Aortic Valve Sclerosis and Aortic Valve Stenosis
Kirsten Tolstrup
Carlos A. Roldan
The physical examination may not accurately differentiate between aortic valve sclerosis and stenosis, commonly underestimates or overestimates the severity of aortic stenosis, and cannot accurately assess the impact of aortic stenosis on the left ventricle (LV).
Definition
Aortic valve sclerosis: Thickened and hyperreflectant cusps without causing obstruction to LV outflow.
Aortic stenosis: Obstruction to LV outflow at the valvular (most common), subvalvular, or supravalvular levels. This chapter focuses on valvular aortic stenosis.
Common Etiologies and Prevalence
Aortic Valve Sclerosis
Aortic valve sclerosis is a degenerative, aging, and/or atherosclerotic process that occurs mainly in the elderly but can be seen as early as in the 4th to 5th decade of life.
Aortic Valve Stenosis
Valvular Aortic Stenosis
The most common forms of aortic valve stenosis are degenerative, congenital, and rheumatic.
In subjects >65 years old, degeneration associated with atherosclerosis of an inherently normal trileaflet valve is the most common etiology, with a prevalence of 2% to 4% (1,4).
In patients <60 years old, aortic stenosis is most commonly due to a congenital bicuspid valve with a prevalence of 1% to 2% of the general population (5,6). The condition is probably inherited with a prevalence among first-degree relatives reported to be 9% to 21% (7,8,9,10). Although mutations in NOTCH1 have been implicated in some cases, the genetics are still not well understood (11).
Rheumatic heart disease is more likely to be the cause if rheumatic mitral valve disease coexists. Rheumatic aortic valve stenosis is uncommon in the United States and typically only seen in immigrants.
Supravalvular Aortic Stenosis
Supravalvular aortic stenosis occurs as an isolated lesion or as part of the Williams syndrome (caused by mutation in the gene encoding elastin) (12). It accounts for <5% of LV outflow obstructions in children.
Subvalvular Aortic Stenosis
Subvalvular aortic stenosis often is associated with other congenital heart disease (25% to 60%), most commonly ventricular septal defects. It accounts for 10% to 20% of LV outflow obstructions in pediatric patients.
Echocardiography
Class I or Appropriate (Score 7–9) Indications for Echocardiography
There are no guidelines for echocardiography (echo) in subjects with aortic valve sclerosis. We suggest transthoracic echo (TTE) in asymptomatic middle-aged or older subjects with risk factors for atherosclerosis and a grade II to III/VI systolic ejection murmur at the
aortic area. Aortic valve sclerosis may indicate underlying atherosclerosis.
Table 9.1 Appropriate (Score 7–9) indications for echocardiography in patients with aortic stenosis
Diagnosis and assessment of the severity of aortic stenosis.
Assessment of left ventricular function, size, and/or hemodynamics.
Re-evaluation of patients with known aortic stenosis with changing symptoms or signs.
Assessment of changes in hemodynamic severity and ventricular function in those with known aortic stenosis in pregnancy.
Re-evaluation of asymptomatic patients with aortic stenosis (at least yearly if moderate or severe, and at least every 3 y if mild).
Evaluation of the ascending aorta in patients with bicuspid aortic valves (stenotic or non-stenotic) in whom associated aortic root disease (dilatation, aneurysm, or dissection) can occur.
(Adapted from Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/HFSA/HRS/ASNC/SCAI/SCCM/SCCT/SCMR 2011 Appropriate use criteria for echocardiography. J Am Coll Cardiol. 2011;57:1126–1166.)
Table 9.1 depicts the class I or appropriate indications for TTE in patients with aortic valve stenosis (13,14).
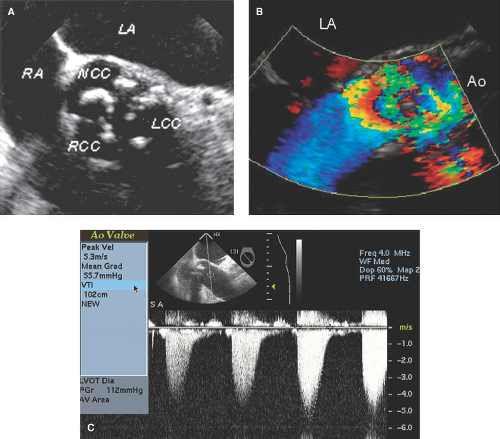
Transesophageal echocardiography (TEE) for planimetry of the valve to assess the severity of aortic stenosis and/or associated aortic root disease is uncommonly indicated when TTE is inconclusive or equivocal.
TEE is the test of choice for the diagnosis of supravalvular aortic stenosis and may also be indicated in bicuspid aortic valve stenosis for improved identification of the bicuspid nature as well as to identify any associated aortic aneurysm.
M-Mode, Two-dimensional, and Three-dimensional Echocardiography: Morphology of the Sclerotic and Stenotic Aortic Valve
Best Imaging Planes
TTE parasternal long- and short-axis and apical three- and five-chamber views.
TEE two-dimensional (2D) basal short-axis (usually 35 to 55 degrees) and long-axis (usually 120 to 140 degrees) views.
Real time three-dimensional (RT3D) TEE basal short axis views for online or offline reconstruction of the aortic root or LV outflow tract en-face views of the aortic valve.
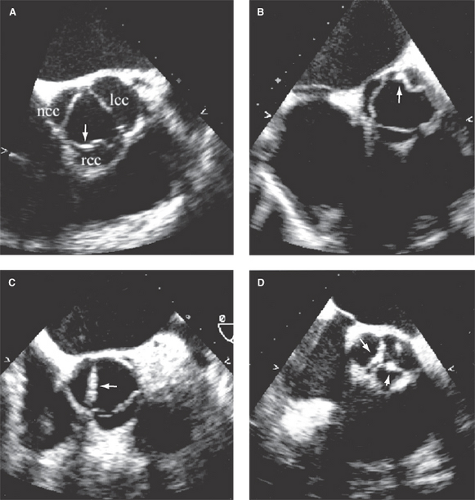
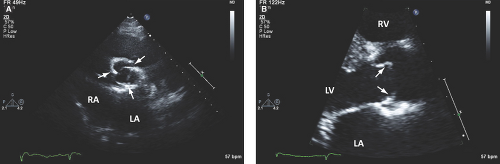
Real-time 3D TEE, although accurate in diagnosing and better characterizing the morphology of the sclerotic and stenotic aortic valve, may not add clinically significant information over 2D images (Fig. 9.1).
Key Diagnostic Features
Degenerative Aortic Valve Disease
Aortic Valve Sclerosis
In aortic valve sclerosis, one or more cusps are hyperreflectant and thickened (>2 mm). Mobility is usually normal, but it can be mild or moderately decreased. Valve sclerosis can be diffuse, localized, nodular, or mixed; it can affect all areas of the cusps, but it most frequently affects the margins and basal portions (Fig. 9.1).
Cusp separation ≥1 cm by M-mode indicates valve sclerosis or noncritical stenosis.
Aortic Valve Stenosis
In aortic valve stenosis, the cusps are hyperreflectant, thickened, calcified, and nonmobile with a decrease in orifice area. The fibrosis, nodular deposits, and calcification are more severe at the base of the cusps, extend to the cusp margins and commissural regions, and then progress to the free edge (Fig. 9.2A). The base of the leaflets may become fixed and immobile. Commissural fusion rarely occurs.
Aortic annulus and root sclerosis and calcification are common.
Congenital Bicuspid Aortic Valve Disease
A bicuspid valve demonstrates two cusps usually of unequal size and a single linear commissure (Fig. 9.3A). Frequently, a raphe makes the bicuspid valve appear tricuspid-like, but two cusps become apparent in systole. Calcifications can be seen along the commissure and more commonly in the raphe.
The long-axis views show the eccentric closure of the bicuspid valve (Fig. 9.3B).
An early sign of bicuspid valve stenosis is systolic doming of the cusps, which means that the edges of the leaflets are curved toward the center of the aorta (Fig. 9.3B). This finding suggests pliable cusps with restricted mobility of the tips relative to the body of the cusps. Domed but thickened and sclerotic cusps suggest aortic stenosis.
In late stages, it is difficult to separate a bicuspid from a trileaflet degenerative valve. TEE may be helpful in such cases.
Aortic root dilatation out of proportion to the degree of stenosis is common due to associated cystic medial necrosis (Fig. 9.4A,B and Fig. 8.3).
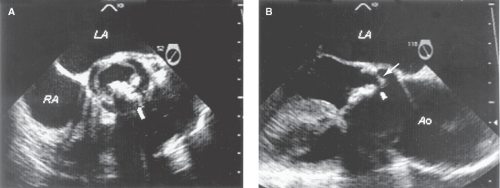
Rheumatic Aortic Valve Disease
The hallmark of rheumatic aortic valve disease is commissural fusion, thickening of the tip portions, and retraction of the cusps with focal thickening of the edges. Often, all commissures are affected. Retraction of leaflets with associated aortic regurgitation is common (Fig. 9.5A,B).
Secondary calcification is common, and, at the extreme, it is difficult to discern between chronic, healed rheumatic stenosis and the degenerative form. Associated mitral stenosis helps in diagnosing rheu-matic disease.
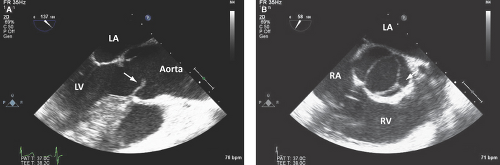
Supravalvular Aortic Stenosis
Three types of supravalvular aortic stenosis exist. The most common is a discrete fibrous membrane near the sinotubular junction in a normal-sized aorta (Fig. 9.6A); other types include fibromuscular thickening above the coronary sinuses causing an hourglass-shaped narrowing and diffuse hypoplasia of the ascending aorta.
Supravalvular diffuse or discrete narrowing is associated with dilated coronary ostia and aortic valve cusp thickening and sclerosis.
Subvalvular Aortic Stenosis
The most common type of subvalvular aortic stenosis is a fibrous membrane located just below the aortic valve extending from the anterior septum to the
anterior mitral leaflet; it appears on echo as a discrete linear structure in the left ventricular outflow tract (LVOT) from the TTE parasternal or apical long-axis view (the ultrasound beam is perpendicular to the membrane) (Fig. 9.7A).
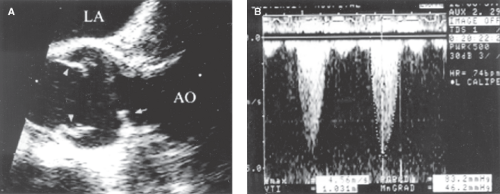
Figure 9.6: Supravalvular aortic stenosis. A.Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree