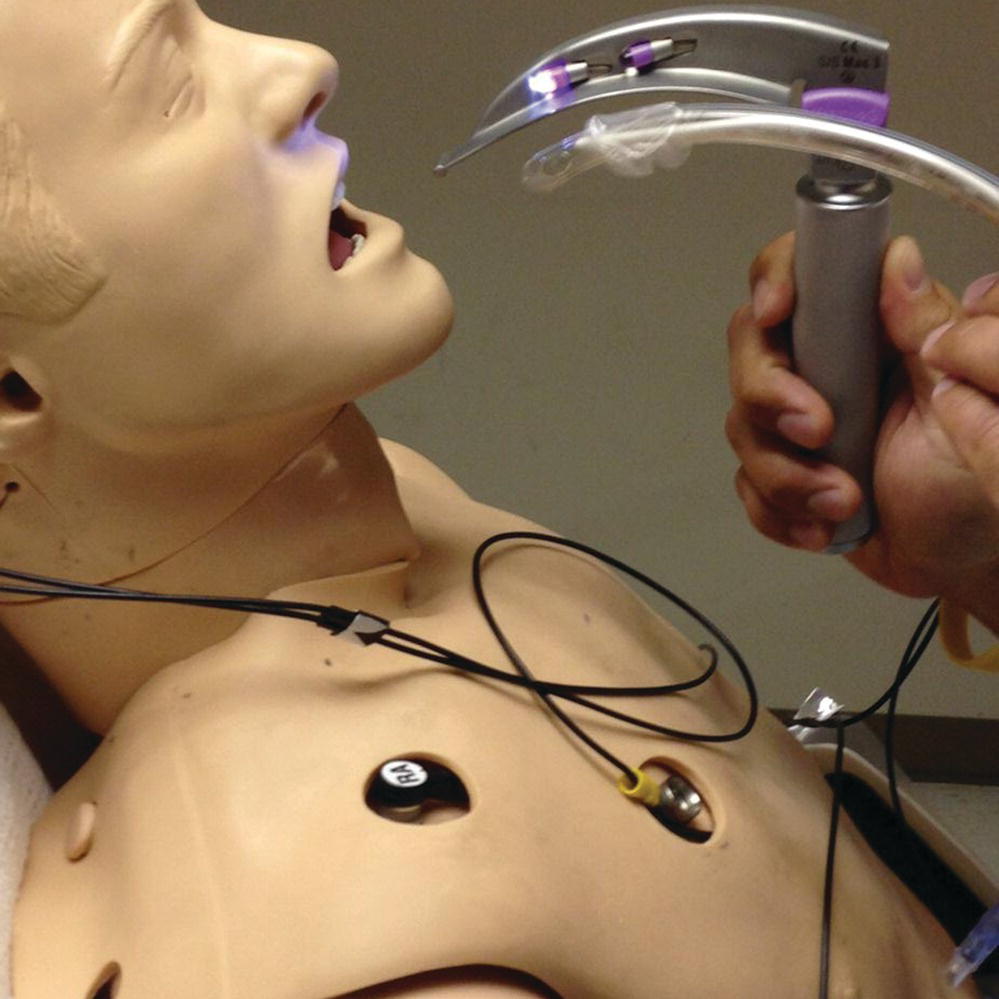
Chapter 4 Brendan Anzalone and Henry E. Wang The prehospital environment presents unique challenges or barriers to patient care. Airway management in these situations may be difficult or impossible. For example, airway management may need to be carried out with the patient on the floor or upright while entrapped in a vehicle. This chapter describes considerations and strategies for airway management in special prehospital situations. The classic position for intubation has the patient supine at the level of the rescuer’s xiphoid. However, prehospital patients requiring airway management are often found in unusual positions, such as on the ground. Conventional approaches to laryngoscopy and intubation must be modified in these scenarios. There are several approaches to rescuer positioning for ground-level endotracheal intubation (ETI). Figure 4.1 Prone intubation. Figure 4.2 Left lateral decubitus intubating position. Figure 4.3 Kneeling intubation. Figure 4.4 Sitting intubation. Figure 4.5 Straddle intubation. Because prehospital patients are frequently found and treated at ground level, rescuers should learn each of these techniques. Note that compared with traditional positioning, the rescuer’s face is closer to the patient’s oropharynx with ground-level intubation, and thus visualization of glottic structures may differ from conventional approaches. Pinchalk et al. describe a technique involving tilting the patient upwards (using the stretcher back or a backboard) to afford improved visualization of and access to the airway [1]. Limited studies suggest that the left lateral decubitus (LLD) positioning may result in higher intubation success rates than the other ground-level techniques. Adnet et al. compared the LLD intubating position versus kneeling with the patient (mannequin) supine on the ground, finding that the LLD position afforded better glottic exposure [2]. A follow-up study of EMS ground level intubations by Adnet et al. again studied LLD positioning versus kneeling in real EMS patients as opposed to mannequins [3]. During this study, they found that provider incidence of laryngoscopic difficulty was lower in the LLD position: 11.1% versus 26.9% for the kneeling group. They also found that there were a higher number of intubation attempts in the kneeling group than the LLD position. This research group postulated that LLD was a better position than kneeling for three reasons: the operator has better visual alignment with the larynx in the LLD position, the left forearm acts as a lever during exposure which minimizes operator effort, and the right arm is completely free during the procedure for tube placement and suctioning [3]. The rescuer’s ability to visualize the glottis during ground-level intubation may be altered. Video laryngoscopy has been proposed as an adjunct for facilitating ground-level intubation. Komatsu et al. evaluated the Airway Scope™ (Pentax) and Macintosh laryngoscope for tracheal intubation in patients lying on the ground [4]. While both the Airway Scope and Macintosh blade had high intubation success rates (98% and 100%, respectively), time to intubation was 17 seconds faster with the Airway Scope. A patient may require intubation while positioned upright; for example, when entrapped in a car. One described approach is to perform ETI while directly facing the patient. With this technique, the operator holds the laryngoscope with the right hand, inserting the laryngoscope blade in an inverted fashion (“tomahawk” or “ice axe” approach) and passing the tracheal tube with the left hand (Figure 4.6). Figure 4.6 Face-to-face “tomahawk” intubation position. In a mannequin study, Wetsch et al. studied face-to-face intubation comparing five types of video laryngoscopes and traditional Macintosh laryngoscopy in a simulated model of an entrapped motor vehicle victim [5]. Interestingly, their findings noted that the fastest time to intubation was with traditional Macintosh laryngoscopy, although the video laryngoscopes provide a better view of the glottis. Of the five video layngoscopes studied, the authors did note a shorter time to intubation with the two devices that had tube guides (Airtraq™ and Ambu Pentax™) than the non-guided scopes. Amathieu et al. also examined face-to-face mannequin intubation times with the LMA Fastrach™, Glidescope™, and Airtraq laryngoscopes [6]. Time to intubation was shorter, intubation success rate was higher, and perceived intubation difficulty was lower with the Airtraq. Silverton et al. compared glottic views during face-to-face Glidescope laryngoscopy and fiberoptic intubation. They noted the Glidescope could be used to obtain adequate intubation visualization in live humans [7]. When face-to-face intubation is the only available option, the provider should assess whether immediate airway intervention or patient extrication is most appropriate. The estimated time of extraction combined with patient condition may influence the decision-making process. High-flow oxygen devices and supraglottic airways may provide suitable alternatives in these situations. Optimal lighting is important in airway management. Increased ambient lighting allows for better gear preparation and procedure execution. EMS practitioners may need to perform airway management in suboptimal lighting conditions such as at night, while conducting military operations, in a confined space rescue, or in indoor areas with poor lighting. There are two major lighting considerations in prehospital airway management: the light illuminating the patient environment, and illumination of the airway. Simple interventions can significantly improve available lighting. Could a family member or colleague turn on additional lights? At the site of an accident, can portable lighting be provided to illuminate the scene? In some cases, a flashlight or headlamp may provide vital additional illumination.
Airway management: special situations
Introduction
Ground-level airway management





Face-to-face intubation
Intubating under low light conditions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




