Chapter 47 Acute Pancreatitis
9 How do you determine the severity and prognosis of AP?
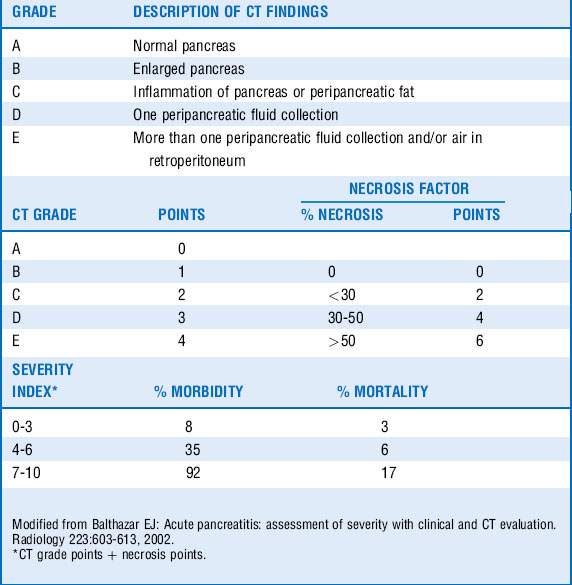
Ranson criteria (Table 47-1) were one of the earliest and widely used scoring systems. Their major disadvantage was that they required 48 hours to complete. The Acute Physiology and Chronic Health Evaluation (APACHE) II system, developed to evaluate critically ill patients, has also been used to differentiate mild AP from SAP. The major disadvantage of this system is that many find it cumbersome as it requires 12 physiologic measures to calculate. A CT severity index (Balthazar score, Table 47-2), has been developed and often used to predict severity of pancreatitis on the basis of radiographic features. The bedside index of severity in AP (BISAP) score (Table 47-3) integrates the systemic inflammatory response syndrome (SIRS) criteria and can be calculated relatively quickly on admission.
Table 47-1 Ranson Prognostic Signs
| Etiology of pancreatitis | ||
|---|---|---|
| Nongallstone | Gallstone | |
| At initial presentation | ||
| Age (yr) | > 55 | > 70 |
| White blood cell count (k/mm3) | >16 | >18 |
| Glucose (mg/dL) | > 200 | > 220 |
| Lactate dehydrogenase (U/L) | > 350 | >400 |
| Aspartate (AST) (U/L) | > 250 | >250 |
| During first 48 hours | ||
| Decrease in hematocrit (%) | ≥10 | >10 |
| Elevation in blood urea nitrogen (mg/dL) | >5 | >2 |
| Serum total calcium (mg/dL) | <8 | < 8 |
| Partial pressure of oxygen (mm Hg) | < 60 | NA |
| Base deficit (mmol/L) | >4 | > 5 |
| Fluid sequestration (L) | > 6 | > 4 |
| Prognosis | No. of Criteria Met | Predicted Mortality |
|---|---|---|
| ≤2 | 0.9% | |
| 3-4 | 16% | |
| 5-6 | 40% | |
| 7-8 | 100% |
NA, Not applicable.
Modified from Ranson JH, Rifkind KM, Roses DF, et al: Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet 139:69-81, 1974; and Ranson JH: Etiological and prognostic factors in human acute pancreatitis: a review. Am J Gastroenterol 77:633-638, 1982.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree