Sepsis & Systemic Inflammatory Response (SIRS):
Links: Definitions | MSOF / MODS | Risks & S/s | Labs | Tx of Septic Shock | Empiric Abx | Shock | Catheter Infection | See ALI / ARDS |
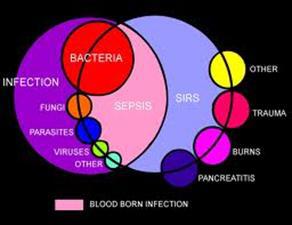
Sepsis is an infectious inflammatory syndrome with clinical evidence of infection that may include focal infections and meningitis. Multiorgan failure and death may rapidly develop.
• Sepsis represents 2% to 3% of all hospital admissions; 59% of pt’s require ICU admission, accounting for 10% of all ICU admissions (South Med J. 2007;100:594-600)…. Pneumonia is the most common trigger, followed by peritonitis and urinary tract infection with or without pyelonephritis.
• Postmortem studies of patients who died of sepsis show evidence of profound immunosuppression (JAMA 2011;306:2594).
 Infection: a pathological process caused by the invasion of normally sterile tissue or fluid or body cavity by pathogenic or potentially pathogenic micro-organisms. Signs and symptoms of infection requires any two of following signs and symptoms both present and new to the patient:
Infection: a pathological process caused by the invasion of normally sterile tissue or fluid or body cavity by pathogenic or potentially pathogenic micro-organisms. Signs and symptoms of infection requires any two of following signs and symptoms both present and new to the patient:
• temperature >38.3° C or <36.0° C.
• heart rate >90 beats per min (bpm).
• respiratory rate >20 breaths per min.
• acutely altered mental status.
• leucocytosis – WBC >12 000/¼l.
• leukopenia – WBC <4000/¼l.
• hyperglycaemia (plasma glucose >7.7 mmol/l) in absence of diabetes.
• plasma C-reactive protein >2 SD above the normal value.
Systemic Inflammatory Response (SIRS): 2 or more of the following: Temp >38C (100.4F) or <36C (96.8F). HR >90, RR >20 (or CO2 <32 mmHg). WBC >12K (or <4K or >10% bands). Can be due to infection, pancreatitis, burns or post-op condition.
Bacteremia: Presence of viable bacteria in the blood.
Sepsis: SIRS + documented infection. Fever is the most common sign. G+ organisms are more common than G- as a cause. 30% mortality. Sepsis is the most frequent cause of ARDS. Sepsis is the leading cause of death in critically ill pt’s, the exact cause of death remains elusive (probably a combo of shock, renal failure, infection and immune dysregulation). Sepsis is a clinical dx. Sepsis is the combination of suspected or proven infection and the presence of at least 2 signs of systemic inflammatory response syndrome.
PP: macrophage activation, proinflammatory cytokines (TNF, IL1,6) activate PMN’s. Microcirculation is altered due to vasoconstriction, endothelial damage from cellular adhesion in capillaries and micro thrombosis.
Severe Sepsis: sepsis (SIRS) + acute end organ dysfunction (MS change, hypoxemia, incr lactate, oliguria). Severe sepsis is defined as acute organ system dysfunction associated with infection. The most common presenting symptom of severe sepsis is respiratory system dysfunction, followed by shock and renal system dysfunction. Severe sepsis accounts for more than 215,000 deaths per year in the U.S. Severe sepsis refers to sepsis complicated by one organ dysfunction that can be defined by the Sequential Organ Failure Assessment (SOFA) score.
Multi-organ failure: two or more organ dysfunction.
PaO2/FiO2 d26.7 kPa.
Noradrenaline/adrenaline e0.1 ¼g/kg per min.
Creatinine e330 ¼mol/l.
Platelets d50 × 103/l.
Bilirubin e102 ¼mol/l.
Glasgow Coma Score <9.
Septic shock: sepsis + hypotension despite adequate fluids + hypoperfusion abnormalities. –> decr systemic vascular resistance. Septic shock can induce severe microcirculatory alterations that manifest as reduced end-organ perfusion, reduced oxygen delivery, and increased accumulation of oxygen debt. 40% mortality. In early septic shock, the cardiovascular system responds with resting tachycardia, warm distal extremities, and brisk capillary refill. In later stages of septic shock, circulatory collapse ensues with weak distal pulses, delayed capillary refill, and cool extremities. Hypotension is a very late, very ominous sign. Septic shock is a subgroup of severe sepsis and is defined as sepsis-induced hypotension with systolic blood pressure of 90 mm Hg or less or a reduction of 40 mm Hg or more from baseline despite adequate fluid resuscitation, along with other perfusion abnormalities such as oliguria or lactic acidosis. Septic shock in adults applies to a state of acute circulatory failure unexplained by other causes, defined as persistent arterial hypotension (a systolic blood pressure (SBP) <90, MAP <60, or a reduction in SBP 40 mmHg from baseline despite adequate volume resuscitation).
ICD-9:
995.91 Sepsis
995.92 Severe sepsis
995.93 Systemic inflammatory response syndrome due to noninfectious process without acute organ dysfunction
995.94 Systemic inflammatory response syndrome due to noninfectious process with acute organ dysfunction
Pearls: In 22% to 33% of suspected sepsis cases, culture results are not positive for pathogens. Of all positive culture results, gram-positive bacteria are identified in 25% to 50% of cases and gram-negative bacteria in 22% to 37% of cases. The 2-year survival rate was only 45% in sepsis survivors and quality of life was decreased, but expenses per QALY were low according to 17 month f/u on 470 adults (Crit Care Med 2009;37:1268)…..The mean total cost for a surviving patient with severe sepsis was 32,563: 22,915 (70.4% of the total) for intensive care and 9648 for treatment in ordinary wards…..The mean cost per QALY increased with age.
Multiple Organ Dysfunction Syndrome (MODS): = Multi-organ system failure (MSOF).
Failure of >2 organs with systemic inflammation. Altered organ function in an acutely ill person such that homeostasis can’t be maintained w/o interventions. The most common cause of death in the ICU. Often due to trauma, burns, pancreatitis, aspiration, or massive blood transfusions (>20 units). If 2 organs fail have a 50% mortality, 80% if 3 organs. See ARDS in pulmonary chapter.
Pressure Ulcer related Sepsis: has 50% in-hospital mortality rate. Usually polymicrobial (G+, G-, anaerobes). Swab of ulcer not helpful. Treat with broad spectrum Abx such as Imipenem.
Risk Factors for Sepsis: Extremes of age, DM, AIDS, hepatic/ renal failure, indwelling catheter, recent operation.
Predictors of bacteremia: (2004;38:357-62) age >30 yo; HR >90; temp >37.8°C (100°F); WBC >12,000 cells/ mL (12 3 106 per L); presence of a central venous catheter; and length of hospital stay >10 days. H/o trauma or surgery, chronic renal failure, diabetes or HIV. Each of these predictors ~ doubled the risk of a positive blood Cx.
• Severe sepsis occurs more often (9.4 vs. 5.6 per 1000 population) — and is more deadly — in blacks than in whites (2.6 vs. 1.7 per 1000 population for deaths caused by infections, and 1.8 vs. 1.0 per 1000 population for deaths caused by severe sepsis)(JAMA 2010;303:2495).
S/s: dyspnea, malaise, altered MS, F/C, N/v, tachy, hypotension, oliguria/ anuria. S/s similar to hypovolaemic shock except in the first stages: Pyrexia (fever), due to increased level of cytokines. Systemic vasodilation resulting in hypotension (low blood pressure). Systemic leukocyte adhesion to endothelial tissue. Reduced contractility of the heart. Diffuse capillary damage in the lung. Activation of the coagulation pathways, resulting in disseminated intravascular coagulation. Increased levels of neutrophils.
1. Fever: the usual presentation. The higher the fever, the more likely the patient is to be bacteremic. Hypothermia or normal temperature in association with bacteremia is a bad prognostic sign.
2. Hemodynamic changes: Tachycardia in association with fever is the rule; pulse is slower in typhoid fever and brucellosis. Hypotension is the most important determinant of outcome. Failure to reverse early warm pre-shock leads to irreversible organ damage and death.
3. Acid–base changes: Initially, respiratory alkalosis develops in response to anaerobic metabolism and lactic acid build-up. Recognizing this pre-shock syndrome is critical. Failure to treat leads to metabolic acidosis and an increased likelihood of death.
4. Respiratory changes: Hyperventilation occurs early. Hypoxia and ARDS are common. CXR reveals pulmonary edema.
Heme –> incr/decr WBC, incr bands/ PTT/ fibrin split products (FSP)/ D-dimer. Decr platelets. Eosinopenia, considered by some a forgotten marker of acute infection, is a useful diagnostic marker for sepsis in newly admitted patients to the intensive care unit (Crit Care. 2008;12:R59)…better than C-reactive protein…..With a cutoff value of < 50 cells/microliter, eosinopenia was 80% sensitive and 91% specific in making this distinction, with positive and negative likelihood ratios of 9.12 and 0.21, respectively…..Eosinopenia was not as reliable in distinguishing SIRS from infection.
• A normal WBC count does not rule out bacteremia according to data on 3563 adults who had blood cultures at a single emergency department…of which 289 had bacteremia, 52% had normal WBC count and 17% had neither WBC elevation nor fever (J Emerg Med 2012;42:254)……The fact that leukocytosis is associated with infection does not mean that the white blood cell count is a good test for infection, because many patients with infection have no leukocytosis, and many patients with leukocytosis have no infection…….The WBC count is the right test for neutropenia and malignancies of the white blood cell, but it is not a discriminatory test for infection……When evaluating a patient for possible infection, WBC counts should be used only as part of validated multivariable decision rules that have adequate predictive value for medical decision making, such as the Bacterial Meningitis Score.
Metabolic –> incr lactate, glucose, decr pH. Some suggest 4- to 6-hourly serum lactate measurements. Low (<70 mg/dL) blood glucose levels indicate a poor prognosis (risk of death 4.7-fold) in pt’s with E coli bacteremia (Am J Med 2006;119:952-957)…. E. coli is the most common isolate among all blood infections.
Pulmonary –> decr PaCo2, decr PaO2.
GI –> incr bili, AST, ALT.
Renal –> incr BUN/ Cr. Acute renal failure is seen in 23% with severe sepsis and 51% with septic shock (NEMJ 2004;351:159-69).
Biomarkers in Sepsis: interleukin (IL)-1 receptor antagonist, IL-8, intercellular adhesion molecule-1, tumor necrosis factor, and caspase-3. Pt’s who died had higher mean biomarker levels than those who survived (Crit Care Med 2007;35:2016). Evidence of increased tissue hypoxia (lactate 4 mmol/L and central venous oxygen saturation <70%) seems to be bimodal with respect to time, reflecting the different clinical presentations seen in early and late septic shock.
• BNP appears to be a useful biomarker for diagnosis and risk stratification of patients with septic shock in the absence of CHF (Arch Surg 2008;143:242-246)…..sepsis leads to damage of cardiomyocytes and cardiac contractile dysfunction……a drop in BNP levels during follow-up was predictive of survival, whereas continuation of high levels correlated with death.
• In patients with sepsis, use of an algorithm based on plasma procalcitonin levels allowed substantial reductions in antibiotic-therapy duration without deleterious effects on outcome (Am J Respir Crit Care Med 2008;177:498)….a recommendation was given to continue or stop antibiotic therapy based on PCT level after 3 days (for patients with baseline PCT levels <1 µg/L) or 5 days (for those with baseline levels 1 µg/L) of antibiotic therapy.
• A study on 971 patients with SIRS at 10 academic emergency departments found the combination of the following three biomarkers was most strongly associated with development of severe sepsis within 72 hours: neutrophil gelatinase-associated lipocalin, interleukin-1–receptor antagonist, and protein C (Crit Care Med 2009;37:96).
Hemodynamic Findings in Sepsis:
Heart rate: >100 beats/min. Major compensatory mechanism for low systemic vascular resistance
Mean arterial blood pressure: <65 mm Hg. Hallmark of septic shock.
Cardiac index (cardiac output/m2 [surface area]): >4 L/min/m2. Elevated in early septic shock; may be depressed in late septic shock.
Pulmonary arterial wedge pressure: 4-10 mm Hg. Must be sure that hypovolemia is not the cause of hypotension; perform fluid resuscitation until pulmonary arterial wedge pressure returns to normal.
Systemic vascular resistance (SVR): <800 dyne/sec/cm-5. SVR often low in early septic shock; may become elevated in later phases of septic shock.
Oxygen delivery (DO2): Cardiac index (CI) x arterial O2 content (A) = < 550 ml/min/m2. Try to provide sufficient DO2 to maintain adequate mixed venous O2 saturation.
Mixed venous O2 saturation: < 70%. Low mixed venous O2 indicates inadequate O2 delivery to tissues in sepsis.
Oxygen consumption (VO2): (CI) x (A-VO2) x 10 = > 180 L/min/m2. Typically increased in early septic shock.
Mortality in Emergency Department Sepsis (MEDS) score: designed to predict 28-day mortality in patients with suspected sepsis. The scoring system categorizes patients into risk groups based on the presence of nine independent predictors of mortality: terminal illness, tachypnea or hypoxia, septic shock, platelet count <150,000 cells/mm3, band proportion >5%, age >65, lower respiratory infection, nursing home residence, and altered mental status. The MEDS score is useful for risk stratification but not as a basis for treatment decisions (Crit Care Med 2008;36:625)…editorialist notes that serum lactate remains the clinical tool to use in the ED to help gauge severity of illness and to direct treatment decisions.
PIRO Classification System for Sepsis:
Taking into account parameters of predisposition, severity of infection, physiologic response, and organ failure (PIRO).
0 to 4 points for predisposition (a composite of age, chronic liver disease, and congestive cardiomyopathy).
0 to 4 points for severity of infection.
1 point for response (presence of both tachycardia and tachypnea).
0 to 4 points for the number of organ failures.
A simple classification system developed using data from patients with severe sepsis performed at least as well as established, complex scores (Crit Care Med 2009;37:1329)….Across the components, each 1-point increment increased mortality risk by 30% to 50%. In the PROWESS and PROGRESS data, correlations of PIRO total scores and in-hospital mortality rates were 0.974 and 0.998, respectively (for both, P<0.0001).
Lactate levels: like ScvO2, are a measure of tissue hypoxia. In a group of Dutch ICU, patients did better with lactate monitoring, but controversy remains (Am J Respir Crit Care Med 2010;182:752)….348 patients with sepsis and lactate levels 3 mEq/L were randomized to usual tx or an arm to decrease lactate levels by 20% every 2 hours for the initial 8 hours of a patient’s ICU stay…..The lactate group (who received more fluids and nitroglycerin than the control group) had a significant 9% absolute decrease in in-hospital mortality compared with the control group when the analysis was adjusted for predefined risk factors (34% vs. 43%)…..Surprisingly, no difference in lactate levels between the groups was noted at any time.
Tx of sepsis: Goal Directed | Xigris | Corticosteroids / Adrenal Insuff & Guidelines | Empiric Abx | Shock | Vasopressin |
Early goal-directed therapy (EGDT) for severe sepsis was associated with a nonsignificant relative mortality reduction according to a small prospective clinical trial (Chest 2007;132:425-32)…early empirical antibiotic therapy; IV fluids, vasopressors, mechanical ventilation, and blood transfusion, as necessary, to ensure central venous pressure 8 mm Hg, mean arterial pressure >65 mm Hg, and central venous oxygen saturation 70%. Employing supportive measures for organ dysfunction (e.g., lung-protective mechanical ventilation, adequate tissue perfusion) and treating the underlying illness (e.g., antibiotics for infection) remain the mainstays of managing critically ill patients. EGDT leads to better outcomes in septic patients. EGDT includes three sequential physiologic goals: intravenous fluids to achieve a central venous pressure of 8 to 12 mm Hg, pressors to attain a mean arterial pressure 65 mm Hg, and inotropes or red blood cell transfusions to achieve central venous oxygen saturation (ScvO2) 70% or mixed venous saturation 65%.
Sepsis Management Guidelines (first 6 hours): (South Med J. 2007;100:594-600)
Step #1: Measure serum lactate level to guide management.
Step #2: Obtain blood cultures before Abx administration. Correct, if possible, the disease that allowed bloodstream invasion (drain any pus under pressure).
Step #3: From the time of presentation, administer broad-spectrum Abx’s (see Empiric Abx) within 3 hours for ED admissions and within 1 hour for non–ED ICU admissions.
Step #4: Fluid resuscitation 4-6L crystalloid, + albumin titrated to PCWP of 10-20 using UO/ BP/ O2 delivery. In the event of hypotension and/or lactate level >4 mmol/L (36 mg/dL), deliver an initial minimum dose of 20 mL/kg of crystalloid (or colloid equivalent); use vasopressors for hypotension not responding to initial fluid resuscitation to maintain mean arterial pressure of >65 mm Hg.
Step #5: In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate level >4 mmol/L (36 mg/dL), achieve CVP of 8 mm Hg or greater and achieve central venous oxygen saturation of >70% or a mixed venous oxygen saturation of >65%.
During the first 24 hours:
1. Low-dose steroids should be administered for septic shock. Consider low-dose vasopressin (max 0.04 units/min) (effective for catecholamine-resistant septic shock, (Lancet 2002;359:1209). Meta-analysis suggests that longer-term lower-dose corticosteroids (200-300 mg of hydrocortisone or 0–75 mg of prednisone daily for 5 to 7 days) are associated with lower mortality in patients with septic shock (JAMA 2009;301:2388).
2. Glucose control should maintain glucose level at or above the lower limit of normal, but <150 mg/dL (8.3 mmol/L).
3. For mechanically ventilated pt’s, inspiratory plateau pressures should be maintained at <30 cm H2O. Even with early goal-directed therapy, starting appropriate antibiotics within 1 hour after diagnosis is essential for optimal outcomes (Crit Care Med 2010;38:1045).
Info: A meta-analysis of randomized sepsis trials showed mortality benefit with early goal-directed therapy (Crit Care Med 2008;36:2734)…..patients who received endpoint-directed resuscitation early (6 studies) demonstrated lower mortality with this procedure (OR, 0.50; 95% CI, 0.37–0.69)…..no mortality benefit resulted from late (>24 hours) resuscitation (OR, 1.16; 95% CI, 0.60–2.22).
Vasopressors & Inotropics if hypotension persists –> Dopamine (DA) is 1st line @ 5-20ug/kg/min. If hypotension persists despite high dose DA or if tachy –> NE @ 2-8ug/min or Epi @ 1-8 mcg/min.
• A meta-analysis shows that dopamine is associated with increased risk for death and arrhythmic events compared with norepinephrine in pt’s with septic shock (RR, 2.34)(Crit Care Med 2012;40:981)…….An editorialist suggests that dopamine, a more powerful beta-agonist than norepinephrine, could still be considered in patients with septic shock, hypotension (systolic blood pressure <90 mm Hg), and either a low cardiac index (<2.5 L/minute/m2) or low heart rate (<90 beats per minute) despite optimal use of norepinephrine.
If decr cardiac output –> Dobutamine to help with 02 delivery @ inotropic dose of 5-10ug/kg/min, vasodilator@ 15-20 mcg/kg/min.
Minimize O2 demand –> artificial respiration using paralysis or muscle relaxation, antipyretics for fever, optimize O2 delivery, incr cardiac output (fluids, presser, colloids).
Other: If CVP <8 give crystalloid or colloid until 8-12 mmHg. Aim to keep MAP 65-90 mmHg with vasoactive agents. If ScvO2 (central venous O2 sat) <70% transfuse with PRBC’s until HCT >30%, if still <70% start inotropes (NEJM 2001;345:1359).
Incr O2 content with –> supplemental O2, RBC transfusion.
Targeting lactate clearance levels improves mortality and shortens ICU stay, a multicenter randomized study shows (Am J Respir Crit Care Med 2010;online May 12th)…..the treatment algorithm started with continuous monitoring of central venous hemoglobin oxygen saturation (ScvO2), to balance oxygen delivery with demand. When ScvO2 was at least 70% but lactate clearance targets weren’t being met, patients received vasodilators with the goal of improving microvascular perfusion. Before the vasodilator infusions, the researchers checked fluid responsiveness and gave fluids as necessary.
Vasopressin: Infusion @0.01-0.04 units/min is associated with a lesser need for other vasopressors, gives hemodynamic support in septic & vasodilatory shock (Chest 2001;120:3).
Sepsis-Induced Immunosuppression: In a small cohort, 8 days of GM-CSF (4 µg/kg/day SQ for 5 days and then 4 or 8 µg/kg/day for 3 days) led to a significant increase in monocyte HLA-DR expression and some improvement in clinical parameters (Am J Respir Crit Care Med 2009;180:640)……In the GM-CSF group, mHLA-DR levels (expression of HLA-DR on the surface of circulating monocytes) were significantly higher at days 5 and 9 than at baseline. Moreover, mHLA-DR levels were normalized (>15,000 molecules/cell) by study day 9 in all 19 GM-CSF recipients versus only 3 of 19 placebo recipients (P<0.001). In addition, at day 9, GM-CSF recipients had required mechanical ventilation for a shorter time (mean, 147.9 vs. 207.2 hours; P=0.04) and had lower APACHE-II scores (mean, 16.7 vs. 20.8; P=0.06) than placebo recipients.
IVIG: Polyclonal IV immunoglobulin therapy should be considered as a potential adjuvant therapy in critically ill adults with sepsis (survival benefit of 32%, risk ratio = 0.68) (Meta-analysis of eighteen trials presented at the Toronto Critical Care Medicine Symposium. October 26th, 2005).
Statin: Simvastatin (80 mg/day x 10 days) appears to reduce in-hospital sepsis mortality by about half according to a small double-blind clinical trial (29th World Congress of Internal Medicine. 2008;Sept)…..might be explained essentially by the anti-inflammatory and antithrombogenic properties, and also might work by enhancing the vasodilation effect of nitric oxide.
• In a study of 69,198 pt’s hospitalized for cardiovascular disease, statin use was associated with a 19% decreased risk of subsequent sepsis (Lancet 2006;Jan 25 online) (dampens down the excessive immune reaction that occurs).
Other: Most recommend holding off on platelet transfusions until <20,000 unless evidence of bleeding or the need for an invasive procedure. Intensive insulin therapy to maintain BS 80-110mg/dL with early goal-directed adjustment of cardiac preload, afterload and contractility to balance O2 delivery/demand improves mortality
High-Dose Antithrombin III?: A nominal tx effect favoring AT-III was found in analyses of most subgroups. Bleeding as an adverse event occurred nearly twice as often in the AT-III group as in the placebo group (Crit Care Med 2006;34:285-92)…..as with the use of activated protein C in sepsis, it is difficult to understand why low-risk pt’s should not benefit. Editorialists emphasize the need for more studies. A meta-analysis found that treatment with Antithrombin III did not reduce mortality among critically Ill Patients (BMJ 2007;335:1248)…..Aggressive supportive care, including early airway management, blood pressure support, and other proven treatments (e.g., antibiotics for sepsis) remain the mainstays of therapy. Antithrombin III did not reduce mortality or other outcome measures in critically ill pt’s, but did increase bleeding risk according to a meta-analysis of 20 randomized trials involving 3458 patients (BMJ 2007;335:1248).
Early goal-directed therapy: If SIRS + source of infection + SBP <90 mm Hg after a 20 mL/kg fluid bolus, or lactate of 4 mmol/L or higher, or evidence of organ dysfunction.
Goals: Hemodynamic monitoring (CVP/ScvO2 ) within 2 hours. Broad spectrum Abx’s administered within 4 hours.
6 hours goal of: CVP of >8 mm Hg, MAP >65 mm Hg, ScvO2 >70%. Monitor for decreasing lactate; and administer steroid if the pt is on a vasopressor (SCCM 34th Critical Care Congress: Abstract 44. Presented Jan. 17, 2005).
Xigris (Drotrecogin, DrotAA = Activated Protein C =APC): In 10/11 Eli Lilly is withdrew it from all markets including the United States in the wake of a new study showing that the agent did no better than a placebo in reducing mortality. Was for age >18yo give 24ug/kg/hr IV infusion for 96hr. Cost >$8,000 per 4 days tx. For pt’s with septic shock who have an APACHE II score >25 or significant organ dysfunction. Gives a 6% benefit over placebo, 3.5% risk of serious bleeding (NEJM 2001;344:759). Drotrecogin does not benefit pt’s with sepsis and an APACHE II score of <25 (low-risk pt’s) (NEJM. 2005;353:1332-1341). A serine protease that it inhibits thrombosis, it normally gets consumed during sepsis, repleting it helps turn off both inflammation and coagulation to enhance fibrinolysis. Caution with heparin >15 u/kg/hr or INR >3.
• A meta-analysis of the sepsis drug drotrecogin alfa (activated) in real-life usage over the course of 10 years shows efficacy and safety rates similar to those reported in the randomized controlled trial that originally led to the drug’s approval (Lancet Infect Dis. Published online July 17, 2012)…..However, amid concerns that the drug was not effective in patients with less severe sepsis and children, researchers conducted a second clinical study, called PROWESS-SHOCK. The results of this trial did not favor the drug and resulted in Eli Lilly withdrawing the drug in October 2011.
Adrenal Insufficiency & Steroids: See Sepsis | Many pt’s with septic shock have relative adrenal insufficiency, which is associated with excess mortality.
• Data from 17,847 patients in the Surviving Sepsis Campaign does not support use of steroids in septic shock (Intensive Care Med 2012:Oct 12;e-pub ahead of print)…..Hospital mortality was significantly higher in patients who received low-dose steroids than in those who did not (41% vs. 35%; adjusted odds ratio, 1.18)…..Just over half of patients received low-dose steroids (50 mg IV QID or 100 mg TID), most within 8 hours of presentation……this observational study shows that administering steroids to septic patients does not improve outcomes and is not indicated.
• If pt’s random cortisol <15ug/dL or stimulated cortisol (1ug ACTH IV) <20 ug/dL (or delta value <9 ug/dL), may benefit from hydrocortisone 50mg q6-8hr (tapered after the pt has improved) (Clev Clin J Med 2005;72:427-32).
• Random serum free-cortisol level may be more accurate, especially if serum albumen is <2.5mg/dL, but not widely available. Low dose steroids such as 100mg hydrocortisone IV q8hr + Fludrocortisone (Florinef) 50ug PO via NGT X 7d reduces death (JAMA 2002;288:862-71).
• A 5-7 day course of physiologic hydrocortisone (200-300mg qd divided x5d) with subsequent tapering (over 5-7 days) increases survival rate and shock reversal in pt’s with vasopressor-dependent septic shock (Ann Int Med 2004;141:47-56).
• Some septic shock pt’s have relative adrenal insufficiency; thus, it is plausible that long courses of physiologic stress-dose steroids (as opposed to brief mega-dose therapy) would improve outcomes (BMJ 2004;329:480-4)….the authors recommend that pt’s with septic shock receive 200-300 mg of hydrocortisone qd after undergoing rapid ACTH testing and that those with relative adrenal insufficiency be treated for 5-11 days. In pt’s with septic shock, low-dose corticosteroids (50mg HC IV q6hr + 50-µg fludrocortisone qd x 7days) are beneficial mainly in those with ARDS and impaired adrenal reserve (= nonresponse to a short corticotropin stimulation test) (Crit Care Med 2006;34:22-30).
• Adrenal insufficiency is dx in 60% of pt’s with sepsis based on Metyrapone testing (no longer available in the US) (Am J Respir Crit Care Med 2006;174:1319-26)….Adrenal insufficiency was ruled in by a baseline cortisol level 10 µg/dL, or by an increase of <9 µg/dL after stimulation; adrenal insufficiency was ruled out by stimulated cortisol to a level 44 µg/dL, or by an increase of 17 µg/dL after stimulation.
• Continuous administration of low-dose hydrocortisone infusions (200 mg/day) reduced the number of hyperglycemic episodes and less nursing workload in pt’s with septic shock (Crit Care. 2007;00:Feb 16).
• Low-dose steroids have virtually no effect on all-cause mortality when used in pt’s with severe sepsis and septic shock, according to results from the Corticosteroid Therapy of Septic Shock study (CORTICUS) RCT with 499 pt’s…..Mortality rates at 28 days for septic shock did not differ between steroid (50 mg of IV HC q6 hrs x 5 days) and placebo groups, regardless of response to corticotropin testing (NEJM 2008;358:111)…..Presently, there is insufficient evidence to support steroid administration for sepsis with shock, regardless of a pt’s response to corticotropin testing.
Guidelines for Giving Steroids in Critically Ill Adult Patients:
(Consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med 2008;36:1937)
• Adrenal insufficiency in critically ill patients should be diagnosed either by a change in cortisol level of <9 µg/dL after administration of 250 µg of cosyntropin (delta cortisol test) or by a random total cortisol level of <10 µg/dL.
• Use of free cortisol levels cannot be recommended at this time (even though free cortisol measurement has advantages over total serum cortisol measurement), because the test is not available widely and its normal range in critically ill patients in unclear.
• The decision to administer glucocorticoids to patients with septic shock or early acute respiratory distress syndrome (ARDS) should be based on clinical criteria, not on results from adrenocorticotropic hormone (ACTH) stimulation testing. Six randomized controlled studies have shown that glucocorticoid treatment resulted in more-rapid shock reversal, and other randomized trials have shown that glucocorticoid treatment improved outcomes in patients with early ARDS. In both cases, benefits have been independent of results from ACTH testing.
• Hydrocortisone should be considered in management strategies for patients with septic shock, particularly those who exhibit limited response to fluid resuscitation and vasopressor agents. Intravenous hydrocortisone dosage should be 200 mg daily in four divided doses or as a bolus of 100 mg followed by continuous infusion at 10 mg/hour (240 mg daily).
• Moderate-dose glucocorticoids should be considered in management strategies for patients with early severe ARDS (PaO2/FiO2 <200) and before day 14 in patients with nonresolving ARDS. The optimal initial regimen in patients with early severe ARDS is methylprednisolone (1 mg/kg daily as a continuous infusion).
• The optimal duration of glucocorticoid treatment in patients with septic shock and early ARDS is unclear. Based on published results, duration of treatment for patients with septic shock should be at least 7 days before glucocorticoids are tapered (assuming no recurrence of sepsis or shock), and patients with early ARDS should be treated for at least 14 days before tapering begins. In both cases, drugs should be tapered slowly and should never be stopped abruptly.
• Treatment with fludrocortisone (50 µg orally once daily) is optional. Dexamethasone is not recommended for treatment of patients with septic shock or ARDS.
Septic shock prognosis: based on cortisol levels.
Short ACTH stimulation test: 0.25mg IV Tetracosactin given and blood samples checked at T-0, 30 and 60 min. Good prognosis (26% 28d mortality) if T-0 <34 mcg/dL and max change of 9. Intermediate (67% mortality) if T-0 >34 and max change >9. Poor prognosis (82% mortality) if T-0 >34 and max change <9 mcg/dL). Thus higher mortality if high baseline and weak cortisol response. (JAMA 2000;283:8) Some just give empiric hydrocortisone replacement @ 100mg IV qd if persistent hypotension. Free cortisol, not total cortisol, should be measured in critically ill hypoproteinemic pt’s, as >90% of circulating cortisol in human serum is protein-bound. A significant percentage of critically ill pt’s with hypoproteinemia may have below normal concentrations of serum total cortisol (and cosyntropin-stimulated serum total cortisol) in spite of having normal adrenal function.
• Measuring serum free cortisol concentrations may prevent unnecessary glucocorticoid therapy (NEJM 2004;350:1629-38).
Sepsis Guidelines:
(Crit Care Med. 2013;41:580)
Resuscitation Goals in First 6 Hours:
Central venous pressure 8 to 12 mm Hg (grade 1C)
Mean arterial pressure (MAP) =65 mm Hg (grade 1C)
Urine output =0.5 mL/kg/hour (grade 1C)
Antimicrobials: IV administration within 1 hour of recognition of septic shock (grade 1B) and severe sepsis without septic shock (grade 1C)
Fluids:
Crystalloids as first choice for initial fluid resuscitation (grade 1B)
Initial minimum crystalloid challenge of 30 mL/kg (grade 1C)
Vasopressors and Inotropes:
Norepinephrine as first choice (grade 1B) with epinephrine added or potentially substituted when adequate blood pressure cannot be maintained (grade 2B)
Phenylephrine not recommended except if norepinephrine is associated with serious arrhythmias, if cardiac output is high and blood pressure persistently low, or as salvage therapy when MAP target is not achieved (grade 1C)
Dobutamine infusion trial up to 20 µg/kg/minute administered or added to vasopressor in the case of myocardial dysfunction or ongoing signs of hypoperfusion (grade 1C)
Corticosteroids: No corticosteroids in the absence of refractory shock (grade 1D)
Blood Products: After tissue hypoperfusion is corrected, red blood cell transfusion only when hemoglobin concentration decreases to <7.0 g/dL, to a target hemoglobin concentration of 7.0–9.0 g/dL in adults (grade 1B)
The sepsis resuscitation bundle, which should be accomplished as soon as possible and scored during the first 6 hours, includes the following: (South Med J. 2007;100:594-600)
• Measure serum lactate level.
• Obtain blood cultures before antibiotic administration.
• From the time of presentation, administer broad-spectrum antibiotics within 3 hours for emergency department admissions and within 1 hour for non–emergency department ICU admissions.
• In the event of hypotension and/or lactate level greater than 4 mmol/L (36 mg/dL), deliver an initial minimum dose of 20 mL/kg of crystalloid (or colloid equivalent); use vasopressors for hypotension not responding to initial fluid resuscitation to maintain mean arterial pressure of 65 mm Hg or greater.
• In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate level greater than 4 mmol/L (36 mg/dL), achieve central venous pressure of 8 mm Hg or greater and achieve central venous oxygen saturation of 70% or greater or a mixed venous oxygen saturation of 65% or greater.
The sepsis management bundle, which should be accomplished as soon as possible and scored during the first 24 hours, includes the following:
• Low-dose steroids should be administered for septic shock, following a standardized ICU protocol.
• Activated drotrecogin alfa should be administered following a standardized ICU protocol.
• Glucose control should maintain glucose level at or above the lower limit of normal, but less than 150 mg/dL (8.3 mmol/L).
• For mechanically ventilated patients, inspiratory plateau pressures should be maintained at less than 30 cm H2O.
The initial empiric antimicrobial therapy used to treat septic shock may be the most important determinant of whether a patient will survive to hospital discharge as inappropriate therapy can reduce the chances of survival by fivefold or more (Chest 2009;136:1237-1248).
Combination regimens: The rate of appropriate empirical antibiotic therapy for severe sepsis was higher with combination treatment than with monotherapy (Antimicrob Agents Chemother 2010;54:1742)…..Hospital mortality was significantly greater when initial antibiotic therapy was inappropriate than when it was appropriate (52% vs. 36%)……The rate of appropriate antibiotic therapy was higher in patients who received combination therapy than in those who received monotherapy (78% vs. 64%; P<0.001)……Isolates resistant to the major beta-lactams were more likely to be susceptible to an aminoglycoside than to a quinolone. However, nephrotoxicity was significantly more common in patients who received an aminoglycoside than in those who did not (22% vs. 14%; P=0.014)……No difference was seen between monotherapy and combination therapy in the occurrence of Clostridium difficile–associated diarrhea.
• In two large cohort studies, combinations that included a beta-lactam showed beneficial effects in severe sepsis (Crit Care Med 2010;38:1773).
….All patients received empirical treatment with a beta-lactam, either alone (86%) or together with an aminoglycoside (14%); 10% of them died within 30 days. Factors independently associated with 30-day mortality included age >65, nosocomial infection, rapidly or ultimately fatal underlying disease, cirrhosis, previous corticosteroid treatment, shock on presentation, pneumonia, and inappropriate empirical therapy……with better outcomes. Martínez and colleagues’ study suggests that the benefit of combination regimens derives from increasing the chances that empirical therapy will be appropriate……additional benefit from “double coverage,” possibly related to faster killing of the pathogen.
Must take into account: a) the presumed primary anatomic site of the infection leading to bacteremia. b) local hospital antibiotic sensitivities. c) sensitivities for bacteria previously grown from possible sites of bacteremia. Empiric therapy must be readjusted based on blood culture results.
• A multi-site study with 2371 pt’s found that the survival rate was 83% in pt’s who received appropriate Abx txt within the first 30 minutes after onset of documented hypotension, and 77% in pt’s who received appropriate tx 30–60 minutes after onset (Crit Care Med 2006;34:1589-96)…over the next 5 hours, the survival rate decreased by ~ 8% per hour for each hour of delay in starting effective tx. IVIG reduces mortality in sepsis and septic shock (Cochrane Database Syst Rev 2001;2:CD001090).
Unknown Pathogen –> Nafcillin or Oxacillin (Vanc if nosocomial) + one of the following: Aminoglycoside (AG) + Flagyl or 3rd Gen Ceph (Ceftriaxone , Cefotaxime, Cefepime or Ceftazidime) + Flagyl or Imipenem or Meropenem or B-lactam-B-lactamase inhibitor (Ticarcillin-clav or piperacillin tazobactam) or IV quinolone + Flagyl.
Respiratory Tract Pathogen –> CAP use 3rd Gen Ceph + Macrolide or Quinolone such as Levofloxacin, Moxifloxacin has enhanced pneumococcal activity. Hospital acquired use 3rd gen ceph + AG + Vanc.
Biliary Tract Pathogen –> Usual microorganisms are Enterococcus Species, Enterobacteriaceae. Tx with TC/CL 3.1 g IV q6h or PIP/TAZO 3.375 g IV q6h or Amp-sulbactam 3 g IV q6h. Can also use (cefotaxime 2 g IV q8h or ceftizoxime 2 g IV q12h or ceftriaxone 2 g IV q12h) + metronidazole 500 mg IV q6h.
Neutropenia –> Ceftazidime or Meropenem or Imipenem or AG + Timentin (or Zosyn).
Pseudomonas –> AG + piperacillin or Ceftazidime or Cefepime.
Staph a –> start Nafcillin + Rifampin + Tobra, can use Cefazolin if Nafcillin not tolerated or need easier dosing schedule. If suspect MRSA start with Van + Rifampin.
Abdominal/ pelvic –> Enterobacteriaceae/ Anaerobes/ Enterococci –> Amp/ Sulbactam (Unasyn) or Timentin or Zosyn or Imipenem or Meropenem or Cefoxitin + Aminoglycoside. Or Amp-Gent-Flagyl or 3rd gen ceph + Flagyl or Cipro + Flagyl.
Decubitus Ulcers: polymicrobial, strep. pyogenes, group A strep, group C and G streptococcus, enterococcus species, anaerobic streptococcus, pseudomonas aeruginosa., bacteroides species, Staph aureus. Tx with imipenem 0.5 g IV q6h or Meropenem 1 g IV q8h or TC/CL3.1 g IV q6h or PIP/TAZO 3.375 g IV q6h. Can also use (ciprofloxacin 400 mg IV q12h or levofloxacin 500 mg IV qd + (clindamycin 900 mg IV q8h or metronidazole 1 g IV loading dose then 0.5 g IV 16h or 1 g IV q12h).
Urinary –> Enterobacteriaceae/ Enterococci –> Amp + Aminoglycoside. Or Quinolone. Or 3rd Gen Ceph + Aminoglycoside.
Petechial rash in child –> Meningococcus, H flu. –> Cefotaxime. Or Ceftriaxone.
Petechial rash in Adult –> Meningococcus, G- bacilli –> 3rd Gen Ceph + Aminoglycoside (use Ceftazidime if Pseudomonas suspected).
RMSF suspected –> R. rickettsii Abdominal/ pelvic –> IV Doxy or Chloramphenicol.
Toxic Shock Syndrome: staphylococcal aureus (toxin-mediated). Tx with Nafcillin or oxacillin 2 g IV q4h. Can also use Cefazolin 1-2 g IV q8h. If Streptococcal group A, group B, group C and G, strep. pyogenes give IVIG (150 mg/kg/day x 5 days) associated with increased survival. Tx with PCN G 24 million units IV qd div in q4-6h + clindamycin 900 mg IV q8h. Can also use Erythromycin 1 g IV q6h or Ceftriaxone 2 g IV qd + clindamycin 900 mg IV q8h.
• Outcomes were similar between meropenem alone and meropenem plus moxifloxacin in patients with severe sepsis (JAMA 2012:May 21;e-pub ahead of print).
Sepsis of Unknown Source:
Neonates: (<1 week old): typically due to Enterobacteriaceae, Listeria, GAS, Enterococci, group B strep, Escherichia coli, klebsiella species, Enterobacter species, Staph aureus (uncommon), listeria monocytogenes (rare). Blood cultures essential, but positive in only 5-10% of cases. Can discontinue ATB after 72 hours if cultures negative and clinical course favorable. Tx with Ampicillin 25 mg/kg IV q8h + cefotaxime 50 mg/kg IV q12h. Can also use Ampicillin 25 mg/kg IV q8h + gentamicin or tobramycin 2.5 mg/kg IV/IM q8h or Ampicillin 25 mg/kg IV q8h + ceftriaxone 50 mg/kg IV/IM qd. –> Amp + Cefixime (if meningitis is suspected) Or Gent + Nafcillin.
Child Neonatal (1-4 weeks old): typically due to group B strep, Escherichia coli, klebsiella species, Enterobacter species, Staph aureus (uncommon), listeria monocytogenes (rare), haemophilus influenzae and Staph epidermidis. Tx with Ampicillin 25 mg/kg IV q8h + cefotaxime 50 mg/kg IV q12h or Ampicillin 25 mg/kg IV q8h + ceftriaxone 75 mg/kg IV/IM qd. Can also use Ampicillin 25 mg/kg IV q8h + gentamicin or tobramycin 2.5 mg/kg IV/IM q8h.
Children: Pneumococcus, H flu, meningococcus, S. aureus, neisseria meningitidis –> Tx with Cefotaxime 50 mg/kg IV q12h or Ceftriaxone 100 mg/kg IV/IM qd or Cefuroxime 50 mg/kg IV qd. Can also use (nafcillin or oxacillin 2 g IV q4h) + cefuroxime 50 mg/kg IV qd.
Adults: Community acquired Enterobacteriaceae, S. aureus, Strep –> Nafcillin or Oxacillin (Use Vanc if infection is nosocomial).
Plus one of the following: Flagyl + 3rd Gen Ceph (Ceftriaxone, Cefotaxime, Cefepime or Ceftazidime) or Flagyl + Aminoglycoside or IV quinolone + Flagyl. Or add Meropenem, Imipenem, Timentin or Zosyn. Imipenem 0.5 g IV q6h or Meropenem 1 g IV q8h or (gentamicin or tobramycin 2 mg/kg IV load then 1.7 mg/kg IV q8h) + (cefotaxime 2 g IV q8h or ceftizoxime 2 g IV q12h or ceftriaxone 2 g IV q12h or TC/CL 3.1 g IV q6h or PIP/TAZO 3.375 g IV q6h). If MRSA suspected: add vancomycin 1 g IV q12h. If ERV suspected: Synercid 7.5 mg/kg IV q8h or linezolid 600 mg IV q12h.
IV drug user –> S. aureus, G-, Enterococci –>Nafcillin or oxacillin 2 g IV q4h + (gentamicin or tobramycin 2 mg/kg IV load then 1.7 mg/kg IV q8h). Can also use Vancomycin 1 g IV q12h + (gentamicin or tobramycin 2 mg/kg IV load then 1.7 mg/kg IV q8h).
Immunocompromised/ neutropenic of any age: G- (P. aeruginosa), S aureus, aerobic gram-negative bacilli (including pseudomonas aeruginosa) of most concern, Staph aureus, fungi (aspergillus species, candida species), streptococcus species –> Ceftazidime & Aminoglycoside + Vancomycin (add for S epidermidis/ evidence of line infection). Or Piperacillin/ Tazobactam & Aminoglycosides, imipenem or Meropenem.
Monotherapy adult: Ceftazidime 2 g IV q8h or Imipenem 0.5 g IV q6h or Cefepime 2 g IV q8h. Monotherapy in Children: Ceftazidime 50 mg/kg IV q8h or Imipenem 10-15 mg/kg IV q6h (max 2 g/day) or Cefepime 150 mg/kg/day div. in q8h.
Duotherapy Adult: (gentamicin or tobramycin 2 mg/kg IV load then 1.7 mg/kg IV q8h) + (ticarcillin or piperacillin 3 g IV q4h or TC/CL 3.1 g IV q4h or PIP/TAZO 3.375 g IV q4h) or (gentamicin or tobramycin 2 mg/kg IV load then 1.7 mg/kg IV q8h) + ceftazidime 2 g IV q8h. Vancomycin 1 g IV q12h added to mono or duotherapy on clinical grounds or prevalence of MRSA or highly resistant S. pneumoniae.
Duotherpy in Children: (gentamicin or tobramycin 2.5 mg/kg IV q8h) + (ticarcillin 75 mg/kg IV q6h or piperacillin 100-300 mg/kg/day div. in q4-6h or TC/CL 75 mg/kg IV q6h or PIP/TAZO 100-300 mg/kg/day div. in q4-6h) or Gentamicin or tobramycin 2.5 mg/kg IV q8h + ceftazidime 2 g IV q8h. Vancomycin 40-60 mg/kg/day IV div. in q6h added to mono or duotherapy on clinical grounds or prevalence of MRSA or highly resistant S. pneumoniae.
**Ref: (Treating pt’s with severe sepsis. NEJM 1999;340:3) (Strategies for tx of sepsis, NEJM 1997;336:952-3) (Sepsis. Infect Dis Clin NA 1999;13:2) (Sepsis. Clin Chest Med 1996;17:2) (Familial Mediterranean fever. Lancet 1998;351:659) (Pathophysiology and tx of sepsis. NEJM 2003;348:138-148) (Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








