Approach to Common Problems of the Foot and Ankle
Richard J. de Asla
Ann H. Johnson
John Kwon
Christopher P. Chiodo
Primary physicians are often consulted for advice and help regarding problems of the foot and ankle, which are extremely prevalent and can be incapacitating. Although some patients require orthopedic referral for more detailed investigation and treatment, many can be cared for by the nonspecialist physician who is knowledgeable about the diagnosis and treatment of common foot and ankle disorders and the indications for referral.
Disorders of the foot are a major cause of frustration and disability. Although often idiopathic or the result of normal activity, foot pain can also be precipitated by structural deformity or systemic disease. Environmental factors, such as shoe type and weight-bearing surface, can also lead to the development and progression of symptoms.
The human foot has 26 bones, comprising one fourth of those in the entire skeleton, along with 100 or more ligaments, 12 extrinsic muscle insertions, and 19 intrinsic muscles. During gait, more than two times the force of body weight is borne by the foot. In normal gait, the foot assumes several roles, including that of a shock absorber, a mobile adapter to accommodate uneven surfaces, and a rigid lever to propel the limb. Limitation or excess of these primary functions places the foot at risk for acquired mechanical trauma. Classification by anatomic region (Table 154-1) helps to guide
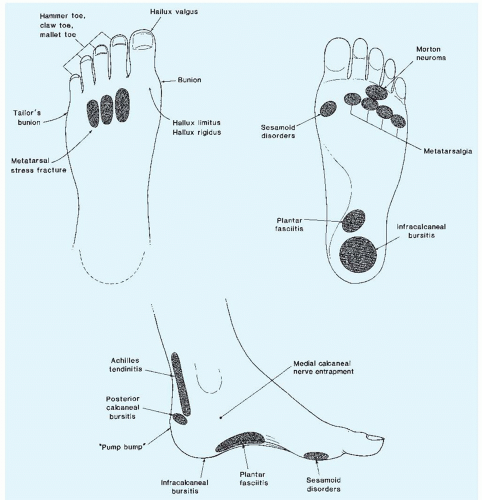
assessment. Office assessment is facilitated by familiarity with the location and manifestations of common foot problems (Fig. 154-1).
assessment. Office assessment is facilitated by familiarity with the location and manifestations of common foot problems (Fig. 154-1).
TABLE 154-1 Common Causes of Foot Pain | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Toe and Forefoot Problems: Painful Toe Deformities
Toe Deformities: Corns
Disorders of the toes are usually related to deformities, most commonly hammer toes, mallet toes, and claw toes. Pain with or without development of a corn (clavus) is usually the primary complaint. Toe contractures develop secondary to compensatory muscle imbalances that result from years of wearing inappropriate shoes and/or from inherited foot abnormalities. The contractures can be flexible or become rigid. Wearing shoes, either prescription or commercial, that provide adequate room in the toe box is the first line of treatment. If the contractures are flexible, over-the-counter splints and pads may be helpful. In persistent or progressive disease, corrective surgery may be necessary if pain compromises daily activity.
Disorders of the First Metatarsophalangeal Joint
The most prevalent disorder of the first metatarsophalangeal (MTP) joint is a hallux valgus deformity, or bunion. Hallux rigidus can also be a problem.
Hallux Valgus: Bunions.
These usually present as painful swelling on the dorsomedial aspect of the first metatarsal head, associated with lateral angulation of the great toe. Although the deformity or difficulty with shoes may be the presenting complaint, patients frequently present with secondary problems, such as hammer toes or pain underneath the other metatarsal heads (metatarsalgia). Narrow shoes, hindfoot malalignment (pronation), and heredity are all believed to contribute, particularly in women. The deformity is also seen in patients with rheumatoid arthritis and other inflammatory arthropathies.
On physical examination, there is tenderness over the inner side of the first metatarsal head; an inflamed bursa may also be present. The great toe is angulated laterally, and at times, the MTP joint cannot be passively reduced. Radiographs may show the underlying cause to be an increased angle between the first and second metatarsals (normal, <10 degrees).
Most bunions respond to nonoperative treatment. Appropriately sized shoes (with wide toe boxes), bunion splints, and orthotic devices provide symptomatic relief to many patients. In addition, stretching the shoes can be helpful. Patients should be specifically instructed to use a “ball-and-ring” shoe stretcher, a device that focally stretches just one portion of the shoe. As a last resort, surgical intervention may be necessary. The type of surgery indicated depends on the nature and degree of the underlying structural deformity. In some patients, extensive reconstruction may be required, and it is important to counsel these patients that they need more than a simple “shaving.”
Hallux Rigidus.
This condition is characterized by arthritis of the first MTP joint; it results in limited or total loss of dorsiflexion. Prominent dorsal osteophytes sometimes lead patients or providers to use the misnomer “dorsal bunion.” Patients with hallux rigidus often have pain with dorsiflexion of the toe (as they push off with the foot) and complain of “jamming.” If the dorsal osteophytes are large enough, finding comfortable shoes also becomes difficult.
Physical examination reveals limited mobility of the first MTP joint, especially on dorsiflexion (normal, 50 to 80 degrees). Crepitus and enlarged osteophytes may also be present. Radiographs reveal degenerative changes such as joint space narrowing, osteophytes, and sclerosis. Chronic gouty arthritis and other inflammatory arthropathies may resemble this condition, but radiographic changes are more destructive and lytic.
Initial treatment includes limiting joint stress and use of analgesics. An orthotic device with an extension under the great toe (Morton extension) and an extra-depth shoe should be prescribed. Limiting joint motion by stiffening the outer sole of the shoe (full-length steel shank) may also help. As with hallux valgus, using a ball-and-ring device to stretch the shoe over the prominent dorsal osteophytes may help.
Surgery involving either débridement of osteophytes (“cheilectomy”) or fusion is indicated if conservative treatment is unsuccessful. In general, less advanced disease can be treated with cheilectomy, whereas more advanced disease requires joint resection. Joint replacement for hallux rigidus is controversial and under investigation.
Sesamoid Disorders.
The first MTP joint contains two sesamoid bones (medial and lateral) that articulate with the plantar aspect of the metatarsal and help to serve as a fulcrum in normal joint mobility. Excessive or abnormal stress about this area can lead to pain and inflammation (sesamoiditis), cartilage injury (osteochondritis or osteonecrosis), or sesamoid fracture. Although a history of trauma may not be obvious, sesamoid injuries are not uncommon among runners, dancers, and other individuals who participate in high-impact activities.
On physical examination, swelling and tenderness is present on the plantar aspect of the first MTP joint; an inflamed bursa may also be appreciated in some instances. Foot radiographs should include a “sesamoid” view of the foot if a fracture is suspected. It is important to remember that bipartite (or multipartite) sesamoids are normal variants; a bone scan or magnetic resonance imaging may be needed when fracture is suspected and plain films are nondiagnostic.
Most sesamoid disorders respond to nonoperative measures, starting with rest and reduction of weight-bearing stresses. Acute fractures may require the use of a fracture boot or even a cast. Mild cases of sesamoiditis without fracture can be managed with a stiff-soled shoe and a soft insert/liner; custom orthotics providing relief under the sesamoids may also be helpful. In refractory cases, shaving or excision of the involved sesamoid may be necessary.
Disorders of the Lesser Metatarsophalangeal Joints
The second through fifth MTP joints (“lesser metatarsophalangeal joints”) are subject to a different set of stresses than those that affect the first MTP joint. The capsule that holds the lesser MTP joints together (the plantar plate) is thickened on its plantar aspect and is especially important for stability and can be affected by both acute and chronic injury.