Acute Pharmacotherapy of Tension-Type Headaches
Ninan T. Mathew
Messoud Ashina
This chapter discusses the treatment of individual attacks of headache in patients with episodic and chronic tension-type headache. Most headache episodes in these patients are mild to moderate. Patients with mild tension-type headache rarely consult the physician and can self-manage by using simple analgesics. These patients may consult a physician when the frequency, severity, and duration of the headache increase. Often, such worsening of headache is associated with stress, anxiety, and depression and may be accompanied by pericranial muscle tenderness and spasm. These factors operate in a vicious cycle, and the physician’s task is to break this cycle.
METHODOLOGIC CONSIDERATIONS IN CLINICAL STUDIES IN THE ACUTE TREATMENT OF TENSION-TYPE HEADACHE
Several parameters, including visual analog scales (VAS), verbal rating scales (VRS), and global ratings, have been studied to assess the pain relief effected by analgesics (11,22,25,51,52). Global rating was reported to be a sensitive parameter, and this finding was confirmed (10,28). Global rating takes into account overall patient acceptability, including taste, ease of use, side effects, and similar factors, in addition to assessing pain relief. Patient’s preference after the intake of two or more different drugs has been a less satisfactory method, because the results depend on the patient’s memory of the degree of effectiveness of a previous medication as well as personal biases about taste and color (23). A strong correlation was found between visual analog pain scales, a verbal pain scale, and verbal pain relief scale (30). A combination of scales that includes global rating gives more reliable assessment of pain relief.
Guidelines for trials of drug treatments for tension-type headache published by the International Headache Society (IHS) Committee on clinical trials (24) recommend VRS or VAS combined with a simple verbal scale for global evaluation efficacy measures.
Patient compliance may become a problem in studies using simple analgesics for the treatment in tension-type headache for the following reasons: (a) Most tension-type headaches are mild and patients therefore may not consider it worthwhile to spend the necessary time and effort for the study. (b) Most patients would have already taken analgesics such as aspirin and may not have confidence in test medications that are not known to be far superior to aspirin. (c) Patients chosen from headache clinics and specialty treatment centers may be more resistant to simple analgesics. Population-based studies are recommended for tension-type headache.
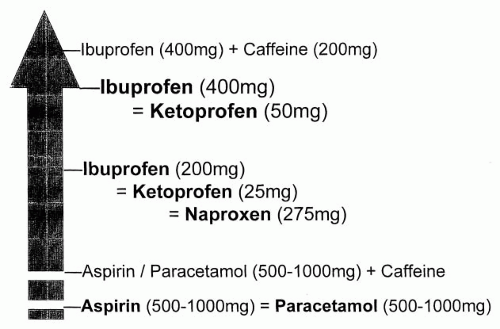
Many controlled studies of simple analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) have been performed in tension-type headache, using the headache attack as a model for acute pain. Several studies done in recent years fulfill the standards recommended for drug trials in tension-type headache by the IHS (24). From these studies, one may conclude that NSAIDs are the drugs of first choice. The following is a review of some of the previous studies and recent randomized, controlled trials comparing various NSAIDs and simple analgesics. Although differences between drugs may be small or variable, a hierarchical classification of compounds emerges when efficacy data are considered (Fig. 83-1).
SIMPLE ANALGESICS
Aspirin and Acetaminophen
Aspirin and acetaminophen are the analgesics used most commonly in the treatment of acute episodes of tension-type headache. In an early double-blind, placebo-controlled, crossover trial, aspirin at doses of 1,000 mg,
500 mg, and 250 mg was shown to be more effective than placebo in the treatment of nonmigrainous headache (50). Moreover, a significant dose-response relationship was established for aspirin; 1,000 mg of aspirin was superior to 500 mg and 500 mg was superior to 250 mg.
500 mg, and 250 mg was shown to be more effective than placebo in the treatment of nonmigrainous headache (50). Moreover, a significant dose-response relationship was established for aspirin; 1,000 mg of aspirin was superior to 500 mg and 500 mg was superior to 250 mg.
Several comparative, randomized, placebo-controlled trials have shown that aspirin (13,28,31,38,40) and acetaminophen (12,35,40,42,48) are effective in the acute therapy of tension-type headache. One of the first placebo-controlled trials demonstrated that 648 mg of solid aspirin and 648 mg of effervescent aspirin were more effective than placebo; there was no difference between solid and effervescent aspirin (28). In another randomized, parallel, double-blind study, a subgroup consisting of 107 patients with tension headaches was treated with 1,000 mg of acetaminophen, 650 mg of aspirin, and placebo (40). Both drugs were more effective than placebo, but no difference was found between the drugs. Steiner et al. (48) reported that two different doses of aspirin (500 and 1,000 mg) and 1,000 mg of acetaminophen were more effective in treating 638 patients with episodic tension-type headache than placebo. In randomized, controlled study of 703 patients, the effects of 1,000 mg of acetaminophen were not significantly different from placebo in a 4-hour sum pain relief intensity differences scores (35). The authors suggested that the spontaneous resolution of headaches could last less than the duration of the evaluation period.
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
Ibuprofen
In one double-blind, randomized, placebo-controlled trial that included 70 patients with muscle contraction headache (published before the IHS Classification), the administration of 400 mg of ibuprofen was shown to be more effective than placebo 30 minutes after administration (44). There are several comparative randomized, placebo-controlled trials regarding the efficacy of NSAIDs in episodic tension-type headache (12, 13, 14,21,35,37, 38, 39,41, 42, 43,49).
In a comparative randomized, controlled trial, it was demonstrated that 153 patients who were administered 400 mg of ibuprofen had better pain relief than 151 patients who received 1,000 mg of acetaminophen or 151 patients administered placebo (43). Moreover, patients who were administered ibuprofen achieved relief faster than those who were administered acetaminophen. Nebe et al. (38) studied the effects of 200 mg of ibuprofen and 500 mg of aspirin in 65 patients with episode tension-type headache in a double-blind, threefold, crossover, placebo-controlled study. The study showed that ibuprofen was significantly superior to aspirin and placebo in decreasing headache intensity on a VAS by a minimum of 50% 1 hour after treatment.
Soluble Ibuprofen
In a double-blind, parallel group, randomized trial that included 154 patients, a new solubilized formulation of 400 mg of ibuprofen was reported to be more effective than 1,000 mg of acetaminophen and placebo in the treatment of episodic tension-type headache (39). Pain relief was reported 39 minutes after administration of the solubilized formulation of ibuprofen, which was significantly faster than with acetaminophen (47 minutes) and placebo (113 minutes) (39).
Ketoprofen
Steiner and Lange (47) evaluated the efficacy of ketoprofen in a multicenter, randomized, parallel group, placebo-controlled study; 25 mg of ketoprofen and 100 mg of acetaminophen were equally effective in pain relief and superior to placebo. In a double-blind, randomized, parallel group study with 159 patients, ketoprofen (25 and 50 mg) was reported to be more effective than 200 mg of ibuprofen and placebo in the treatment of episodic tension-type headache (49). Mehlisch et al. (35) conducted a double-blind, parallel-group, randomized study of 703 patients with episodic tension-type headache and demonstrated that low doses of ketoprofen (12.5 and 25 mg) also were more effective than placebo.
Naproxen Sodium
Naproxen sodium is the sodium salt of naproxen, a phenylalkanoic acid with potent analgesic, anti-inflammatory, and antipyretic properties. Naproxen sodium is more rapidly absorbed and has a more rapid onset of pain relief than naproxen. Rapid absorption and peak plasma levels within 1 hour are desirable qualities for fast relief of headache.
In a multicenter, randomized, double-blind, three-way parallel study that included 124 patients, naproxen sodium (550 mg) was more effective than acetaminophen (650 mg), and placebo (37).
In another multicenter, double-blind, randomized, placebo-controlled trial, 375 mg of naproxen (321 patients) was reported to be more effective than placebo (321 patients), but no better than 1,000 mg of acetaminophen (41).