Adult, Pediatric, and Newborn Resuscitation
Peter L. Bekker
Somaletha Bhattacharya
Richard M. Pino
I. OVERVIEW
Cardiopulmonary resuscitation (CPR) in the operating room (OR) is the responsibility of the anesthesiologist who knows the location and function of resuscitation equipment, delegates tasks, and instills calmness in assisting personnel. The algorithms described below have been modified as appropriate for the anesthesiologist in a hospital setting but closely follow the evidenced-based 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care that includes basic life support (BLS), advanced cardiac life support (ACLS), and pediatric advanced life support (PALS). Essential to the swift return of spontaneous circulation (ROSC) after a sudden cardiac arrest (SCA) is defibrillation for ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), the prompt delivery of effective, minimally interrupted chest compressions to maintain cerebral and cardiac perfusion, and the avoidance of hyperventilation that may cause continued hypotension through a decrease venous return to the heart. Effective compressions deliver oxygen and energy substrates to the myocardium and increase the likelihood that a perfusing rhythm will return after defibrillation. It is important that CPR be resumed immediately after defibrillation without pause for pulse or rhythm checks. When defibrillation terminates VF and ROSC occurs, continuation of chest compressions is often required, since the myocardium has been depleted of oxygen and metabolic substrates and is “stunned.” Table 38.1 lists the classifications for the quality of evidence used to support most of the protocol interventions presented in this chapter.
II. CARDIAC ARREST
A. Diagnosis. The absence of a palpable pulse in a major peripheral artery (carotid, radial, or femoral) in an unconscious, unmonitored patient is diagnostic. An electrocardiogram (ECG) may reveal a nonperfusing rhythm (asystole, VF, VT) or an organized rhythm (as for PEA).
B. Etiologies. Common causes of cardiac arrest are
1. Hypoxemia
2. Acid-base disturbances
3. Derangements of potassium, calcium, and magnesium
4. Hypovolemia
5. Adverse drug effects
6. Pericardial tamponade
7. Tension pneumothorax
8. Pulmonary embolus
9. Hypothermia
10. Myocardial infarction
TABLE 38.1 Evidence Classification for Interventions | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
C. Pathophysiology. If CPR is not immediately started after a cardiac arrest, the cessation of blood flow causes tissue hypoxia, anaerobic metabolism, accumulation of cellular wastes, and permanent organ damage. Acidosis from anaerobic metabolism may cause systemic vasodilation, pulmonary vasoconstriction, and decreased responsiveness to the actions of catecholamines.
III. ADULT RESUSCITATION
A. Basic life support (BLS) includes those fundamental principles that are taught to the general public but applies equally to OR situations. A cardiac arrest should be suspected in any person unexpectedly found unconscious. If the subject cannot be aroused, the 2010 AHA guidelines for CPR and ECC stress immediate activation of the emergency response system and initiation of chest compressions to provide Circulation prior to Airway management and Breathing (C-A-B). The vast majority of cardiac arrest in adults is due to VF or pulseless VT, etiologies in which early chest compressions and defibrillation are most critical. The C-A-B sequence minimizes delay associated with opening the airway and associated positioning, obtaining a seal for mouth-to-mouth breathing, or obtaining bag-mask equipment. Beginning with chest compressions may also increase likelihood that bystanders will perform CPR on persons who have suffered from SCA, since laypersons and some health care providers may find airway management a challenging first step and therefore be hesitant to initiate CPR. For lone rescuers, the lay public is taught the “phone first/phone fast” rule (evidence class indeterminate). For adults, children aged 8 years and older, and all children known to be at high risk for arrhythmias, the emergency medical system (911; EMS) should be activated (phone first) before attempts at resuscitation by a lone rescuer. An initial resuscitation attempt followed by the activation of EMS (“phone fast”) is indicated for children less than 8 years old and for all ages in cases of submersion or near drowning, arrest secondary to trauma, and drug overdose.
1. Circulation. The patient should be on a firm surface (e.g., backboard) with the head on the same level as the thorax. The rescuer (surgeon in the OR) compresses the sternum between the nipples with the heel of one hand, the other hand on top of the first so that the hands are overlapped and parallel (evidence class IIa), shoulders positioned directly over the patient, and elbows locked to depress the chest to a depth of 1.5 inches (infants) and of at least 2.0 inches in children and a normal-sized adult. The chest compression rate is 100/minute at a compression-relaxation ratio of 1:1. For a single rescuer, the compression-ventilation ratio is 30:2.
Unlike adults, in children, the compression-ventilation ratio becomes 15:2 if there are 2 rescuers. For a prone patient in the OR who cannot be quickly turned supine for CPR, one rescuer can place a clenched fist between the subxiphoid area and the OR table while compressions are administered over the corresponding region of the back. If an advanced airway (i.e., endotracheal tube or laryngeal mask airway) is in place during two-rescuer CPR, ventilations should be given at a rate of 8 to 10 breaths/min, chest compressions at a rate of 100/min without pauses for ventilation, and compressions are not synchronized between breaths.
Unlike adults, in children, the compression-ventilation ratio becomes 15:2 if there are 2 rescuers. For a prone patient in the OR who cannot be quickly turned supine for CPR, one rescuer can place a clenched fist between the subxiphoid area and the OR table while compressions are administered over the corresponding region of the back. If an advanced airway (i.e., endotracheal tube or laryngeal mask airway) is in place during two-rescuer CPR, ventilations should be given at a rate of 8 to 10 breaths/min, chest compressions at a rate of 100/min without pauses for ventilation, and compressions are not synchronized between breaths.
2. Airway and breathing. Spontaneous ventilation is evaluated by observation and auscultation and is aided by repositioning (chin lift and jaw thrust) or insertion of an oropharyngeal or nasopharyngeal airway. If the patient is apneic or has ineffective spontaneous breaths (e.g., gasping only), rescue breathing or ventilation by bag-valve-mask with 100% O2 is started. Two slow breaths at low airway pressures (to limit gastric distention) are first given, followed by ventilation with a respiratory rate of 8 to 10 breaths/min. If ventilation is not possible after these maneuvers, efforts to clear the airway of a suspected foreign body (e.g., Heimlich maneuver, chest compressions, or manual removal) should be attempted.
3. Defibrillation within 3 minutes in the hospital (evidence class I) and 5 minutes after calling the EMS (along with immediate high-quality CPR) is the major determinant of a successful resuscitation, since VF is the most likely etiology of a cardiac arrest in adults. Public access defibrillation programs have enabled “level I” responders (e.g., fire personnel, police, security guards, and airline attendants) to employ readily accessible automated external defibrillators (AEDs). AEDs are small, lightweight devices that use adhesive electrode pads for both sensing and delivering shocks. Visual and voice prompts are provided to assist the operators. The AED, after analysis of the frequency, amplitude, and slope of the ECG signal, advises either “shock indicated” or “no shock indicated.” The AED is manually triggered and does not automatically defibrillate the patient. AEDs are now also equipped with pediatric pad-cable systems that attenuate the adult dose to smaller dose appropriate for children. The dose attenuators should be used in children less than 8 years of age and less than 25 kg in weight. For infants, manual defibrillator is recommended but if unavailable AED with or without an attenuator can be used.
4. Reassessment. CPR should be resumed immediately after defibrillation (without checking for a pulse or rhythm) and continued for five cycles (or about 2 minutes if an advanced airway is in place) after which time the rhythm should be checked. For health care providers, if there is evidence for a perfusing rhythm, the pulse should be checked to determine if there is ROSC. If a nonshockable rhythm or no pulse is detected, CPR should be resumed, with rhythm checks every five cycles.
B. Advanced cardiac life support, including endotracheal intubation, electrical defibrillation, and pharmacologic intervention, is the definitive treatment for cardiac arrest.
1. Intubation. Swift control of the airway optimizes oxygenation and the removal of carbon dioxide during resuscitation. Endotracheal intubation by the most experienced person present should minimally disrupt other resuscitative measures. Quantitative waveform capnography should be used to confirm and monitor endotracheal tube placement. The endotracheal tube may be used to deliver certain drugs like naloxone, atropine, vasopressin, epinephrine, or lidocaine (NAVEL) if
intravenous (IV) access has not been established. Higher doses (two to three times) of these drugs diluted in 10 mL of sterile saline should be used, since peak drug concentrations are lower with the endotracheal route compared to IV administration.
intravenous (IV) access has not been established. Higher doses (two to three times) of these drugs diluted in 10 mL of sterile saline should be used, since peak drug concentrations are lower with the endotracheal route compared to IV administration.
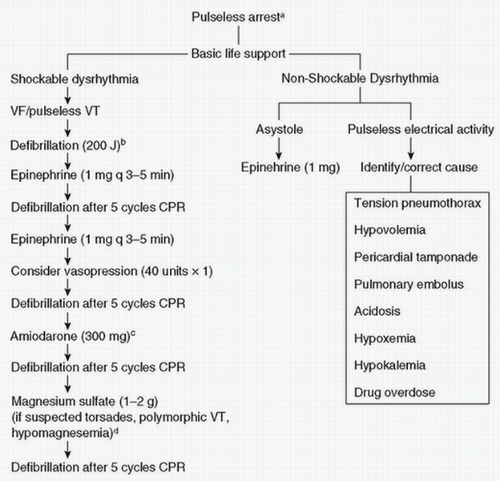
2. Defibrillation. Pulseless VT and VF are the most common dysrhythmias associated with a cardiac arrest (Fig. 38.1). As the duration of an SCA increases, cardiac function worsens and it becomes more difficult to convert to ROSC. Defibrillation is the priority and can often be administered by the anesthetist without compromising the surgical field. It is the responsibility of the person operating the defibrillator to ensure that members of the resuscitation team are not in contact with the patient during defibrillation.
a. Defibrillators deliver energy in a biphasic pulse that flows in a positive direction for specified milliseconds followed by reversal of current flow in the negative direction. The optimal dose determined to terminate VF is 150 to 200 J and is indicated on the front of the
defibrillator. In children, an initial dose of 2 to 4 J/kg is advised, and the dose can be increased with successive shocks. The dose should not exceed 10 J/kg or the maximum adult dose. The large adult paddles (8 to 13 cm) are recommended in children above 1 year of age and at least 10 kg in weight. Infant paddles (4.5 cm) are used in children less than 10 kg in weight.
defibrillator. In children, an initial dose of 2 to 4 J/kg is advised, and the dose can be increased with successive shocks. The dose should not exceed 10 J/kg or the maximum adult dose. The large adult paddles (8 to 13 cm) are recommended in children above 1 year of age and at least 10 kg in weight. Infant paddles (4.5 cm) are used in children less than 10 kg in weight.
b. Cardioversion using synchronized biphasic shocks of 50 to 100 J is used for supraventricular arrhythmias such as paroxysmal supraventricular tachycardia (PSVT). The recommended initial biphasic energy dose for cardioversion of atrial fibrillation is 120 to 200 J, depending on the manufacturer of the device; dosing can be increased in stepwise fashion is initial shock is ineffective. Hemodynamically stable VT can be cardioverted using 100 J as the starting point. The initial dose for cardioversion in children is 0.5 to 1 J/kg followed by subsequent doses of 2 J/kg.
3. Pacing. High-grade heart block with profound bradycardia is one etiology of cardiac arrest. Temporary pacing should be used when the heart rate does not increase with pharmacologic therapy. Transcutaneous pacing is the easiest method to increase the ventricular rate. Transesophageal atrial pacing is efficacious for sinus bradycardia with maintained atrioventricular (AV) conduction and is useful intraoperatively for bradycardia-related hypotension in otherwise stable patients. Transvenous pacing via a temporary wire into the right heart is a third option to increase heart rate while CPR continues. Special pacing pulmonary artery catheters are capable of AV pacing.
4. IV access is imperative for a successful resuscitation, though establishment of venous access should not delay chest compressions or defibrillation (when appropriate). The most desirable route is into the central circulation. The insertion site (internal jugular, external jugular, subclavian, or femoral vein) is predicated based on the anatomy of the patient, experience of the physician, and what is the least disruptive to the resuscitation. Peripheral IV catheters in antecubital veins are adequate when an appropriate volume is used to flush medications toward the central circulation. If peripheral vascular access is not easily established, intraosseous (IO) cannulation should be attempted. IO access can be done in less than a minute in children. All drugs and fluids can be given through an IO route till good IV access is obtained.
5. Drugs. The drugs described below are used in ACLS protocols for the treatment of hemodynamic instability, myocardial ischemia and infarction, and arrhythmias. The doses of drugs used for Pediatric Advanced Life Support (PALS) are in parentheses following discussion of adult doses.
a. Adenosine, an endogenous purine nucleoside with a half-life of 5 seconds, slows AV nodal conduction and interrupts AV node reentry pathways to convert a PSVT to a sinus rhythm. It also assists in the differential diagnosis of supraventricular tachycardia (e.g., atrial flutter with a rapid ventricular response versus PSVT). Adenosine can also be considered in the diagnosis and treatment stable, regular wide complex monomorphic tachycardia. The initial dose is a 6 mg rapid IV bolus. A brief asystole ensues, followed by P waves, flutter waves, or fibrillation waves that are initially without ventricular responses. PSVT is sometimes converted to a sinus rhythm by the 6 mg dose. A second injection of 12 mg may terminate PSVT if the first dose is unsuccessful. Recurrent PSVT, AF, and atrial flutter will require longer-acting drugs for definitive treatment. The dose of adenosine should be increased in the presence of methylxanthines
(competitive inhibition) and decreased if dipyridamole (potentiation via blockage of nucleoside transport) has been administered (PALS: 0.1 mg/kg; repeat dose 0.2 mg/kg; maximum dose 12 mg).
(competitive inhibition) and decreased if dipyridamole (potentiation via blockage of nucleoside transport) has been administered (PALS: 0.1 mg/kg; repeat dose 0.2 mg/kg; maximum dose 12 mg).
b. Amiodarone is the most versatile drug in the ACLS algorithms. It has the properties of all four classes of antiarrhythmics (lengthening of action potential, sodium channel blockade at high frequencies of stimulation, noncompetitive antisynaptic actions, and negative chronotropism). Because of its high efficacy and low incidence of proarrhythmic effects, it is the preferred antiarrhythmic for patients with severely impaired cardiac function. For pulseless VT and VF, 300 mg diluted in 20 to 30 mL of saline or 5% dextrose in water (D5W) is administered rapidly. To treat stable dysrhythmias (e.g., hemodynamically stable AF), 150 mg is administered over 10 minutes, followed by an infusion of 1 mg/min for 6 hours, and then 0.5 mg/min. The maximum daily dose is 2 g. Immediate side effects can be bradycardia and hypotension (PALS: loading dose, 5 mg/kg; maximum dose, 15 mg/kg/day). Amiodarone is indicated in the following arrhythmia situations.
1. Unstable VT (evidence class IIb)
2. VF or pulseless VT after failed electrical defibrillation and epinephrine treatment (evidence class IIb)
3. Attempted rate control during stable monomorphic VT, polymorphic VT (evidence class IIb), or AF (evidence class IIa)
4. Attempted ventricular rate control of rapid atrial arrhythmias when digitalis is ineffective (evidence class IIb) or when the tachycardia is secondary to accessory pathways (evidence class IIb)
5. Need for an adjunct to electrical cardioversion of refractory PSVT (evidence class IIa) or atrial tachycardia (evidence class IIb)
c. Atropine is useful in the treatment of hemodynamically significant bradycardia (evidence class I) or AV block occurring at the nodal level (evidence class IIa). It increases the rate of sinus node discharge and enhances AV node conduction by its vagolytic activity. The dose of atropine for bradycardia or AV block is 0.5 mg repeated every 3 to 5 minutes to a total dose of 0.04 mg/kg. Atropine is not indicated for asystole but should be considered for treatment of a profound bradycardia that may appear as asystole. Full vagal blockade is obtained at a cumulative dose of 3 mg (PALS: 0.02 mg/kg; minimum dose, 0.1 mg; maximum single dose, 0.5 mg in child, maximum dose for adolescent 3 mg.
d. β-Adrenergic-blocking drugs (atenolol, metoprolol, and propranolol) have established utility (evidence class I) for patients with unstable angina or myocardial infarction. These drugs reduce the rate of recurrent ischemia, nonfatal reinfarction, and postinfarction VF. In contrast to calcium channel blockers, β-blockers are not direct negative inotropes. β-Blockers are useful for the acute treatment of PSVT, AF, atrial flutter (evidence class I), and ectopic atrial tachycardia (evidence class IIb). Initial and subsequent IV doses, if tolerated, are atenolol, 5 mg over 5 minutes, repeated once at 10 minutes; metoprolol, three doses of 5 mg every 5 minutes; propranolol, 0.1 mg/kg divided into three doses given every 2 to 3 minutes; esmolol, 0.5 mg/kg over 1 minute followed by an infusion starting at 50 µg/min and titrated as needed up to 200 µg/min. Contraindications include second- or third-degree heart block, hypotension, and severe congestive heart failure. Although β-blockers may trigger
bronchospasm in a small number of patients, they are tolerated by most patients with chronic lung disease.
bronchospasm in a small number of patients, they are tolerated by most patients with chronic lung disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree