Chapter 52 Adrenal Insufficiency in the Intensive Care Unit
2 Describe the main types of adrenal insufficiency seen in patients in the ICU
 Relative adrenal insufficiency: This is the most common and perplexing type of adrenal insufficiency seen in patients in the ICU. Patients with relative adrenal insufficiency may present with vasopressor dependency, acute multiple organ dysfunction, hypothermia, or an inability to wean from mechanical ventilation. These patients can be identified by their limited response to adrenal stimulation tests or lower-than-expected basal cortisol levels despite critical illness.
Relative adrenal insufficiency: This is the most common and perplexing type of adrenal insufficiency seen in patients in the ICU. Patients with relative adrenal insufficiency may present with vasopressor dependency, acute multiple organ dysfunction, hypothermia, or an inability to wean from mechanical ventilation. These patients can be identified by their limited response to adrenal stimulation tests or lower-than-expected basal cortisol levels despite critical illness.
 Acute adrenal crisis or insufficiency: The acute clinical presentation typically includes profound hypotension, fever, and hypovolemia. These patients will have very low cortisol levels (<3 mcg/dL).
Acute adrenal crisis or insufficiency: The acute clinical presentation typically includes profound hypotension, fever, and hypovolemia. These patients will have very low cortisol levels (<3 mcg/dL).
 Primary adrenal insufficiency (Addison disease): The most common causes are autoimmune diseases (70%) and tuberculosis (10%). Rare causes include adrenal hemorrhage, adrenal metastasis, cytomegalovirus, human immunodeficiency virus (HIV) disease, amyloidosis, and sarcoidosis.
Primary adrenal insufficiency (Addison disease): The most common causes are autoimmune diseases (70%) and tuberculosis (10%). Rare causes include adrenal hemorrhage, adrenal metastasis, cytomegalovirus, human immunodeficiency virus (HIV) disease, amyloidosis, and sarcoidosis.5 How is adrenal insufficiency diagnosed?
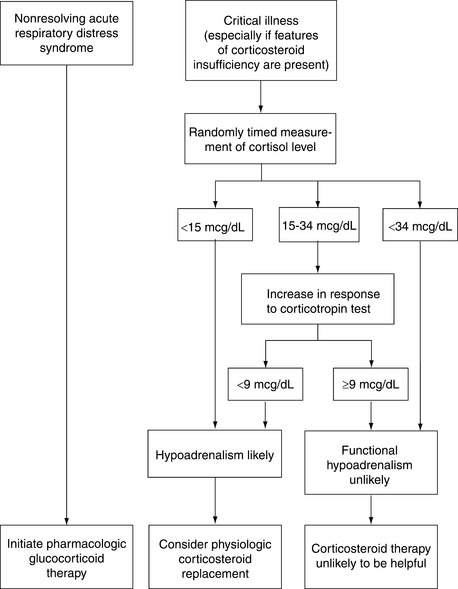
 In ICU patients: The use of provocative adrenal stimulation tests in critically ill patients remains controversial. Perhaps the most widely used protocol (from Annane et al.) identifies patients with septic shock as having relative adrenal insufficiency if their baseline cortisol level is <35 mcg/dL and they respond to an ACTH stimulation test (250 mcg corticotropin) with a bump in cortisol of <10 mcg/dL (see Fig. 52-1). The patients identified as nonresponders appeared to have a reduction in mortality when given stress-dose steroids. However, in a large subsequent study, no mortality benefit with stress-dose steroids was observed for patients with or without evidence of relative adrenal insufficiency.
In ICU patients: The use of provocative adrenal stimulation tests in critically ill patients remains controversial. Perhaps the most widely used protocol (from Annane et al.) identifies patients with septic shock as having relative adrenal insufficiency if their baseline cortisol level is <35 mcg/dL and they respond to an ACTH stimulation test (250 mcg corticotropin) with a bump in cortisol of <10 mcg/dL (see Fig. 52-1). The patients identified as nonresponders appeared to have a reduction in mortality when given stress-dose steroids. However, in a large subsequent study, no mortality benefit with stress-dose steroids was observed for patients with or without evidence of relative adrenal insufficiency.
 In non-ICU patients: In a nonstressed patient, a random cortisol level >20 mcg/dL may rule out the diagnosis of adrenal insufficiency. A random cortisol level <3 mcg/dL confirms the diagnosis of adrenal insufficiency.
In non-ICU patients: In a nonstressed patient, a random cortisol level >20 mcg/dL may rule out the diagnosis of adrenal insufficiency. A random cortisol level <3 mcg/dL confirms the diagnosis of adrenal insufficiency.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree