Anatomical Anomalies in Ultrasound Simulation
Jeremy Kaplowitz
Paul E. Bigeleisen
Ultrasound-guided regional anesthesia has provided the regional anesthesiologist with the ability to visualize pertinent nerves and local anesthetic spread. One consequence of this newfound “vision” in regional anesthesia is the ability to visualize anatomic variations and sonopathology. These findings may impact the performance of your regional anesthetic and may lead to an altered anesthetic technique.
Currently, there is some debate about the role of regional anesthesiologists in diagnosing pathologic abnormalities while performing ultrasound-guided nerve blocks. Although this question has imporTant medicolegal and clinical implications, it is beyond the scope of this chapter to delve into this issue. Nonetheless, practitioners agree that knowledge of the common anatomical variations is essential in allowing the practitioners to perform effective and safe regional anesthesia.
In order to appreciate the anatomic variants, we first discuss some of the common anatomic artifacts that frequently confuse novices. Then we discuss some of the common anatomic variants. Last, we highlight some of the more common sonopathologic findings that you may encounter while performing ultrasound-guided regional anesthesia.
Anatomic artifacts
There are various anatomic artifacts that one may encounter while performing a regional anesthetic block. Anatomic artifacts occur when tissue structures are confused with each other. These are usually structures that may appear similar to nerves. Some common examples include tendons, muscles, lymph nodes, and blood vessels.
Tendons
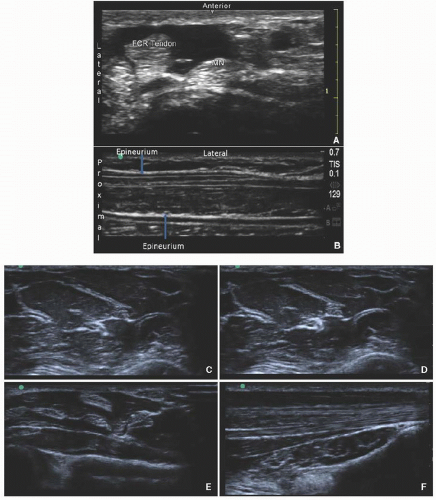
Tendons may be confused with nerves that have a hyperechoic appearance. This artifact confusion most commonly occurs while performing sciatic nerve blocks at the popliteal fossa or during selective nerve blocks in the arm and forearm. The normal sonographic image of a tendon is groups of hyperechoic dots mixed in among a hypoechoic background. Nerves often have fascicles with a hypoechoic center (Fig 8.1A), which may also be apparent in a long-axis view (Fig 8.1B). In Figure 8.1B, notice the epineurium of the nerve and the hypoechoic fascicles within the nerve. The primary distinction is that tendons have hyperechoic continuous fibrils, whereas nerves have fascicles. These fascicles have a hyperechoic border caused by the perineurium and hypoechoic center caused by the axons. Tendons may also show greater anisotropy than nerves, showing a greater change in echogenicity when toggling the probe. Moreover, a tendon should be seen taking origin from a muscle or inserting on a bone. This can be seen by scanning along the length of the structure in question. Finally, a tendon should move in the image when the appropriate muscle/joint is contracted (Fig. 8.1C-E).
Vasculature
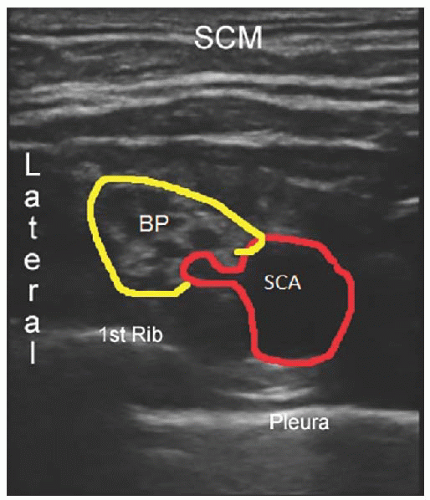
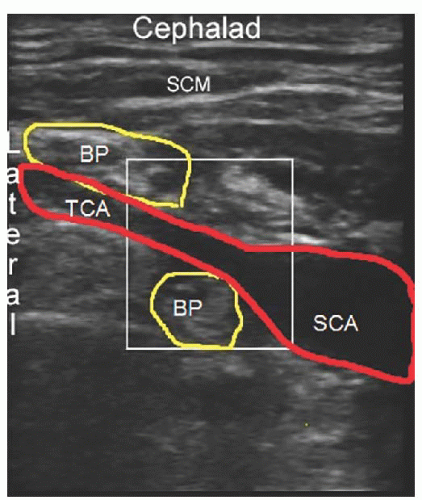
Larger blood vessels are not usually mistaken for nerves. In fact, most regional anesthesiologists use vascular landmarks to help identify many nerves. Smaller blood vessels are easier to confuse with nerves, especially in the short-axis view. Color-flow Doppler is invaluable in helping to distinguish small blood vessels from nerves. This problem is frequently encountered while performing brachial plexus nerve blocks (Figs. 8.2 and 8.3). If in doubt, use Doppler to ensure that the nerve in question is truly a nerve.
Lymph Nodes
Lymph nodes may be flat or oval and either hypoechoic or hyperechoic. Lymph nodes can be differentiated from nerves by their lack of fascicles. They are most commonly seen in axillary, femoral, sciatic, and interscalene blocks (Fig. 8.4).
Muscle
Muscles have either fusiform or pennant structures. Fusiform muscles have fascicles with a parallel orientation that converge toward the tendon at the end of the muscle. Pennate muscles have fascicles that appear more featherlike in relation to their aponeurosis or tendon. Muscles have a relatively hypoechoic appearance with some hyperechoic structures (connective tissue or fat) embedded in the muscle. Some practitioners liken this appearance to a “starry night.” The ratio of hypoechoic to hyperechoic muscle is based on the ratio of connective tissue to fascicle within each muscle. In the long axis, muscle may have a featherlike appearance (pennate muscle), and it is usually well organized. Intramuscular tendons and aponueroses are best imaged in the short axis. It may be difficult to distinguish muscle from nerve when performing gluteal or popliteal sciatic nerve blockade (Fig 8.5). Small muscles may have the appearance of a small vessel or nerve. Use of nerve stimulator can usually allow the practitioner to differentiate nerves from muscles.
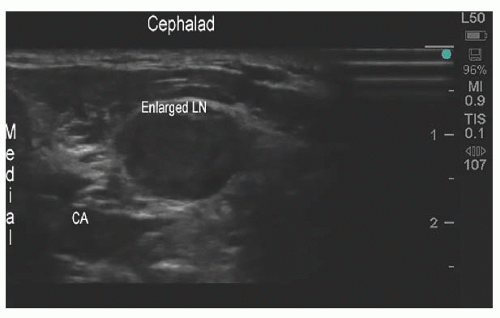 Figure 8.4. After probe repositioning, the structure is clearly the transverse cervical artery (CA) which divides the brachial plexus in two. LN, lymph node. |
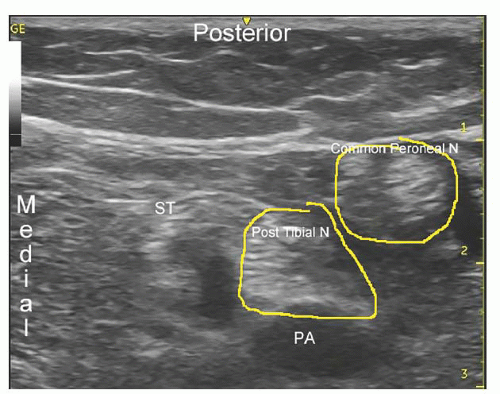 Figure 8.5. While performing sciatic blocks, it may be difficult to distinguish between the nerve and the surrounding muscle. Placement of local anesthetic may enable you to distinguish between the two. N, nerve; PA
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|