Anesthesia for Trauma and Burns
Cindy Kim
Rebecca Kalman
I. INITIAL EVALUATION OF THE TRAUMA PATIENT
Rapid assessment of injuries and institution of resuscitative measures are particularly important in trauma patients. Life-threatening injuries should be identified immediately based on Airway, Breathing, Circulation, Disability/neurologic function, and Environmental priorities with treatment measures initiated simultaneously. Assume that all patients have a cervical spine injury, a full stomach, and hypovolemia until proven otherwise.
A. Airway
1. Airway assessment should include inspection for foreign bodies, facial and laryngeal fractures (palpable fracture and subcutaneous emphysema), and expanding cervical hematomas. Dyspnea, hemoptysis, dysphonia, stridor, and air leaking through the neck wound may also be signs of airway injury. Remove all secretions, blood, vomitus, and any existing foreign bodies (e.g., dentures or teeth).
2. Minimize movement of the cervical spine during airway manipulation. If immobilizing devices must be removed temporarily, an assistant should keep the head in a neutral position with manual in-line immobilization.
3. Establish a definitive airway if there is any doubt about the patient’s ability to maintain airway integrity. With blunt or penetrating injuries to the neck, endotracheal intubation may worsen a laryngeal or bronchial injury. Functional suction equipment should always be immediately available to prevent aspiration if the trauma patient with a full stomach vomits.
a. The awake patient. Depending on the patient’s injuries, the ability to cooperate, and cardiopulmonary stability, several options are available. Choice of technique for securing the airway should be individualized based on operator preference and patient circumstances since there are few data to support one approach over another.
1. Intubations after a rapid sequence induction is our most common approach to the airway. Video laryngoscopy may be helpful in patients with suspected cervical spine injury.
2. Awake nasal or orotracheal intubation with the use of a laryngoscope or fiberoptic bronchoscope is an alternative.
3. Blind nasal intubation may be performed on the spontaneously breathing patient.
4. Awake cricothyroidotomy or tracheostomy may be necessary for patients with severe facial trauma that might be contraindications to other methods of intubation.
b. The combative patient. A rapid sequence orotracheal intubation is often the most expedient approach provided there are no problems precluding neuromuscular blockade. Hypoxemia must always be excluded in an agitated patient.
c. The unconscious patient. Orotracheal intubation is usually the safest and most expeditious approach.
d. If the patient arrives with an esophageal obturator airway or esophageal gastric tube airway, perform endotracheal intubation before removing these devices because vomiting frequently occurs with their removal.
4. The intubated patient. Verify the position of an endotracheal tube by auscultating for breath sounds bilaterally and by detecting end-tidal CO2. Secure the endotracheal tube, and ensure adequate ventilation and oxygenation.
B. Breathing. Adequate function of the lungs, diaphragm, and chest wall should be evaluated rapidly. Supplemental oxygen should be provided to all trauma patients, either by mask or by endotracheal tube.
1. Assess the chest wall excursion, and auscultate the lungs to ensure adequate gas exchange. Visual inspection and palpation may rapidly detect injuries such as a pneumothorax.
2. Tension pneumothorax, massive hemothorax, and pulmonary contusion are three common conditions that may acutely impair ventilation and should always be identified. Positive-pressure ventilation may worsen a tension pneumothorax (and cardiac tamponade) and can rapidly lead to cardiovascular collapse.
3. The trauma patient’s breathing and gas exchange should be reevaluated after intubation or initiation of positive-pressure ventilation and periodically after the initial assessment.
C. Circulation
1. In the severely injured trauma patient, rapid initiation of resuscitation measures is important to prevent and control hypothermia, acidosis, and coagulopathy.
2. Hemodynamics is initially assessed by palpating pulses and measuring the blood pressure.
3. Intravenous (IV) access. Check IV lines already in place to ensure proper function. At least two large (preferably 14 gauge) catheters should be placed. These lines should be placed above the level of the diaphragm in patients with injuries of the abdomen (where there is a potential for major venous disruption). IV access below the level of the diaphragm is helpful when obstruction or disruption of the superior vena cava, innominate, or subclavian vein is suspected.
4. Peripheral venous cannulation failure. In this event, percutaneous subclavian or femoral vein cannulation should be carried out. Although the internal and external jugular veins remain options, access to these structures is frequently hindered by immobilization of the head and neck for a suspected cervical spine injury. If these approaches prove unsuccessful, surgical cutdowns can be performed. The saphenous vein at the ankle and the antecubital venous system are acceptable options. Intraosseous access to the vasculature is also an option for personnel trained in this technique.
5. Volume resuscitation should be individualized. The concept of “damage control” emphasizes multiple approaches to control and prevent tissue hypoperfusion, acidosis, coagulopathy, and hypothermia.
a. Damage control resuscitation (DCR) refers to the strategy of limiting crystalloid use, early resuscitation with packed red blood cells and clotting factors, and maintenance of a systolic blood pressure around 85 to 90 mm Hg. The disadvantages to crystalloid infusion include dilution of coagulation factors, hemodilution, and clot disruption. Early administration of blood and clotting factors serves to treat trauma-induced coagulopathy that can occur early after injury. In a patient in whom hemorrhage has not been definitely controlled, elevation in blood pressure and cardiac output can cause dislodgement of a clot and further bleeding. Hypotensive resuscitation should not be used in certain subsets of patients such as patients with head trauma.
b. Type-specific non-cross-matched blood or type O-negative blood may be given before cross-matched blood becomes available. Fresh frozen plasma and platelets should be ordered early if a patient
requires ongoing blood transfusion. The ratio of fresh frozen plasma and platelets to packed red blood cells should be closely monitored with hemoglobin levels, prothrombin times, and platelet counts. Even the administration of components in a 1:1 ratio is inferior to the administration of fresh whole blood when clotting activity and platelet counts are compared, but whole blood resuscitation is not an option in most clinical settings except the battlefield. Aggressive resuscitation with blood products can lead to hypothermia, hyperkalemia, and hypocalcemia. Empiric treatment is often indicated as the laboratory results may lag behind the clinical scenario when massive fluid resuscitation is undertaken.
requires ongoing blood transfusion. The ratio of fresh frozen plasma and platelets to packed red blood cells should be closely monitored with hemoglobin levels, prothrombin times, and platelet counts. Even the administration of components in a 1:1 ratio is inferior to the administration of fresh whole blood when clotting activity and platelet counts are compared, but whole blood resuscitation is not an option in most clinical settings except the battlefield. Aggressive resuscitation with blood products can lead to hypothermia, hyperkalemia, and hypocalcemia. Empiric treatment is often indicated as the laboratory results may lag behind the clinical scenario when massive fluid resuscitation is undertaken.
c. Severely injured trauma patients do not tolerate prolonged surgical procedures. Damage control surgery refers to the concept of employing initial short surgical procedures immediately after injury with the goals of controlling hemorrhage and preventing contamination through temporary measures. Patients then undergo definitive corrective surgery at a later date after they have been stabilized.
6. Vasopressor infusions should not substitute for adequate volume replacement during initial resuscitation. Vasopressors may be necessary as a temporizing measure if perfusion pressure is clearly inadequate during ongoing volume resuscitation.
7. Antifibrinolytics, such as tranexamic and ε-aminocaproic acid can reduce mortality in bleeding trauma patient when started as soon as possible within 3 hours of injury. The safety of antifibrinolytics after 3 hours or in certain patient subsets such as isolated traumatic brain injury has yet to fully elucidated and may be associated with increased adverse events.
D. Disability/Neurologic Evaluation. A brief neurologic examination yields useful information in assessing cerebral perfusion or oxygenation and can provide a simple and quick means of predicting a patient’s outcome.
1. The level of consciousness can be described by the AVPU method (A = alert, V = responds to verbal stimuli, P = responds only to painful stimuli, and U = unresponsive to all stimuli). A more detailed and quantitative assessment of neurologic function is with the Glasgow coma score (GCS; Table 34.1) that is the sum of the best eye opening, verbal, and motor responses.
2. An altered level of consciousness dictates immediate reevaluation of the patient’s oxygenation and circulation, even though it can be of central nervous system origin (trauma or intoxication).
3. Neurologic deterioration can rapidly occur in trauma patients and necessitates frequent neurologic reevaluation.
E. Environmental Control. Trauma patients are often hypothermic upon arrival at the hospital and require aggressive efforts to maintain body heat. Hypothermia can exacerbate coagulopathy.
1. External warming devices should be applied, IV fluids warmed before infusion, and a warm environment maintained.
2. If there is any suspicion of exposure to chemical agents, decontamination of the victim must be carried out before entrance to the hospital. This terminates exposure, protects the health care provider, and allows the hospital to function effectively.
F. Diagnostic Studies
1. Laboratory studies include blood type and cross-match, complete blood count, platelet count, prothrombin time, activated partial thromboplastin time, electrolytes, glucose, blood urea nitrogen, creatinine, urinalysis, and, if indicated, toxicologic screening.
TABLE 34.1 Glasgow Coma Score | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
2. Radiographic studies should include a lateral cervical spine film, a chest radiograph (CXR), and an anteroposterior view of the pelvis on all patients with blunt trauma. At a minimum, a CXR is obtained in all patients with penetrating injuries of the trunk. Additional studies include thoracic, lumbar, and sacral spine films and chest and abdominal computed tomography (CT) studies.
a. Lateral radiographs of the cervical spine must include the C7-T1 interface and must be of sufficient quality to delineate the structures of interest (i.e., soft tissues and bones).
b. If the patient’s clinical condition allows time for additional studies, open-mouth odontoid and anteroposterior views of the neck (standard trauma cervical spine series) may be obtained.
c. If the clinical evaluation demonstrates a patient with significant neck pain and tenderness but no evidence of fracture or dislocation on the plain radiographs, CT and magnetic resonance imaging may help delineate an occult injury.
3. A 12-lead electrocardiogram (ECG) should be performed on all major trauma patients to help evaluate the presence of myocardial injury (e.g., contusion, tamponade, ischemia, and arrhythmia).
4. Ultrasonic examination of the abdomen (called FAST for Focused Abdominal Sonography in Trauma) specifically focusing on free fluid within the perihepatic, perisplenic, perivesical, and pericardium is very helpful to exclude significant intraperitoneal bleeding in patients with blunt abdominal trauma.
G. Monitoring is dictated by the severity of the patient’s injuries and preexisting medical problems.
1. An arterial line is useful in patients with hemodynamic instability or respiratory failure.
2. A central venous pressure line may be required to assess volume status and administer vasoactive drugs.
3. A pulmonary artery catheter may be helpful in patients with ventricular dysfunction, severe coronary artery disease, valvular heart disease, multiple organ system involvement, or hemodynamics that seem disproportionate to their trauma burden. Placement is planned according to the time available and the clinical status of the patient.
II. SPECIFIC INJURIES
A. Intracranial and Spinal Cord Trauma (see Chapter 25)
B. Facial Trauma. Considerable force is required to produce facial fractures. Accordingly, these injuries often are associated with other injuries such as intracranial and spinal cord trauma, thoracic injury, myocardial contusion, and intra-abdominal bleeding. Brisk oral or nasal bleeding, broken teeth, vomitus, or tongue or pharyngeal injury may occlude the airway and complicate airway management. Trismus may be associated with these injuries and should be assessed before the induction of anesthesia. Emergency cricothyroidotomy or tracheostomy done under local anesthesia may be lifesaving.
a. Type I (transverse or horizontal). The body of the maxilla is separated from the base of the skull above the level of the palate and below the level of the zygomatic process.
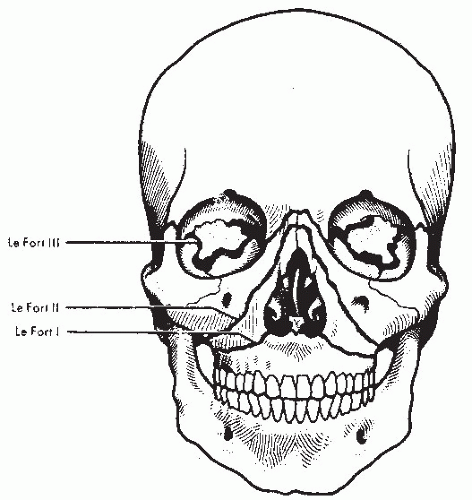 FIGURE 34.1 The LeFort classification. (From Rosen P, Baker FJ, Barkin RM, et al., eds. Emergency Medicine: Concepts and Clinical Practice. 2nd ed. St. Louis: Mosby; 1988.) |
b. Type II (pyramidal). Vertical fractures through the facial aspects of the maxilla extend upward through the nasal and ethmoid bones.
c. Type III (craniofacial dysjunction). Fractures extend through the frontozygomatic suture lines bilaterally, across the orbits, and through the base of the nose and the ethmoid region.
d. Le Fort and related fractures are frequently associated with skull fractures and cerebrospinal fluid rhinorrhea. Nasotracheal intubation and placement of nasogastric tubes are relatively contraindicated under these circumstances. Elective nasal intubation (or tracheostomy) may be necessary, however, before operative repair. A fiberoptic bronchoscope may be used in these cases to guide endotracheal tube into the trachea.
e. In the presence of rhinorrhea, positive-pressure mask ventilation can potentially cause pneumocephalus.
2. Mandibular fractures
a. Malocclusion, limitation of mandibular movement, loose or missing teeth, sublingual hematoma, and swelling at the fracture site complicate airway management.
b. Posterior displacement of the tongue producing airway obstruction is associated with bilateral condylar or parasymphyseal fractures of the mandible. Simple forward traction on the tongue often provides relief.
c. Reestablishment of normal occlusion may necessitate intermaxillary fixation, which can also be combined with rigid fixation. Awake nasotracheal intubation is recommended if the nose has not been severely traumatized.
3. Ocular trauma usually requires general anesthesia for repair. Special considerations for open-eye injuries are discussed in Chapter 26, section I.C.1.
4. Anesthetic management. Most displaced facial fractures require general anesthesia for repair. Although children usually require general anesthesia, many soft tissue injuries can be treated with local anesthesia. Maintenance of a patent airway is the principal concern, and induction may require awake nasotracheal intubation, fiberoptic laryngoscopy, or tracheostomy under local anesthesia.
C. Neck trauma may cause cervical spine injury, esophageal tears, major vascular injuries, and airway injuries. Airway injuries may present with obstruction, subcutaneous emphysema, hemoptysis, dysphonia, or hypoxemia.
1. “Clothesline” injuries occur from direct trauma to the upper airway and can result in separation of the larynx from the trachea or separation between the cricoid cartilage and the first tracheal ring. These injuries do not always present with an open neck wound. Additional injuries include laryngotracheal transection, laryngeal fractures, and vascular injury.
2. Blunt injury over the carotid arteries may result in intimal disruption and dissection, even in the absence of initial symptoms. Angiography or ultrasonography may be required to exclude these injuries.
3. Initial management of penetrating trauma includes direct compression of involved vessels to control hemorrhage and prevent air embolism.
4. Associated thoracic injuries, such as pneumothorax and hemorrhage from injury to the great vessels, may occur with lower neck injuries.
5. Anesthetic management
a. Securing the airway is the central issue in these patients. A coordinated approach among members of the trauma team is necessary. A surgical airway or direct intubation of an open airway defect can be lifesaving. Anesthesia induction via spontaneous ventilation of a potent inhalational agent can be useful in the presence of airway disruption with the caveat that the patient likely has a full stomach and is a high risk for aspiration. Preparations should be made for fiberoptic intubation, rigid bronchoscopy, and a surgical airway.
b. Great vessel injuries in the neck may necessitate lower extremity IV access.
D. Chest trauma can involve injuries to the trachea or larynx, heart, great vessels, thoracic duct, esophagus, lung, or diaphragm.
1. Rib fractures are a common feature of major thoracic trauma and mandate assessment for pneumothorax by CXR. First-rib fractures should alert the clinician to the potential for associated internal injuries due to severe forces needed to fracture the first rib. Multiple rib fractures most commonly involve ribs 7 to 10 and often accompany lacerations of the spleen or liver.
2. The hypoxemia and respiratory failure that accompany flail chest and other major chest injuries are indicative of underlying pulmonary contusion. IV fluids should be administered judiciously because the injured lung is sensitive to fluid overload.
3. The presence of subcutaneous emphysema may indicate the presence of a pneumothorax or laryngeal, tracheobronchial, or esophageal trauma. Pneumothorax and hemothorax may lead to respiratory and cardiovascular collapse. If these conditions are present or highly suspected, chest tubes should be placed before the induction of general anesthesia. Avoid central line insertion (particularly by the subclavian route) on the side opposite an injury because of the potential consequence of bilateral pneumothorax. Avoid the ipsilateral side if a concomitant major venous injury is suspected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






