Chapter 8 Arthrodesis and Fusion for the Treatment of Discogenic Neck and Back Pain
Evidence-Based Effectiveness and Controversies
 A careful and detailed patient history and physical are key to understanding the mechanism and physiology of pain.
A careful and detailed patient history and physical are key to understanding the mechanism and physiology of pain. Determining the discs responsible for pain based on imaging studies alone is inaccurate, as degeneration of multiple levels is common with age.
Determining the discs responsible for pain based on imaging studies alone is inaccurate, as degeneration of multiple levels is common with age.Introduction
Neck and back pain are common conditions that affect millions of people each year. Neck pain is reported to occur in as many as 66% of individuals at some point during their lifetime.1 With the widespread use of magnetic resonance imaging (MRI), patients are increasingly being diagnosed with degenerative disc disease, prompting referrals to surgeons and pain management physicians. The clinical significance of these degenerative findings is often overstated by physicians and patients alike, leading to a cascade of interventions and treatments that may not improve their symptoms.
Similarly, low back pain is among the leading reasons for individuals to seek medical attention. One out of 17 patients seen by general practitioners presents with low back pain, and approximately 31 million patient visits for back pain occur in the United States annually.2 It is estimated that 70% to 85% of individuals will suffer an acute episode of low back pain in their lifetime. Although most experience near complete resolution of symptoms within several weeks, a small percentage continue to experience persistent or chronic low back pain.3
Persistent low back pain is a significant source of anxiety, distress, depression, and disability that affects not only the individual, but society. It is estimated that 28% of the working population in the United States will be disabled by back pain at some time during their professional life, with approximately 8% of the entire work force disabled in a given year.3 This is a troublesome statistic since back pain is the primary cause of disability in persons less than 50 years of age, often the most productive years in a lifetime. The total socioeconomic burden of back pain, including both health care costs and lost wages, is estimated at $100 to $200 billion annually, with two thirds of this cost the result of work-related disability.4 Of alarming concern is that, although the incidence of diagnosed chronic back pain has been stable for 30 years, the rate of disability claims has increased by 14 times that of population growth.5
Despite the lack of evidence, fusion for discogenic pain is being performed more often, and reports of successful outcomes stem mostly from small retrospective case series.6–9 Approximately 300,000 spinal fusions are performed annually in the United States, an increase of 220% between 1990 and 2001. Of these fusion operations, approximately 75% are performed for degenerative disc disorders. National inpatient data sample identifies degenerative disc disease as the diagnosis accounting for the largest increase in lumbar fusions during this period.5
Critics of fusion surgery argue that current imaging and functional diagnostic modalities do not accurately identify the source of pain in most patients who lack evidence of nerve compression or neurological deficit.10 Further, the relationship between arthrodesis and pain relief remains equivocal. Despite advancements in surgical technology, instrumentation, and osteobiologics, clinical outcomes continue to lag behind fusion rates. This lack of correlation between rates of arthrodesis and pain improvement is an argument against arthrodesis for discogenic pain.
Pathophysiology of Discogenic Pain
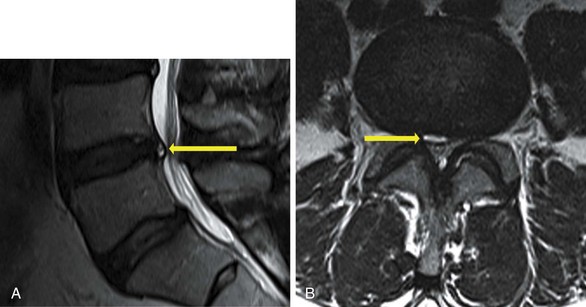
With aging, the disc gradually becomes less hydrated, and the concentration of proteoglycans decreases. Normal disc metabolism shifts toward catabolic processes that further deplete proteoglycans and lead to increased matrix degeneration. As a result, the disc becomes progressively dysfunctional as the nuclear material is replaced by desiccated fibrocartilaginous material. Loss of fluid results in decreased hydrostatic pressure as a mechanism for effective load transference. Thinning or microfracture of the endplates can occur, and subsequent loss of endplate vascularity reduces transport of nutrients and waste products out of the disc. With cyclical loading of the degenerated disc, radial fissures or cracks propagate through the annulus with migration of nuclear material peripherally (Fig. 8-1, A). With complete annular disruption, disc material can herniate into the central canal or foramen (Fig. 8-1, B). These degenerative processes are estimated to occur in 90% of normal individuals by 50 years of age.10
In 1970 Crock11,12 first associated back pain with the pathophysiological process of disc desiccation and subsequent radial fissure formation of the annulus. He termed this entity internal disc disruption. It was characterized by the progressive disruption of the internal architecture of the disc while essentially maintaining the external shape such that nerve root compression did not occur. Crock hypothesized that pain was generated when degradation of the disc matrix causes release of inflammatory cytokines, which then migrate through the disrupted inner annular fibers to irritate the high concentration of sensory nerve endings in the outer annulus. His conclusion was supported radiographically by the relative absence of any nerve root compression and the high correlation of concordant pain in discs that exhibited severe radial fissures with intradiscal contrast injection.
Since then several theories regarding the relationship between degenerative disc disease and pain generation have been developed. The mechanical theory suggests that degeneration results in alteration in the biomechanical properties of the disc. As the disc degenerates and the annulus becomes disrupted, increasing instability occurs at the motion segment. Therefore with normal physiological loading the motion segment responds with excessive compression, bending, or rotation, which can trigger pain transmission in surrounding nociceptors. CT and MRI studies have quantified the response of the lumbar spine to rotatory torque and have correlated increased axial rotation in degenerated discs with pain provocation on discography.13,14
Diagnostic Controversies
Neck Pain
Although imaging studies often reveal degenerative changes, including disc desiccation, loss of disc space height, and osteophyte formation, these findings usually involve multiple levels and do not localize to a single disc. Moreover, as many as 85% of asymptomatic individuals over 60 years of age exhibit degenerative changes in their cervical discs on MRI.15,16
Controversy regarding the validity of diagnostic testing techniques, including MRI and discography, for cervical discogenic pain continues to appear in the literature.17,18 Cervical discography has been used by clinical practitioners in select cases as a provocative study to evaluate suspected discogenic pain.19,20 Despite its enthusiasts, many have questioned the validity of discography for this application.17 It has been argued that the specificity of discography is dramatically affected by the psychological profile of the patient.17,21 Some propose that discography is not helpful in identifying the pain source or determining the predictive value of surgery.22–25
Conversely, there are authors who argue that discography can be used effectively in determining the source of a patient’s pain.26–28 Grubb and Kelly28 reviewed their experience with cervical discography during a 12-year period and suggested that a reliable pattern of pain was produced by stimulation of each cervical disc. They reported a high percentage of patients who demonstrated multiple discs responsible for their axial neck pain.
Back Pain
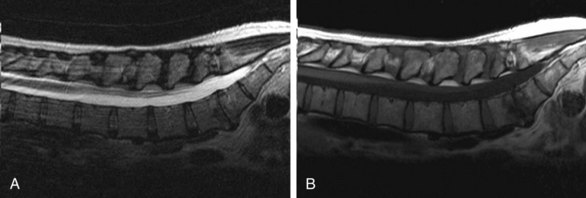
Imaging findings are also generally nonspecific. Plain radiographs may show decreased disc height and sclerotic endplates (Fig. 8-2, A). Sclerotic endplates or bone-on-bone appearance is commonly seen with severely degenerated discs (Fig. 8-2, B). MRI may demonstrate dehydrated, desiccated, or collapsed discs (Fig. 8-3, A). However, these changes may occur in multiple discs, making it difficult to determine which level is symptomatic. Because of its sensitivity for visualizing soft tissue structures of the spine, including the discs, ligaments, joints, and neural elements, MRI is the preferred test to evaluate for nerve root compression from degenerative disc disease. The ability of MRI to detect loss of water content and disc desiccation has led to widespread use of this imaging modality. It also characterizes the effect of disc degeneration on the adjacent endplates and vertebral bodies. In the early phase the normal vertebral body bone marrow is replaced with vascularized fibrous tissue as a reparative response to injury (Fig. 8-3, B). With chronic degeneration the normally red bone marrow is converted to yellow marrow as the marrow elements are replaced by fat cells, which appears to represent a chronic, stable state. Despite these findings, these changes commonly occur in asymptomatic individuals, calling into question their clinical relevance.
Certain studies have demonstrated that positive discography reliably predicts positive surgical outcomes. Simmons and Segil27 studied patients who had discography before undergoing lumbar discectomy, discectomy and fusion, or fusion alone. They found that preoperative discography demonstrated 82% diagnostic accuracy in identifying the symptomatic level. However, this study represented a heterogenous patient population, including not only patients with back pain, but those suffering from herniated discs and nerve root compression. Colhoun and associates29 found that, among patients undergoing lumbar fusion, 89% of those with a positive preoperative discogram had significant improvement after surgery, including decreased pain, return to work, and cessation of analgesics.29 Alternatively, patients with nondiagnostic preoperative discography had a lower rate of success after lumbar fusion, with only 52% of patients reporting a similar satisfactory postoperative outcome.
Varying degrees of success with preoperative discography have been observed. Positive clinical outcomes have been demonstrated in 64% to 86% of patients with positive discography who undergo anterior lumbar interbody fusion (ALIF).30–32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree