantly — largely without change in underlying lung function (Thorax 2007; doi: 10.1136/thx.2006.076430)…Breathing training consisted of replacing inappropriate use of accessory muscles with diaphragmatic breathing, using nose breathing instead of mouth breathing, relaxation training, and home exercises taught with audiotape or CD with integration of exercises into daily activities.
• Breathing techniques designed to reduce hyperventilation may improve asthma symptoms and reduce medication use in adults with poorly controlled asthma, although the evidence regarding breathing techniques overall appears to be limited (Agency for Healthcare Research and Quality. Online September 10, 2012)….the reviewers described the evidence supporting yoga breathing for asthma relief to be very low……There was minimal evidence to support the use of inspiratory muscle training (IMT). Breathing training may promote relaxation and decrease anxiety and/or autonomic arousal. Breathing training may also directly promote the delayed use of reliever medication, thereby decreasing reliever medication use.
When to Refer: Link: Fatal & Resistant Asthma | Not meeting tx goals after 3-6mo. The pt has required hospitalization or >2 bursts of oral corticosteroids in a year. The adult and pediatric pt >5 yo requires step 4 care or higher or a child <5yo requires step 3 care or higher. Any pt on daily inhaled steroids and still requiring daily beta-adrenergic agonists. Complex or severe persistent asthma or moderate-severe asthma not controlled with inhaled medications. The pt experienced a life-threatening asthma exacerbation (ICU admission). Atypical or comorbidity such as GERD, COPD, congenital pulmonary anomalies, heart dz, nasal polyposis, chronic sinusitis, severe rhinitis, allergic bronchopulmonary aspergillosis, COPD, vocal cord dysfunction. The diagnosis of asthma is uncertain. Needing additional diagnostic tests are needed (skin testing for allergies, bronchoscopy, complete pulmonary function tests). If the pt is a candidate for allergen immunotherapy. There appear to be occupational triggers. Pt’s in whom significant psychosocial or psychiatric problems are interfering with asthma management.
Prognosis: About two thirds of children with asthma at a young age are likely to continue to have asthma as adults, 1/3 appear to outgrow their asthma (BMJ 2003;326:422-3). In children who develop asthma-like sx’s in the preschool years, patterns of wheezing and lung function are established by age 6 years and do not change much by age 16 (Am J Respir Crit Care Med 2005;172:1253-1258). Children who “outgrow” early wheezing may have a relapse in midlife (Ann Allergy Asthma Immunol. 2007;98:337-343)…relapse of wheezing illness in adults may be affected by atopy and cigarette smoking. Data for 34,216 children who were born in 1994 and were diagnosed with asthma before age 6 years indicates that about half the children had persistent asthma, defined as any hospitalization or physician visit for asthma from age 6 to 12 years (Arch Pediatr Adolesc Med 2007;161:1197)….Factors that were significantly associated with persistent asthma were older age at diagnosis, male sex, greater use of health services during the first year after diagnosis, atopic conditions before age 6, living in an urban area, and lower birth weight. Data from 34,216 children found that those who required little or no additional care during the year after they received diagnoses of asthma were most likely to be in remission by age 12 (Arch Pediatr Adolesc Med 2007;161:1197)….children who were hospitalized for asthma during that year were 3 times more likely to have persistent disease, and children who had at least four asthma-related physician visits were 2.6 times more likely to have persistent disease. Asthma morbidity improves as children get older, but most school-age children with persistent asthma will have symptoms during adolescence (J Allergy Clin Immunol 2010;125:359.e3).
ASTHMA IQ: An evidence-based online system for improving the way clinicians care for asthma patients was launched here by the American Academy of Allergy, Asthma, and Immunology. The system aims to help in matching the best treatments to individual patients on the basis of symptoms and risk factors using the latest guidelines. Can be accessed at www.asthmaiq.org. Although registration and full access are currently available only to AAAAI members as of 3/08.
Links: Quick relief | Systemic Corticosteroids | Long-term “Control” Meds | Combo’s | Theophylline | Nebulized | MDI Use | Spacers | Nebulizer | Dry Powder Use | Acute Exacerbations |
Quick Reliever Meds:
Short acting beta-agonists, anti-cholinergic, systemic glucocorticoids. Albuterol | Levalbuterol | Terbutaline | Anticholinergics | OTC | Omalizumab | Nebulizer |
Controller Meds:
Glucocorticoids (PO and MDI), cromolyn, long-acting beta agonist, methylxanthines, anti-leukotrienes. Combination of meds is best. Oral Albuterol | Oral Metaproterenol | Long-Acting Beta2 Agonists | Formoterol (Foradil) | Salmeterol (Serevent) | Leukotriene Modifiers: Singulair (Montelukast), Accolate (Zafirlukast), Zyflo (Zileuton) | Mast Cell | Inhaled Corticosteroids | Combo Agents & Tiotropium (Spiriva), Tudorza (Aclidinium) & Xolair (Omalizumab) | Theophylline | Other Agents: Xolair (Omalizumab), Halothane, Bronchial Thermoplasty, Alternative Meds etc |
All inhalers containing chlorofluorocarbons (CFCs) were banned in the United States beginning in 2009.
General Age Requirements for Correct Use:
Breath-actuated MDI –> >5 yo.
Dry powder inhaler –> >5 yo.
MDI –> >5 yo.
MDI with chamber –> >4 yo.
MDI with chamber and mask –> <4 yo.
MDI with endotracheal tube –> Neonate.
Small-volume nebulizer –> <2 yo. Aerosolized medication delivery systems, when used with comparable drug doses, provide equivalent efficacy (Chest. 2005;127:335-371).
Taking the wrapper off & Expiration: Many patients don’t realize how fast their inhalers expire once they remove the foil wrapper that protects them from moisture. Once the inhaler is removed from the wrapper the expiration date on the box no longer applies. Advair Diskus is good for only one month after opening, Serevent for only 6 weeks, and Symbicort for only 90 days (Prescriber’s Letter 2009;25(9):250901). Different sizes of the same brand have different expiration dates after opening. Ventolin HFA 60-count is good for 12 months but the 200-count version has a 6-month expiration date. Advise patients to check the expiration date on the Rx label if their inhaler doesn’t seem to be working as well. If a patient will only need to use an inhaler infrequently, try ProAir HFA and Proventil HFA albuterol inhalers as they aren’t wrapped in foil and are good for up to 2 years. Advair HFA is good for 18 months vs one month for Advair Diskus.
Inhalers that expire quickly once the foil overwrap is removed:
Ventolin HFA (200 inhalations): 6 months.
Ventolin HFA (60 inhalations): 12 months.
Symbicort: 3 months.
Serevent Diskus: 6 weeks.
Advair Diskus: 1 month.
Asmanex Twisthaler: 45 days.
Foradil: 4 months.
Flovent Diskus 50 mcg: 6 weeks.
Flovent Diskus 100 and 250 mcg: 2 months.
Cost of Meds in 2013:
Inhaled Anticholinergics
Ipratropium / Atrovent HFA metered-dose inhaler 17 mcg/inhalation at 2 inhalations 4 times daily as needed $90.53
Generic nebulizer 250 mcg/mL at 500 mcg 4 times daily as needed $176.40
Tiotropium (Spiriva HandiHaler) dry-powder inhaler 18 mcg/capsule once daily $139.78
Inhaled Beta-2 Agonists
Short-acting (100 doses):
Albuterol HFA MDI 90 mcg/inhalation at 2 inhalations every 4-6 hours as needed
ProAir HFA $33.92
Proventil HFA $41.34
Ventolin HFA $36.18
• Albuterol sulfate nebulizer 1.25-5 mg every 4-8 hours as needed (0.63-2.5 mg in children aged 2-4 years)
Generic single-dose vials 2.5 mg base/3 mL $159.00
Generic multi-dose vials 2.5 mg base/0.5 mL $17.00
AccuNeb single-dose vials 0.63 or 1.25 mg base/3 mL $183.00
Levalbuterol tartrate (Xopenex) nebulizer 0.31, 0.63, or 1.25 mg/3 mL at 0.63-1.25 mg (0.31-0.63 mg in children ages 6-11 years) 3 times daily every 6-8 hours $393.00. (Xopenex HFA) MDI 45 mcg/inhalation 2 inhalations every 4-6 hours as needed $52.50
Pirbuterol (Maxair Autohaler) CFC MDI 200 mcg/inhalation at 2 inhalations every 4-6 hours as needed $57.96
Long-acting (30 days):
Arformoterol (Brovana) nebulizer 15 mcg/2 mL at 15 mcg twice daily $380.99 (Treat Guidel Med Lett 2007 Nov;5(63):95 TOC)
Formoterol (Foradil Aerolizer) DPI 12 mcg/capsule at 12 mcg twice daily $145.80
Formoterol (Perforomist) nebulizer 20 mcg/2 mL at 20 mcg twice daily $334.80 (Treat Guidel Med Lett 2007 Nov;5(63):95 TOC)
Aalmeterol (Serevent Diskus) DPI 50 mcg/blister at 50 mcg twice daily $153.00
Inhaled Corticosteroids
Beclomethasone dipropionate (QVAR) HFA MDI 40 or 80 mcg/inhalation at 40-320 mcg twice daily (40-80 mcg twice daily in children aged 5-11 years) $71.25
Budesonide / Pulmicort Flexhaler DPI 90 or 180 mcg/inhalation at 360-720 mcg twice daily (180-360 mcg twice daily in children aged 6-17 years) $134.88
Pulmicort Respules 0.25, 0.5 or 1 mg/2 mL ampules at 0.25-0.5 mg once or twice daily or 1 mg once daily FDA approved for children aged 1-8 years $183.00
Ciclesonide (Alvesco) HFA MDI 80 or 160 mcg/inhalation at 80-320 mcg twice daily for adults or children > 12 years old $139.08
Flunisolide (AeroBid) CFC MDI 250 mcg/inhalation at 500-1,000 mcg twice daily (500 mcg twice daily in children aged 6-15 years) $90.51
Fluticasone propionate / Flovent Diskus DPI 50 mcg/blister at 100-500 mcg twice daily (50-100 mcg twice daily in children aged 4-11 years) $187.20
Flovent HFA MDI 44, 110 or 220 mcg/inhalation at 88-440 mcg twice daily (88 mcg twice daily in children aged 4-11 years) $95.82
Mometasone furoate (Asmanex Twisthaler) DPI 110 or 220 mcg/inhalation at 220-440 mcg once daily or 220 mcg twice daily (110 mcg once daily in children aged 4-11 years) $113.92
Triamcinolone acetonide (Azmacort) HFA MDI 75 mcg/inhalation at 150 mcg 3-4 times daily or 300 mcg twice daily (maximum 1,200 mcg/day) (75-150 mcg 3-4 times daily or 150-300 mcg twice daily [maximum 900 mcg/day] in children aged 6-12 years) $145.20
Combination Short-Acting Beta-2 Agonist/Short-Acting Anticholinergic:
Albuterol sulfate/ipratropium (Combivent) metered-dose inhaler 90 mcg/18 mcg/inhalation at 2 inhalations 4 times daily as needed $100.19
Albuterol sulfate/ipratropium (DuoNeb) nebulizer 2.5 mg/0.5 mg/3 mL at 3 mL 4 times daily as needed (maximum 6 doses/day) $234.00
Combination Inhaled Steroid/Long-Acting Beta-2 Agonist:
Budesonide/formoterol (Symbicort HFA) MDI 80 or 160 mcg/4.5 mcg/inhalation at 2 inhalations twice daily (only FDA-approved for treatment of asthma) $162.08
Fluticasone/salmeterol (Advair Diskus) DPI 100, 250 or 500 mcg/50 mcg/blister at 1 inhalation twice daily $172.80
Fluticasone/salmeterol (Advair HFA) MDI 45, 115 or 230 mcg/21 mcg/inhalation at 2 inhalations twice daily $174.24
Anti-IgE antibody: Omalizumab (Xolair) 150-300 mg subcutaneously every 4 weeks or 225-375 mg subcutaneously every 2 weeks $559.87 per 150 mg vial
Cromolyn sodium: Generic cromolyn sodium 10 mg/mL for nebulization at 20 mg 3-4 times daily $100.80
Leukotriene modifiers:
Montelukast (Singulair) 10 mg orally once daily in the evening (4-5 mg in children > 1 year old) $117.30
Zafirlukast (Accolate) 20 mg orally twice daily (10 mg twice daily in children aged 5-11 years) $101.40
Zileuton (Zyflo CR) 1,200 mg orally twice daily in adults and children > 12 years old $162.08
Oral corticosteroids:
Methylprednisone 7.5-60 mg every other day or 40-60 mg/day for 3-10 days, generic $59.30, Medrol $68.20
Prednisolone 7.5-60 mg every other day or 40-60 mg/day for 3-10 days, generic tablets $10.40, generic syrup $30.80, Orapred solution $109.20, Orapred ODT disintegrating tablets $114.50, Pediapred solution $120.00, Prelone syrup $71.40,
Theophylline (oral): theophylline extended-release tablets. Generic tablets at 300-600 mg/day $18.00. Uniphyl (400 or 600 mg) at 400-600 mg once daily $41.40. Theo-24 (100, 200, 300, or 400 mg) at 300-600 mg once daily $33.00 (entire 24-hour dose released in 4-hour period if taken with food)
Links: Albuterol | Levalbuterol | Terbutaline | Anticholinergics | OTC | Omalizumab | Nebulizer | Acute – Severe Exacerbations | See MDI Use | Spacers | Dry Powder Use |
If bronchodilator therapy does not improve sx’s and airflow within minutes to hours in asthmatics, consider pneumonia, emphysema or CHF. Continuous prophylactic bronchodilators w/o sx’s should not be encouraged as tolerance will build to the quick relief meds. None are these are considered by the FDA to be pharmaceutical equivalents even thought they contain the same active ingredients.
• Exclusive and heavy use of short-acting beta-2 adrenergic receptor agonists may double the risk of primary cardiac arrest in asthmatics (Am J Med 2002;113:711-716).
• Long-term albuterol (1yr) use is well tolerated and does not lead to deterioration of lung function according to a study with 746 patients with asthma with an average use of less than 0.6 puffs per day (Ann Allergy Asthma Immunol 2007;99:540-548).
• Inhaled albuterol (Proventil) brought faster increases in asthma patients’ lung function than did two corticosteroid-beta agonist combination agents, but the budesonide-formoterol (Symbicort) combination was significantly faster than fluticasone-salmeterol (Advair) (J Aller Clin Immun 2008;121:S220-S221)…..Some 51% of patients receiving albuterol showed at least 15% improvement in FEV1 values within 15 minutes of dosing, versus 40% of patients taking the budesonide-formoterol combination (P<0.05) and 18% of patients treated with fluticasone-salmeterol (P<0.05).
• Greater use of a short-acting beta-agonist is associated with an increased frequency of asthma exacerbations and this is especially the case for home use of nebulizers (Ann Allergy Asthma Immunol 2008;101:482-487)…..over a 3-month period, short-acting beta-agonist medication use via a nebulizer was associated with an increased risk of an asthma-related emergency department visit (hazard ratio, 6.32) and of asthma-related hospitalization (hazard ratio, 21.6).
Albuterol MDI (Proventil, Ventolin, Salbutamol)(Racemic): [$30, name brand Vs $11 for a generic, 90 mcg/actuation, 200 actuations/inhaler, 17 g] 1–2 puffs (90–180 mcg) Q4–6 hr PRN or 5min prior to exercise. Adult NEB @1.25-5mg (0.25-1ml) in 2-3ml NS. Child NEB @ 0.05mg/kg (minimum of 1.25mg, max 2.5mg). Short acting beta-agonist. SE: skeletal muscle tremor, decr K, incr lactic acid, H-A, hyperglycemia. Can give at 10-20 puffs q1-2hr, then q4hr if severe exacerbation. Regular use for >1wk of b-2 agonists results in tolerance to both the bronchodilator and nonbronchodilator effects and may be associated with poor disease control (Ann Int Med 2004;140:802-13). Oral Albuterol | Meds |
Dry powder (Ventolin Rotocaps): [200 µg/capsule] 1-2 q4-6 hours as needed. $37.92/100 200-µg capsules. Rotohaler required for inhalation..
Albuterol HFA: [all have 90 mcg/ actuation, 200 puffs/ actuation, $29-$44] non-chlorofluorocarbon (CFC-Free) approved in 3/05 as other to be phased out by 2009. All recommend washing the plastic actuator weekly and air-dry. Differ in priming. Tell pt’s that even though HFA inhalers may not “feel” like they are working as well, they are….the softer spray still delivers the correct amount of drug. They may need to wash the actuator with warm water once a week to prevent clogging.
Ventolin HFA: $30. Prime before first use with 4 sprays and after 2 weeks on non-use with 4 sprays and with 1 spray after dropped or washed. Initially the only MDI with built-in counter. Has same spray force and volume at older MDI’s (>55 milliNewtons). Green house, black cap.
Proventil HFA: $38. Prime before first use with 4 sprays and after 2 weeks on non-use with 4 sprays. Yellow house, orange cap. The Proventil brand of HFA-driven albuterol inhalers may be more prone to clogging than other brands if not washed regularly (ACAAI Meeting 2008; Abstract 3). Has an intermediate spray force (41 milliNewtons).
ProAir HFA: $34. Prime before first use with 3 sprays and after 2 weeks on non-use with 3 sprays. Red house, white cap. Has a weak spray force (15 milliNewtons). Built-in dose counter added in 1/2013.
Levalbuterol MDI (Xopenex HFA): [45 mcg/ actuation, 200 actuation /canister, $44] FDA approved in 3/05 for pt’s >4yo with reversible obstructive airway disease. R-isomer only (possibly less tremor and nervousness, less cardiovascular SE’s than racemic albuterol). Possible longer duration of bronchodilation. Prime before first use with 4 sprays and after 3 days on non-use with 4 sprays. Light blue house, marroon cap. Also in NEBS via unit dose vial of 0.63mg (= 2.5mg Albuterol) and 1.25mg for NEB.
• Xopenex HFA if not a first-line alternative, it’s more expensive than albuterol inhalers and it isn’t more effective nor better tolerated….There is no evidence that levalbuterol is any safer that albuterol regarding hospitalizations, increased heart rate or pulmonary inflammation (Prescriber’s Letter 2007;23(11):231101).
• Levalbuterol appears to be no more effective and offers no improvement in the side-effect profile compared with albuterol MDI (STEPS. New Drug Reviews. Am Fam Physician 2007;75:234).
• For continuous bronchodilator therapy, racemic albuterol and levalbuterol achieve similar outcomes according to a RCT on 81 children (age range, 6–18 years; 93% black) with acute asthma exacerbations who required continuous nebulized bronchodilator treatment despite 1 hour of treatment with intermittent nebulized racemic albuterol, nebulized ipratropium, and systemic corticosteroids.(J Pediatr 2009;155:205.e1)……clinical outcomes — including time to meet discharge criteria, heart rate, and clinical asthma scores — were similar in the two groups. Link: Nebulizer | Meds |
• Levalbuterol is not anymore beneficial than Albuterol in critically ill patients (Chest 2011;140:1466)…..On average, patients’ heart rates rose by <1 beat per minute after administration of either medication.
Pirbuterol (Maxair Autohaler, 400 puffs/canister): 200ug/puff, 2 puffs TID-QID PRN. $90.
Bitolterol (Tornalate): 200ug/puff, 2 puffs TID-QID PRN. Also in NEB as 0.2% soln (Tornalate)
Metaproterenol (Alupent, Metaprel): 2-3 puffs q2-3hr, max 12/d MDI. Also in tab, syrup and neb forms.
Terbutaline (Brethaire, Brethine, Bricanyl): Injection @ 0.25mg SQ into lateral deltoid, can repeat in 15-30min (max 0.5mg q4hr). Also in tabs at 2.5mg & 5mg PO TID q6hr (not quick relief). No longer in MDI, was 200ug/puff @ 2 puffs TID-QID PRN.
Asthmanefrin: An OTC chlorofluorocarbon (CFC)-free epinephrine inhaler in 2012. It will help fill the void left when Primatene Mist was discontinued in 2011 because of its CFC propellant, the manufacturer says.
Epinephrine MDI (Primatene Mist): the only nonprescription (OTC) inhalers available in the U.S. for asthma. May be pulled from the marked as they contain CFCs as propellants pPer the FDA in 9/07 inhalers that contain CFCs would be removed from the market by the end of 2010. Epinephrine, a mixed alpha-beta agonist, is no longer a part of practice guidelines for asthma management as might have more adverse effects on the cardiovascular system than pure beta-agonists (Status of OTC epinephrine inhalers. Prescriber’s Letter 2006;22(3):220311). For temporary relief of occasional sx’s of mild asthma.
Note: Some pt’s with corn allergy or sulfite hypersensitivity raise concerns about the new albuterol HFA inhalers because they contain ethanol…reasure them that it is distilled and purified to the extent that even if made from corn. But if they are still concerned, consider switching them to Ventolin HFA…it doesn’t contain ethanol.
Link: Atovent | Combivent – Respimat | See Tiotropium (Spiriva) & Tudorza (Aclidinium) | Meds | Patients with COPD who used inhaled anticholinergic agents [ipratropium (Atrovent or Combivent) and tiotropium (Spiriva)] for at least a month, compared with controls who took placebo or other inhaled agents, showed a significant 58% independent increase in risk of cardiovascular (CV) death, myocardial infarction (MI), or stroke in a 17-trial meta-analysis (JAMA. 2008;300:1439-1450). Their risk of CV death alone jumped 80%, although such events were few in the populations studied…….increased risk for MI with a number needed to harm of 174 per year and an increased risk for CV death with a number needed to harm of 40 per year.
• Ipratropium used for COPD is associated with the risk for all-cause and cardiovascular death, according to the results of a nested case-control study with 32,130 case patients and 320,501 controls (Ann Intern Med. 2008;149:380-390)……For all-cause mortality, adjusted odds ratios (ORs) were 0.80 for inhaled corticosteroids, 1.11 for ipratropium, 0.92 for long-acting beta-agonists, and 1.05 for theophylline……ipratropium was linked to a greater risk for cardiovascular deaths (OR, 1.34), inhaled corticosteroids were associated with a lower risk for cardiovascular death (OR, 0.80).
Ipratropium (Atrovent) [$72] 2-6 puffs q6-8hr (max 24puff/24hr) or beta-2 agonist 2 puffs q4-6hr PRN. (18ug/puff), NEB 0.025% (0.25mg/ml) QID. Non selectively inhibits all 3 muscarinic receptors (M1, M2, M3).
• May be adjunctive therapy to B-agonists in acute asthma. Also in patients intolerant to B-agonists. Tx of choice for b-blocker-induced bronchospasm.
SE: dry mouth, blurred vision if get in eyes, incr wheeze in some pt’s. May cause pharyngeal irritation. Caution if glaucoma, BPH or bladder neck obstruction. In 11/08 the FDA approved safety labeling revisions for ipratropium bromide such that patients should be cautioned to avoid spraying the inhalation aerosol into their eyes and are advised that doing so may result in precipitation or worsening of narrow-angle glaucoma, mydriasis, increased intraocular pressure, acute eye pain or discomfort, temporary blurring of vision, and visual halos or colored images in association with red eyes from conjunctival and corneal congestion. In 11/08 the FDA warned that ipratropium plus albuterol inhalation aerosol should be used in pregnancy only if the potential benefit to the mother justifies fetal risk. Although no animal studies have been conducted with the combination product, a 4.5% rate of cleft palate formation was observed in rodents receiving doses equivalent to the maximal recommended human dose of albuterol.
• A VA cohort study to examine cardiovascular risk among almost 83,000 COPD patients found that exposure to ipratropium was associated with 30% greater risk for adverse cardiovascular events than was no exposure (Chest 2010;137:13)……For now, many experts believe that patients can reasonably continue to use anticholinergic inhalers if their symptoms clearly improve with these agents.
• Inhaled anticholinergics may increase the risk of community-acquired pneumonia in asthma patients according to a case-control study (Eur Respir J 2010;09031936.00022909v1)…..Among asthma patients, 5% in the pneumonia group and 1% in the control group had used an inhaled anticholinergic……..The use of ipratropium bromide was associated with an adjusted OR of 8.8 for pneumonia (p=0.048).
• Pneumococcal vaccine had a significant protective effect (OR, 0.35). Elderly men taking inhaled anticholinergic drugs for COPD face increased risk for acute urinary retention (Arch Intern Med 2011;May 23)….The authors advise that patients “may benefit from close monitoring for … impending urinary retention within the first month” of starting the drugs.
• Inhaled anticholinergics are associated with increased risk for arrhythmia (odds ratio, 1.56) in children and young adults with asthma, according to a case-control study (American Thoracic Society meeting. May 2012, http://conference.thoracic.org/2012/)…..Ipratropium conferred the highest risk.
Atrovent HFA (ipratropium bromide HFA): [17 mcg/puff, 200 puffs/canister, $94] FDA approved in 11/04, provides a therapeutic benefit comparable to Atrovent (ipratropium bromide) (CFC) Inhalation Aerosol. CFC-Free breath-activated meter. SE: dry mouth (1.6%) and bitter taste (0.9%). The new Atrovent HFA inhaler does not have soy as thus is no longer contraindicated in patients allergic to peanuts (cross reactive)(Prescriber’s Letter 2009;25(6):250601)…..Combivent (ipratropium/albuterol) inhalers still have soy lecithin…but a new version without soy is in the works.
Tiotropium (Spiriva): see long-term control, SEE Tiotropium (Spiriva) |.
Combivent Respimat (Ipratropium bromide and albuterol sulfate inhalation spray): One spray QID. $250 for 30 days of treatment. Open cap, twist unit then push release button…..Delivers a slow moving soft mist (that is similar to a nebulizer) over 1.5 seconds. A CFC-propellant-free inhaler device that relies on a mechanical spring to generate a slow-moving cloud of medicine. The original Combivent is phased out at the end of 2013. FDA approved in 10/2011 for patients with COPD who use a regular aerosol bronchodilator, but continue to have evidence of bronchospasm and require a second bronchodilator. Not contraindicated in patients with soybean or peanut allergy…unlike the old Combivent.
• Patients with COPD experience few adverse events and discontinuations when treated with an ipratropium plus albuterol inhalation spray (CVT-R; Combivent Respimat, Boehringer Ingelheim) than when treated with the same drug formulated as a metered-dose inhaler (CVT-MDI), according to a large randomized controlled trial (CHEST 2012: American College of Chest Physicians Annual Meeting. Presented October 24, 2012)…..CVT-MDI “is the last metered-dose inhaler on the market that has been given a waiver to allow CFC]”…..”CVT-MDI is being phased out and will not be available for sale after December 2013.”
Combivent (18 mcg Ipratropium + 90 mcg albuterol MDI): [18 mcg/90 mcg, 200 puffs/canister, $250] Adults @ 2-3 puffs q 6 hours (max 12 inh/d). Ped @ 1-2 puffs q 8 hours. Contra: atropine, soybean, lecithin, peanut or related allergy. Atrovent & Combivent (ipratropium) MDI’s contain soy lecithin as a suspending agent (not in the nasal or NEB), thus a contra to anyone with a peanut allergy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








