Chapter 45 Advanced nursing roles
Advancing nursing practice is a global phenomenon: in the context of the Australian experience, this has evolved over the past three and a half decades. The evolution of advance nurse practice is an ongoing process moving nursing practice forward for the benefit of the patient.1 This change of practice is directly related to changes in the delivery of healthcare services and the implementation of new models of patient-focused care. An important driver in the development of the advance practice nurse is the political demand to meet government-set performance indicators and benchmarks aimed to reduce emergency department waiting times and patient length of stay and to increase patient satisfaction.2 Another factor that has contributed to evolving advance practice is medical and nursing workforce shortages and skill mix problems. These developments have provided the impetus for emergency nurses to take on new opportunities to develop and increase their scope and complexity of practice in the field of emergency medicine. These advance nursing roles are now core roles that work with and support the medical and clerical staff to expedite the patient’s journey through the emergency department.
THE TRIAGE NURSE
The patient’s journey in the emergency department begins at triage. Triage is an essential function in the delivery of care in all emergency departments. It is the point at which emergency care begins. Triage is a brief clinical assessment that determines the urgency of treatment and the time sequence in which patients should be seen in the emergency department. The purpose of the triage system is to ensure safe quality of care and equity of access to health services. In all healthcare environments, the triage process is underpinned by the premise that a reduction in the time taken to access definitive medical care will improve patient outcomes.3
In Australasian emergency departments a standardised triage system known as the Australasian Triage Scale (ATS) is the primary clinical tool for ensuring patients are seen in a timely manner, commensurate with their clinical urgency. The practical application of the ATS is the process by which the triage nurse assesses a patient’s presenting complaint, which is identified by a brief history of the presenting illness or injury. Triage decisions using the scale are made on the basis of observation of general appearance, focused clinical history and physiological data.4 This decision-making process may also require consultation and discussion with medical staff.
In practical terms triage refers to two domains, which are:
Domain 1. The ATS has five levels of acuity that categorise patients according to a rating scale from 1 to 5. (Also see Chapter 39, ‘Psychiatric presentations’, Table 39.1 Mental health triage.)
Table 45.1 ATS categories for treatment acuity, performance thresholds and examples of possible presenting problems
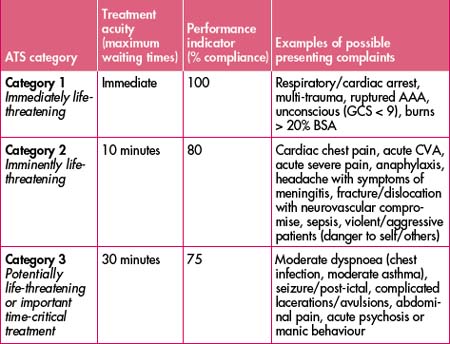
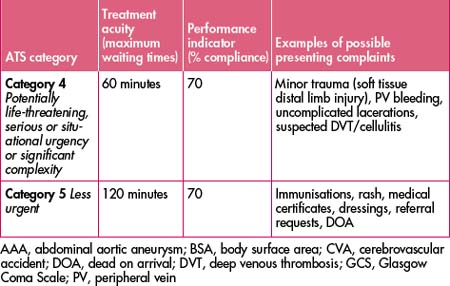
Domain 2. Time-to-treatment criteria attached to the ATS.
Please refer to Table 45.1 for triage examples.
There are five core components for a nurse undertaking the role of triage nurse:
Step 3. Always ask the question: ‘Does this person look sick?’
Step 5. Other conditions in which timely intervention may significantly influence outcomes (such as thrombolysis, an antidote or management of acid or alkali splash to eye) must also be detected at triage.
Step 6. Timely access to emergency care can improve patient outcomes.
Step 7. Early identification of physiological abnormality at triage can inform focused ongoing medical assessment and investigation.6
CLINICAL INITIATIVES NURSE (CIN)
Nurses working at CIN level should have:
The CIN role enables the nurse to commence patient treatment via pre-approved standing orders for specific presentations under the supervision of an emergency department registrar or consultant.
Box 45.1 Example 1. Patient presenting with an ankle fracture
AGED SERVICE EMERGENCY TEAM (ASET)
The specific objectives of this team include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







