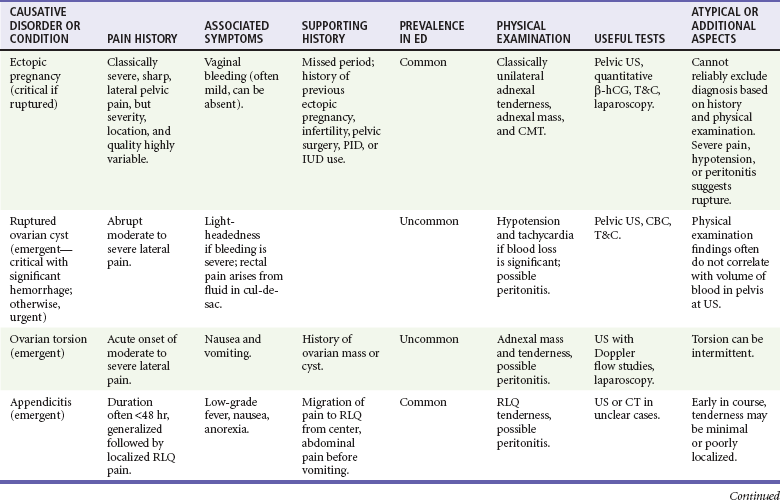
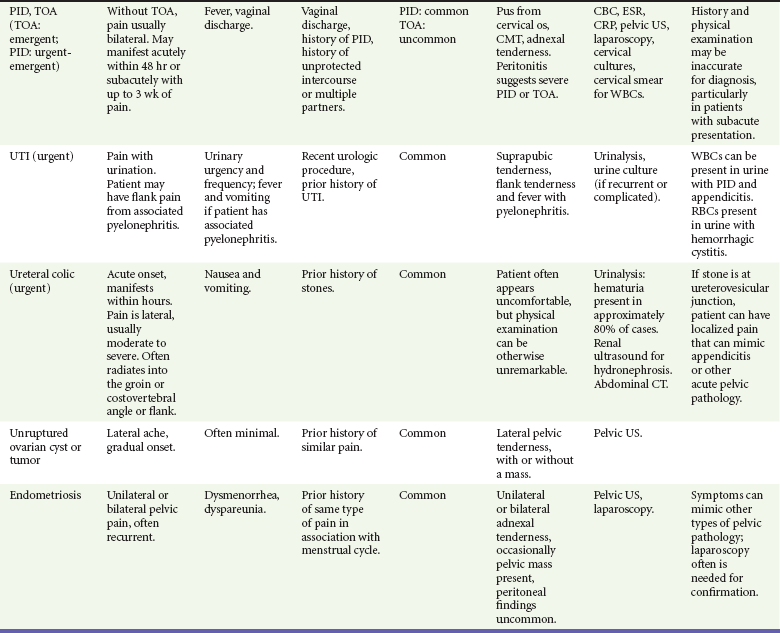
Chapter 33 Over one third of reproductive-age women will experience nonmenstrual pelvic pain. Among diagnoses for women with pain caused by gynecologic disorders in the emergency department, pelvic inflammatory disease (PID) and lower genital tract infections (e.g., cervicitis, candidiasis, Bartholin’s abscess) account for almost half. Other common diagnoses are menstrual disorders, noninflammatory ovarian and tubal pathology (including cysts and torsion), and ectopic pregnancy. In the general population, ectopic pregnancy accounts for 2% of first-trimester pregnancies; however, among women visiting the emergency department with vaginal bleeding or abdominal pain in the first trimester of pregnancy, the incidence of ectopic pregnancy is as high as 18%.1 Younger patients and those with multiple sexual partners are more likely to have PID, and a previous episode increases the likelihood of a subsequent episode.2 The risk of ectopic pregnancy is higher in women who have had PID, pelvic surgery, or a prior ectopic pregnancy, as well as in women with an intrauterine device. Heterotopic pregnancy is of special concern in women undergoing fertility treatment. The incidence of heterotopic pregnancy in the general population was 1 in 30,000 patients in 1948 and is currently reported to be as high as 1 in 8000. It is much more common in women undergoing assisted reproductive techniques (in vitro fertilization and ovulation-stimulating medications), with an incidence of 1 in 100.3 Common nongynecologic diseases, such as appendicitis, diverticulitis, urinary tract infection, and urolithiasis, remain important considerations in the woman with acute pelvic pain. Box 33-1 lists conditions accounting for pelvic pain in most women. Some causes of pelvic pain may lead to serious sequelae. PID carries the short-term risk of tubo-ovarian abscess and the long-term risks of impaired fertility, chronic pelvic pain, and increased predisposition to ectopic pregnancy.5 Rupture of an ectopic pregnancy or a hemorrhagic ovarian cyst may be life-threatening. Unrecognized abuse may have serious or lethal consequences as well. The differential diagnosis of pelvic pain is broad (see Box 33-1). Most causes of pelvic pain fit into three categories: (1) the reproductive tract, (2) the urinary tract, and (3) the intestinal tract. Because a subset of pelvic pain is found only in pregnancy, the pregnancy test is a key branch point in the diagnostic process. Potential pregnancy-related disorders can be divided into complications of early pregnancy and complications that occur further along in pregnancy. Although the specific cause of pelvic pain cannot always be determined at the initial ED visit, an organized approach usually leads to the confirmation or exclusion of disorders most likely to result in significant morbidity and/or mortality. It is rare that any particular finding on history or physical examination (summarized in Table 33-1) is reliable enough to conclusively make or exclude a particular diagnosis, so ancillary testing (beyond a simple pregnancy test) is commonly required in the evaluation of patients with acute pelvic pain.
Acute Pelvic Pain in Women
Perspective
Epidemiology
Diagnostic Approach
Pivotal Findings
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Acute Pelvic Pain in Women
Only gold members can continue reading. Log In or Register to continue