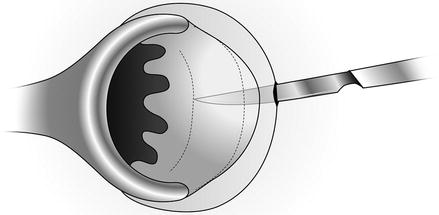
Figure 28.1
Anal fissure in posterior midline
Preoperative Care
Approximately half of all fissures resolve with conservative management, which consists of increased fiber and water intake and warm sitz baths. These measures have been found to heal nearly all fissures [1, 4, 5]. Various medical treatments may also be considered, including topical calcium channel blockers and botulinum toxin injection [5]. Medical therapies have been found to promote healing by decreasing sphincter pressures, however success rates are variable [6, 7]. Patients with persistent fissures or those associated with severe pain are candidates for surgical intervention [1, 4].
Indications for Surgical Approach
Lateral internal sphincterotomy (LIS) is the gold standard of treatment for chronic anal fissures with cure rates >90 % [1, 8]. Improvement in quality of life has also been described following LIS [9]. Overall, post-operative complications after this procedure are quite rare. While there is a potential risk of post-operative incontinence, incontinence rates after LIS have been found to be lower than reported in patients treated with medical therapies, such as calcium channel blockers and botulinum toxin injections [9, 10].
Description of Procedure
Positioning and choice of anesthesia are determined at the discretion of the surgeon. Many surgeons prefer the prone-jackknife position or high lithotomy for this procedure. General anesthesia is typically preferred, although a direct anal block may also be used. No preoperative bowel preparation is required.
Either a closed or open sphincterotomy may be performed, as both procedures have been found to result in similar outcomes [11]. In a closed sphincterotomy, the internal sphincter muscle is divided without incising the overlying anoderm. First, the groove between the internal and external sphincter is palpated and the index finger of the nondominant hand is inserted into the anal canal. A generous amount of 1 % lidocaine is injected into the intersphincteric groove. Then a No. 11 scalpel is inserted with the blade parallel to the fibers of the internal sphincter (Fig. 28.2). The blade is advanced to the dentate line, approximately 1.5 cm, or to the level of the apex of the fissure, and the scalpel is rotated 90° toward the mucosa. The knife is then advanced toward the inserted index finger with a sawing motion until the internal sphincter is transected taking care to not penetrate the mucosal surface (Fig. 28.3). The scalpel is removed and any remaining fibers are transected. This may be repeated on the opposite side of the anal canal if a deficiency cannot be palpated. Pressure should be applied to any bleeding. A foam sponge is then inserted to prevent hematoma formation. The sponge will be expelled during the patient’s next bowel movement. Dry gauze over the wound can be removed on postoperative day 1.