Acute Nephrology
Robert A. Weiss MD
INTRODUCTION
Disorders of the urinary tract are common in pediatric practice. This chapter reviews the most common conditions that are likely to be encountered by the practitioner. Their mode of presentation, diagnosis, differential diagnosis, pathophysiology, and treatment are discussed, emphasizing office approach. Indications for referral to a specialist are also covered.
Urinary Tract Infection
Second only to respiratory tract infection in frequency, urinary tract infection (UTI) occurs in approximately 0.5% to 1% of all boys and 3% to 5% of all girls during the pediatric years (Winberg, Andersen, Bergorrom, et al., 1974). In the newborn period extending into infancy, the male-female ratio is 1:1 (Ginsburg & McCracken, 1982). The uncircumcised state is a risk factor for UTI in male infants (Wiswell & Hachey, 1993); UTI in boys after infancy, however, is rare. The peak age for UTI in girls is around the time of toilet training (Winberg, et al.). It is distinctly uncommon in girls older than 8-years-old (Winberg, et al.). These epidemiological features may, in part, be explained by the differences in pathogenesis of UTI between boys and girls.
ANATOMY, PHYSIOLOGY AND PATHOPHYSIOLOGY
UTI occurs when bacteria, usually of bowel origin (approximately 80% Escherichia coli) (Jodal, 1987), colonize the periurethral area. Bacteria that are characterized by hair-like structures on the cell wall (p-fimbriae or pili), allowing them to adhere to the urinary tract epithelium, are most likely to be pathogenic. Another reservoir of bacteria is the prepuce beneath the uncircumcised foreskin in infant boys. After the urethra is colonized, bacteria replicate in bladder urine. If the infection is confined to the bladder, the symptoms are usually those of bladder irritation: frequency, urgency, dysuria, and wetting in children who are already toilet-trained.
Bacterial infection may ascend to the kidneys in one of two ways. Normally, each ureter enters the bladder in a way that prevents regurgitation of bladder urine into the ureter and, by extension, the kidney itself.
• Clinical Pearl
In approximately one third of all children with UTI (Smellie, Normand, Katz, et al., 1981), this ureterovesical junction valve is incompetent, creating a condition called vesicoureteral reflux (VUR).
The second potential mechanism that can allow infected bladder urine to ascend to the kidney is the elaboration of a toxin by the infecting bacteria that prevents the normal peristaltic action of the ureter, thus allowing bladder bacteria to ascend the ureter to the kidney. In addition, any mechanical obstruction to the drainage of urine, such as hydronephrosis, will allow bacterial access and replication, producing UTI.
HISTORY AND PHYSICAL EXAM
• Clinical Pearl
The clinical features of UTI are nonspecific during infancy and in preschool-aged children. Fever and irritability, without obvious origin in the respiratory tract, is the most common mode of presentation.
Often, gastrointestinal symptoms such as vomiting, diarrhea, and abdominal pain are present. The urine is often foul-smelling or cloudy. The child who had been successfully toilet trained may have wetting accidents. In the school-aged child, the signs and symptoms are more directed to the urinary tract. There may be symptoms of bladder irritation (frequency, dysuria) with cystitis. If the kidney(s) is involved, there is usually significant fever, and the diagnosis of acute pyelonephritis is used. Currently, the 99mTc-DMSA scintiscan is the best tool available to accurately diagnose acute pyelonephritis. In one study, 75% of children had unilateral pyelonephritis; 25%, bilateral lesions (Bjorgvinsson, Majd, Eggli, et al., 1991).
DIAGNOSTIC CRITERIA AND STUDIES
Because the diagnosis of UTI, particularly in infants, commits the clinician to a diagnostic evaluation to determine potentially correctable risk factors, the importance of an accurate diagnosis cannot be underestimated.
The diagnosis of UTI is based on significant bacterial growth in a properly collected urine specimen. The traditional significant colony count is greater than 100,000 colonies/mL.
The presence or absence of white blood cells (pyuria) in the urinalysis (UA) is too unreliable for making or discarding the diagnosis of UTI.
Children who are able to void on command can provide a midstream clean catch urine sample. When compared with the gold standard of a catheterized or bladder puncture specimen, the midstream clean catch is only 80% reliable (Ogra & Faden, 1985). That is, 20% of the time, contamination is the reason for a positive midstream clean catch culture result.
In infants, the results of a urine culture from a specimen obtained by a plastic bag applied to the perineum is helpful only when negative. If the diagnosis of UTI is entertained in an infant, the urine specimen should be obtained by catheterizing the bladder per urethra or by directly aspirating urine from the distended bladder (suprapubic puncture).
• Clinical Pearl
Virtually any bacterial growth is significant when a urine specimen is obtained by suprapubic tap. Intermediate growth (<100,000 colonies/mL) from a catheterized specimen may be significant.
Occasionally, specific clinical scenarios may cloud the diagnosis. The child with symptoms of urgency and frequency is an example. In this scenario, a negative culture in the face of a very dilute urine may actually be a false-negative result. This should prompt a repeated culture obtained from a first morning specimen, which is more likely to be concentrated and thus yield a higher colony count. Additionally, dysuria in the face of a true negative culture may be caused by bubble baths or other bath additives, representing a chemical urethritis.
MANAGEMENT
Acute Antibiotic Treatment
After the results of urine culture are known, or while pending, acute treatment for the less toxic, older child is usually amoxicillin, 40 mg/kg per day, divided into three doses daily, for 10 days. An alternative is a trimethoprim-sulfamethoxazole preparation: 8 mg/kg per day of the trimethoprim moiety, divided into two daily doses. Hospitalization for intravenous treatment is indicated for the infant and/or toxic-appearing patient. Ceftriaxone, 75 mg/kg parenterally every 24 hours at least until the child is afebrile, is a first-line drug, with other cephalosporins available as acceptable alternatives, depending on antibiotic sensitivities. The urine will usually become sterile within 48 to 72 hours, accompanied by a clinical response, including resumption of a healthy demeanor. The remainder of the 10-day antibiotic course may be completed with amoxicillin or an oral cephalosporin, such as cefixime, 8mg/kg per day, divided into two daily doses.
Evaluation for Risk Factors
After acute treatment of the infection, the diagnostic evaluation for risk factors must begin. The purpose of imaging studies is to identify those patients at risk for recurrence of UTI, with its attendant acute morbidity and risk of pyelonephritic scarring (American Academy of Pediatrics [AAP], 1999). While the yield of ultrasonography of the kidneys and bladder is approximately 40% (AAP, 1999), it presents no risk to the patient. Kidney size, number, and position can be determined, as well as dilatation of the pelvis and calyces (hydronephrosis) or ureter (hydroureteronephrosis). The bladder can be evaluated for wall-thickness and for postvoid residual. Ultrasonography is an excellent screen for abnormal urinary tract anatomy, but it provides no functional information.
• Clinical Pearl
The frequency of VUR is such that any infant or child with a febrile UTI merits investigation for this condition with a voiding cystourethrogram (VCUG).
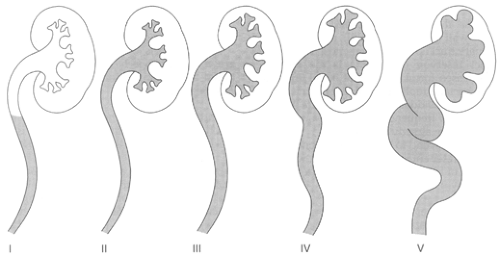
VCUG should be performed as soon as the urine is sterile. The bladder is catheterized with an 8F feeding tube, and radiographic contrast fills the bladder by gravity. Under fluoroscopic control, the radiologist determines if the contrast enters one or both ureters and goes up into the kidney. Figure 39-1 illustrates the clinical grading of VUR as seen on VCUG. Because the likelihood of detecting VUR declines precipitously after age 5 years; those girls older than 5 with a first episode of cystitis who respond promptly to antibiotic treatment need not undergo VCUG. The yield from ultrasonography is so low as to make this examination also unnecessary. However, below the age of 5, many authorities recommend both sonography and a VCUG with the first UTI in respect of the presence or the absence of fever.
Management of Vesicoureteral Reflux
VUR can be unilateral or bilateral, mild, moderate, or severe. When severe, it is frequently associated with kidney scarring from one or more episodes of acute pyelonephritis. Scarring is best seen by the use of a radionuclide renal scan using 99mTc-DMSA.
VUR, when mild or moderate, will often disappear over several years. The patient can be successfully protected against UTI with antibiotic prophylaxis during this period. The preferred agent is trimethoprim-sulfisoxazole, 4 mg/kg per day, administered at bedtime. When VUR is severe, referral to a pediatric urologist is indicated for possible surgical reimplantation of the refluxing ureter(s).
VUR, when mild or moderate, will often disappear over several years. The patient can be successfully protected against UTI with antibiotic prophylaxis during this period. The preferred agent is trimethoprim-sulfisoxazole, 4 mg/kg per day, administered at bedtime. When VUR is severe, referral to a pediatric urologist is indicated for possible surgical reimplantation of the refluxing ureter(s).
Ancillary Management
In addition to imaging studies, a more detailed history of the child’s bladder habits may reveal a pattern of dysfunctional voiding. This condition is often observed in preschool- and school-aged children who void infrequently, often have to rush to the toilet when the urge to void overcomes them, and may wet during the day. Often these symptoms are accompanied by chronic constipation. Such children will frequently benefit from a bladder re-education program of timed voiding and anticonstipation therapy. Occasionally, anticholinergic medication, such as oxybutynin (Ditropan), 5 mg two or three times daily, is helpful.
What to Tell Parents
Regardless of the outcome of the imaging studies, unless antibiotic prophylaxis is prescribed, UTI recurrence rate is at least 50% (Hellerstein, 1982).
Parents should be counseled that after the diagnosis and treatment of a first UTI, monthly surveillance urine cultures are recommended for 3 months, followed by quarterly urine cultures for at least 2 years.
Any febrile illness is an indication to repeat the urine culture (UC) in a child with a past history of even one UTI. Parents must be reminded to report the history of UTI, if they are seeking care for a febrile illness away from the provider’s usual office.
Hematuria
Hematuria must be described as either gross (ie, so many red blood cells [RBCs] that the threshold for visual detection is exceeded) or microscopic (ie, requiring either chemical testing for hemoglobin [dipstick] or microscopy to identify RBCs).
PATHOPHYSIOLOGY
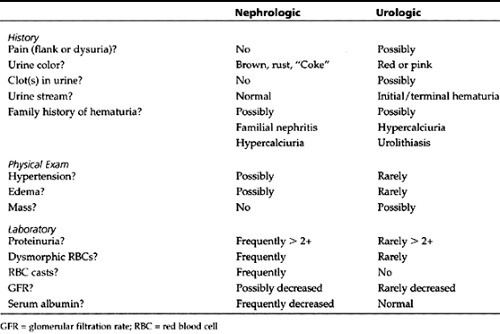
RBCs can originate either from kidney parenchymal disease, such as glomerulonephritis, or from outside the nephron (eg, from the urinary drainage system). The former requires a nephrologic perspective and the latter a urologic perspective. Table 39-1 depicts the clinical and laboratory features that might assist the provider in distinguishing between these two categories.
DIAGNOSTIC CRITERIA AND STUDIES
A visual or microscopic examination of the urine establishes the diagnosis. Not all dark urine is gross hematuria. Two conditions that are not hematuria can be associated with dark urine, reacting with the occult blood pad on the dipstick.
Active hemolysis may release sufficient hemoglobin into the plasma, and thus glomerular filtrate, that the urine is dark, but RBCs are not seen on microscopy. Frequently, bilirubin is found in the urine under such conditions as well.
Massive muscle trauma or disorders of muscle metabolism may release enough myoglobin to darken the urine; again, no RBCs are seen by microscopy.
Neither visual description nor the dipstick alone is sufficient to diagnose gross hematuria; urine microscopy is required.
MANAGEMENT
Gross Hematuria
The child with gross hematuria who is suspected of having a nephrologic process, typically glomerulonephritis, needs evaluation for hypertension, edema, and oliguric renal failure (see section on glomerulonephritis).
The child whom the provider suspects has bleeding from outside the nephron needs an immediate imaging study, typically ultrasonography of the kidneys and bladder, because bleeding may stem from anywhere in the urinary tract.
Microscopic Hematuria
• Clinical Pearl
Screening microhematuria is rarely associated with significant urinary tract pathology (Feld, et al., 1998).
A positive dipstick reaction for “blood” requires confirmation by urine microscopy, because frequently the dipstick reaction is out of proportion to the quantitation of RBCs per high powered field. Should urine microscopy be negative for RBCs, the patient and family can be reassured that no pathology is present, and thus there is no need for follow up surveillance urinalyses.
In the past, children with confirmed microscopic hematuria were subjected to extensive imaging and serologic evaluations, including renal biopsy (Trachtman, et al., 1984). The yield from these diagnostic investigations is so low that they are no longer recommended, except for patients with a history of gross hematuria, significant proteinuria, or a family history of hematuria (gross or microscopic).
What to Tell Parents
For microscopic hematuria, no more than reassurance is usually indicated. Such patients, however, should be instructed to notify their provider if and when gross hematuria occurs, because this event is much more likely to be associated with significant uropathology. For patients with documented microscopic hematuria, regular (at least annual) surveillance UAs should be continued for the purpose of detecting proteinuria, a much more serious marker of glomerular disease. Figure 39-2 depicts an algorithm for the evaluation and management of hematuria in children.
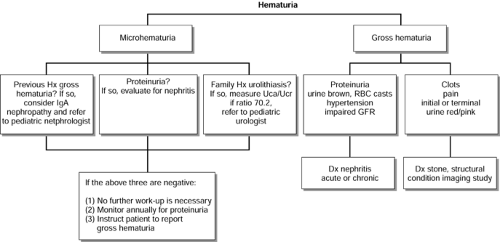 Figure 39-2 Algorithm for the evaluation and management of hematuria.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|