Key Clinical Questions
What risk factors increase the severity of lower gastrointestinal (GI) bleeding?
What are the categories and individual causal factors for colonic ischemia?
What are the indications for tagged red blood cell scan and angiography in the setting of lower GI bleeding?
What are the indications for surgery in patients with diverticular bleeding and ischemic colitis?
Introduction
Lower gastrointestinal (GI) bleeding is defined as bleeding that occurs from a source distal to the ligament of Treitz. This chapter will discuss only colonic sources of bleeding, as other chapters explore both upper gastrointestinal and small intestinal bleeding.
Lower GI bleeding accounts for about 20% of major gastrointestinal bleeding and is less common and generally less severe than upper GI bleeding. There are 20 to 27 hospitalizations per 100,000 adults in the United States due to lower GI bleeding. It generally occurs in the older population with a mean age between 63 and 77 years old. Nearly 80% of lower GI bleeding stops spontaneously, similar to upper GI bleeding. The overall mortality rate of lower GI bleeding is 2% to 4%. Similar to upper GI bleeding, patients who begin lower GI bleeding as an outpatient have a significantly lower mortality rate (3.6%) than inpatients who develop lower GI bleeding (23%).
|
Hematochezia is defined as bright red blood per rectum and usually implies a left colonic source, although it can be caused by a more brisk, proximal source of bleeding. Maroon stools are maroon-colored blood mixed with stool that is often associated with a right colonic source of bleeding; however, it can also result from a more brisk, proximal source of bleeding. Melena refers to black, tarry, foul smelling stool that results from the bacterial degradation of hemoglobin over a period of at least 14 hours. It usually implies an upper GI source of bleeding, although it may be associated with right colonic bleeding in cases of slow motility. Ingestion of iron, bismuth, charcoal, and licorice should be excluded as they all can turn stool black. Occult blood refers to the presence of small quantities of blood in the stool that does not change its color and can only be detected by performing a stool guaiac card test. Blood loss of at least 5–10 mL per day can be detected by stool guaiac card tests. The gastrointestinal tract normally loses about 0.5–1.5 mL of blood per day, which is not usually detected by guaiac tests.
|
History in these patients should focus on factors associated with potential etiologies (Table 160-1). Differential diagnosis should be developed based on presenting complaints and physical examination. Patients should be asked about symptoms that might indicate hemodynamic compromise including dyspnea, chest pain, lightheadedness, and fatigue.
| Etiology of Lower GI Bleeding | Historical Features |
|---|---|
| Hemorrhoidal bleeding |
|
| Proximal large bowel bleeding |
|
| IBD |
|
| Infectious colitis |
|
| Anal fissure |
|
| Colon cancer |
|
| Ischemic colitis |
|
| Diverticulosis |
|
| AVM | Painless bleeding |
| Radiation proctitis | Painless bleeding |
| Colon ulcer | NSAID use |
| Postpolypectomy bleed | Recent colonoscopy |
The physical examination and initial testing should focus on
Vital signs. Orthostatic hypotension with decrease of 20 mm Hg in the systolic blood pressure implies at least a 20% loss of blood volume.
Abdominal examination for tenderness, masses, liver span, and splenomegaly.
Rectal examination including inspection of the anus, characterization of the stool color, and stool guaiac card test.
Triage/Hospital Admission
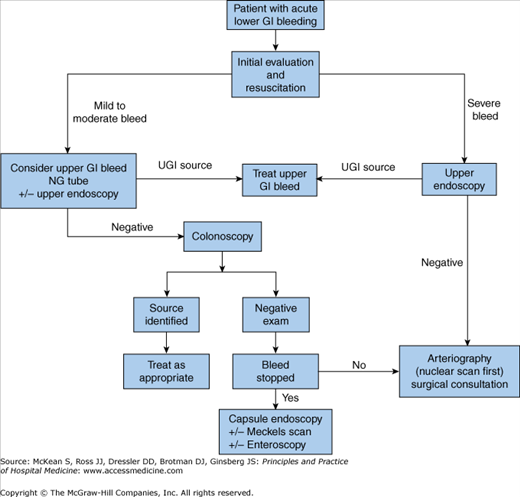
When patients initially present with acute lower GI bleeding, they should be triaged and managed based on the severity of the hemorrhage (Figure 160-1).
During the initial clinical evaluation of patients with suspected acute lower GI bleeding, resuscitation should proceed simultaneously with the placement of two large-bore (18-gauge or larger) peripheral catheters or a large bore central line (eg, cordis) followed by administration of intravenous fluids including normal saline and/or packed red blood cells. Blood tests should be performed including complete blood count, prothrombin time, partial thromboplastin time, electrolytes, and typing and cross-matching for blood products. Coagulopathy and thrombocytopenia should be immediately corrected if possible. Platelets should be maintained above 50,000/mL and coagulopathy should be corrected with vitamin K or fresh frozen plasma. Vitamin K should be taken orally unless the patient has cirrhosis or biliary obstruction, in which case it should be administered subcutaneously. It takes 12 to 24 hours for the full effect of vitamin K to occur, unlike fresh frozen plasma, which rapidly reverses coagulopathy. The effects of fresh frozen plasma last about three to five hours and large volumes (over 2–3 liters) may be required to completely reverse coagulopathy depending on the initial INR. Recombinant activated factor VII has been approved for use in patients with hemophilia A and B with factor 8 and 9 inhibitors. Evidence of possible benefit in patients with cirrhosis and gastrointestinal bleeding has been demonstrated, although the optimal dose is unclear and recombinant activated factor VII is very expensive with a single 90 mcg/kg dose costing at least $4500.
Multiple validated scoring systems help predict the probability of rebleeding, surgery, and mortality in upper GI bleeding. These scoring systems enable appropriate triage and aggressive management of high risk patients and potentially early discharge of low risk patients. Few studies stratify patients by severity in lower GI bleeding. The strongest predictors of mortality include age over 70, ischemic colitis, and presence of at least two comorbidities.
Risk factors identified for increased severity of lower GI bleeding are heart rate greater than 100 beats per minute, systolic blood pressure less than 115 mm Hg, syncope, nontender abdomen, rectal bleeding within four hours of presentation, aspirin use, and more than two comorbidities. Patients with none of these risk factors have a low risk (6%) of severe bleeding; those with one to three of these have a moderate risk (43%); and those with more than three risk factors have a high risk (79%) of severe bleeding.
Increased severity of lower GI bleeding is associated with the following risk factors (RF):
Zero RFs equates to a low incidence (6%) of severe bleeding. One to three RFs equates to a moderate incidence (43%) of severe bleeding. More than three risk factors equates to a high risk (79%) of severe bleeding. |
Patients who have minor bleeding with scant hematochezia represent 75% to 90% of all patients with lower GI bleeding and may be evaluated as outpatients. For patients over the age of 50 years, colonoscopy should be performed to evaluate the source and to screen for colon cancer. In younger patients with rectal bleeding, there is debate regarding the necessity of a colonoscopy versus flexible sigmoidoscopy. Several studies demonstrate that 10% to 30% of patients with rectal bleeding had proximal lesions, which would have been missed by a flexible sigmoidoscopy. Other studies found that no cancers and only a very few polyps would have been missed by flexible sigmoidoscopy in patients with “outlet-type bleeding,” defined as blood seen during or after defecation on the toilet paper or in the toilet bowl without symptoms or special risk factors for colorectal neoplasia. Physicians are unable to reliably predict based on history alone which patients with rectal bleeding will have significant pathology. As patients grow older, it becomes cost-effective to perform a full colonoscopy. Patients in their mid-30s or older should likely be evaluated with a colonoscopy while patients in their 20s with “outlet-type bleeding” may have a flexible sigmoidoscopy. If no lesion is discovered to explain the hematochezia, those patients should then undergo a full colonoscopy.
Another category of patients presents with chronic, intermittent bleeding, which manifests as guaiac positive stool and/or iron deficiency anemia. Evaluation of these patients can usually occur in the outpatient setting; however, if the patients are severely anemic with cardiopulmonary symptoms and/or disease, inpatient admission should be considered for further monitoring, evaluation, and management. All of these patients must be evaluated with colonoscopy. About 25% to 41% of these patients will have abnormalities on upper endoscopy. Therefore, if no source is identified on colonoscopy or if the patient has upper gastrointestinal symptoms, an upper endoscopy should be performed. Asymptomatic patients may also harbor upper gastrointestinal abnormalities, and those with iron deficiency anemia should undergo an upper endoscopy.
Other patients with lower GI bleeding include those with episodic, severe bleeding and continuous active bleeding who must be evaluated in the hospital. Approximately 10% to 15% of initially suspected lower GI bleeding cases ultimately have an upper gastrointestinal source. Clues to the possible upper gastrointestinal source include hematochezia with hemodynamic instability, melena, and a history of upper GI bleeding. Placement of a nasogastric tube or obtaining a prompt upper endoscopy examination may be helpful to rule out an upper GI source in patients with severe bleeding.
|
Diagnosis
Diagnostic evaluation must be performed after patients have been adequately resuscitated. If an upper GI source is suspected, an upper endoscopy should be performed first. Lower GI evaluation can be performed with anoscopy, flexible sigmoidoscopy, colonoscopy, rarely barium enema, and various radiologic studies.
Anoscopy is useful only for diagnosing bleeding sources from the anorectal junction and anal canal including internal hemorrhoids and anal fissures. This is performed using an anoscope, which is a tube about the width of an average to large bowel movement and three to four inches long through which a light can be shone. Anoscopy is superior to flexible sigmoidoscopy for detecting hemorrhoids in an outpatient setting, and can be performed quickly in the office or at the bedside as an adjunct to flexible sigmoidoscopy and colonoscopy.
Flexible sigmoidoscopy uses a 65 cm long sigmoidoscope that visualizes the left colon. It can be performed without sedation and only minimal preparation with enemas. However, the diagnostic yield of flexible sigmoidoscopy in acute lower GI bleeding is only 9%. The role of anoscopy and flexible sigmoidoscopy in inpatients with acute lower GI bleeding is limited as most patients should undergo colonoscopy.
Colonoscopy is the test of choice in the majority of patients with acute lower GI bleeding as it can be both diagnostic and therapeutic. The diagnostic accuracy of colonoscopy in lower GI bleeding ranges from 48% to 90% and urgent colonoscopy appears to increase diagnostic yield. This wide range in yield is partially explained by different criteria for diagnosis, as often if no active bleeding, nonbleeding visible vessel, or adherent clot is found, bleeding is attributed to a lesion if blood is present in the area. The presence of fresh blood in the terminal ileum is presumed to indicate a noncolonic source of bleeding.
The overall complication rate of colonoscopy in acute lower GI bleeding is 1.3% with 0.3% risk of perforation. Bowel preparation is safe and well-tolerated in most patients. The complication rate of colonoscopy in an unprepped colon may be higher. About 2% to 6% of colonoscopy preparations in acute lower GI bleeding are poor. Between 4 to 8 liters (1–2 gallons) of Golytely should be administered orally or via nasogastric tube until the effluence is clear. Antiemetics and prokinetics such as metoclopramide 10 mg should be given as needed during the preparation. In patients at risk of aspiration or fluid overload the preparation should be cautiously administered although complication rates are low with PEG-based preparations. Colonoscopy can be performed within one to two hours after the stool clears. There is no role for enemas in colonoscopy preparation.
It is not clear that aggressive treatment with urgent colonoscopy improves the outcome in patients with severe lower GI bleeding. There are two prospective randomized trials to date of patients with significant lower GI bleeding who were randomized to standard care or urgent colonoscopy. Patients in the standard care arm underwent elective colonoscopy within four days of admission while patients undergoing urgent colonoscopy were administered 4–6 L of a balanced electrolyte-polyethylene glycol (PEG) prep solution orally or via a nasogastric tube over three to four hours and underwent colonoscopy within 8 to 12 hours of hospitalization or diagnosis of hematochezia. More sources of bleeding were identified in the urgent colonoscopy group in one study, but there was no difference in early or late rebleeding, length of hospital stay, surgery, mortality, or complications in either study. Therefore, it is unclear whether urgent colonoscopy influences patient outcome despite the increased identification and treatment of a source of bleeding, and further larger studies are needed.
There is no role for barium enema in acute lower GI bleeding. It may impede the performance of a colonoscopy or subsequent angiography due to the presence of barium in the colon. In young patients with minor hematochezia who have a negative flexible sigmoidoscopy, barium enema can be an alternative to colonoscopy.
Tagged red blood cell scan and angiography may be the tests of choice in patients with massive lower GI bleeding that prevents colonoscopy, in those with ongoing bleeding and a negative colonoscopy, or in patients who have not yet been prepared for a colonoscopy. Although tagged RBC scan is solely a diagnostic exam, angiography, like colonoscopy, can be both diagnostic and therapeutic.
A bleeding rate of at least 0.1 to 0.5 mL/min is required to be detected by tagged RBC scan. An injected radiotracer circulates in the blood and extravasation of blood into the gastrointestinal lumen can be identified on a series of static images captured after injection or on multiple sequential dynamic images obtained at 15- or 30-second intervals (Figures 160-2A, B). Two radiotracers have been used for tagged RBC scan: technetium (Tc) 99 m sulfur colloid and technetium 99m-labelled RBC, which involves labeling the patient’s red blood cells in vitro and then reinjecting them into the patient. Sulfur colloid is rapidly cleared by the reticuloendothelial system and, therefore, leaves the blood pool within minutes, which provides an approximate 10-minute window to detect extravasation. RBC labeling is superior because the red blood cells persist for at least 24 hours in the circulation. This allows for longer imaging and repeated imaging if the patient rebleeds during this time window. Typically a 90-minute imaging period is used as the diagnostic yield plateaus at this time.