Chapter 88 Acute Liver Failure, Liver Transplantation, and Extracorporeal Liver Support
Acute liver failure (ALF) is a relatively rare and potentially fatal disease. It represents a heterogeneous condition with numerous etiologies in which the pathophysiology is diverse and frequently unclear, preventing substantial advances in specific therapy. Recognized etiologies include infections, toxins, metabolic disorders, infiltrative diseases, autoimmune hepatitis, ischemic, or irradiation damage, although a proportion of cases are unable to be diagnosed and fall into the cryptogenic group.1–4 For the pediatric intensivist, the mainstay of therapy consists of meticulous supportive measures, with a focus on anticipation and prevention or treatment of complications and early consideration for liver transplantation.5–10 With the onset of cerebral edema in children with acute liver failure, the risk for permanent disability increases dramatically.11–13 Thus the timely intervention to prevent the metabolic derangements associated with acute liver failure is pivotal in preventing progression and the morbidity associated with this condition.14–16 The rewards of bridging children with end-stage liver failure are reflected in the recent publication of the Pediatric Acute Liver Failure (PALF) Study Group, in which 53% of patients survived with medical therapy alone and an additional 30% survived with the aid of liver transplantation.3
Definition
The clinical syndrome of acute or “fulminant” liver failure is defined as the onset of hepatic encephalopathy and coagulopathy within 8 weeks of the onset of liver disease in the absence of preexisting liver disease in any form.1,17 This narrow definition does not adequately address children with new-onset liver disease who develop encephalopathy more than 8 weeks after presentation or children with subclinical chronic liver disease such as autoimmune hepatitis or Wilson disease who present initially with liver failure. Although the management principles of children are similar for most etiologies of liver failure,15,16 it is important for the intensivist to recognize that the prognosis can be remarkably different for the different underlying causes.
Epidemiology
The cause of ALF in children continues to be age dependent2,3,18 with viral hepatitis probably the most common cause of ALF in all age groups overall. Severe hepatitis from echovirus and adenovirus is seen almost exclusively in the neonatal population. Liver failure can be one of the manifestations of overwhelming herpes infection in the newborn or immunocompromised patient. Metabolic liver disease and familial erythrophagocytosis are most commonly found in infants. Acute hepatitis A and B infections are rare causes of ALF in North America, but are a common cause of ALF in school-aged children in developing countries.19 Drug-induced liver disease is more common in older children especially that secondary to intentional acetaminophen overdose.20 Acute liver failure of indeterminant cause is common in all age groups, accounting for 40% of ALF among patients younger than age 3 years and 60% in those age 3 years and older.20
The incidence of ALF in childhood is not well described but has been estimated to be 2000 cases per year in adults in the United States. A recently established multicenter database (PALF) including 24 pediatric liver centers in the United States, Canada, and England, has collected demographics and outcome data from 348 pediatric cases of acute liver failure over a 6-year period.20 A specific etiology could not be determined in 49% of the cases. Overall survival in this group was 84% at 3 weeks after presentation with 36% of the survivors receiving liver transplantation.3,20 Considering the infrequency of this diagnosis and the frequent associated morbidity and mortality it is not unexpected that few pediatric subspecialists are comfortable managing patients with this diagnosis.
Management
Initial Assessment and Care
There is no specific therapy for acute and end-stage liver failure except hepatic replacement. Management therefore is directed toward early consideration for liver transplantation, hepatic support, treatment of acquired infections, and prevention and treatment of complications while awaiting recovery or a suitable donor for liver transplantation.15,16,22–36 The key elements in managing patients before transplantation are meticulous medical support in the setting of an intensive care unit and rapid referral to a transplant center. It is essential to take a full history from the parents; this would include establishing appropriate risk factors such as information on intravenous injections, infusions of blood products, foreign travel or contact with individual exhibiting jaundice. It is important to establish what medications the child has taken, including over-the-counter preparations, folk remedies and herbal supplements, what medications might be in the household, and in adolescents to inquire about the use of illicit drugs and sexual contact. Folk remedies, some Chinese herbs, and herbal supplements (e.g., pennyroyal) in particular are often overlooked by parents giving a medical history but may be vital information in establishing an etiology.27 Until a diagnosis is made (Box 88-1), it is assumed that all children are infectious and that all blood, excretions and secretions are potentially capable of transmitting viral hepatitis. Enteric isolation procedures must be enforced (http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf) until an infectious etiology has been ruled out.
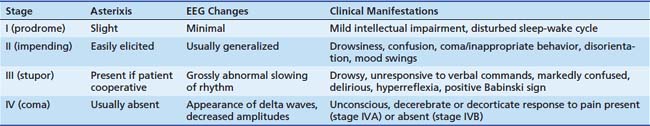
The initial physical examination should determine the status of major organ systems including hepatic, cerebral, cardiovascular, respiratory, renal, and acid–base balance. The patient’s level of consciousness and degree of hepatic encephalopathy (Table 88-1) should be established using a reliable scale3,28,29 and a complete central nervous system examination performed including examination of reflexes and mental status. Progression of coma may be assessed by serial examinations. Evidence of chronic liver disease or other signs which may suggest an etiology, such as Kayser-Fleischer rings, caput succedaneum, cataracts, and needle marks, should be established. Liver size and consistency should be determined and documented. The presence of impaired central nervous system function with acute liver disease is an indication for immediate hospitalization independent of any other clinical or biochemical findings. Observation in a suitable facility to intervene immediately with mechanical ventilation, intracranial pressure monitoring, if deemed beneficial, rapid availability of blood products and the ability to maintain acid-balance/fluid and electrolyte balance is critical. Typically, this level of support warrants referral to a transplant center where greater experience and availability of emergency transplantation may prove lifesaving.
A central venous catheter is useful for assessment of right heart function and volume status, but must be placed with care in patients with significant coagulopathy or thrombocytopenia. Use of a multilumen catheter, which enables simultaneous administration of blood products, dextrose solutions to maintain normal serum glucose levels, intravenous fluids and drugs, is helpful and may be replaced if needed to facilitate exchange blood transfusions or renal replacement therapy when required. An indwelling arterial line for continuous measurement of blood pressure and for biochemical and acid-base monitoring is frequently helpful especially in patients with evolving cardiopulmonary instability or in whom intracranial pressure monitoring is planned.30 A nasogastric tube is passed and placed to gravity, with regular gentle saline lavage to detect upper gastrointestinal hemorrhage. The urinary bladder is catheterized and strict output measured to help in the evaluation of fluid status and renal function. Ideally, the patient is placed on a bed that permits the body weight to be recorded frequently.
Baseline biochemical and other investigations should be performed and management initiated as in Box 88-2. Frequency of biochemical monitoring will depend on the severity of illness, ranging from daily in mild cases to every 4 to 6 hours in patients in stage III and IV coma, and should include complete blood count, blood gases, electrolytes, aminotransferases, and prothrombin time, plus daily monitoring of plasma creatinine, bilirubin, and ammonia. A baseline chest radiograph is useful to diagnose cardiac dysfunction or aspiration. An abdominal ultrasound may indicate liver size and patency of hepatic and portal veins, particularly if liver transplantation is being considered.
Nonspecific Adjunctive Therapy
It is usual to administer a single dose of vitamin K (2 to 10 mg intravenously) although it is frequently not effective. Proton pump inhibitors and antacids (see below) should be administered prophylactically to minimize the risk of gastrointestinal hemorrhage from stress erosions. The role of N-acetylcysteine in the management of ALF other than acetaminophen poisoning has been investigated with promising results. A multicenter, randomized trial of a continuous infusion of N-acetylcysteine over the first 72 hours after presentation in adult patients with ALF suggests that N-acetylcysteine may improve spontaneous survival in patients with early stages of encephalopathy.31,32
Central Nervous System Monitoring
A baseline electroencephalogram may be helpful to stage coma; however, the findings are typically nonspecific. Computed tomography scans may be useful early in encephalopathy as a baseline examination to be compared with subsequent imaging to evaluate for signs of progressive, cerebral edema later in the disease. Frequent evaluation of neurological function with serial examinations and blood ammonia is essential to follow the progress of hepatic encephalopathy. Continuous or frequent electroencephalography may demonstrate abnormal electrical activity as a heralding sign of progressive hepatic encephalopathy or subclinical seizure activity. The role of intracranial pressure monitoring remains controversial (see Cerebral Encephalopathy and Edema sections in the following sections). The choice of intracranial pressure monitoring system is dependent on the standards of the individual institution and neurosurgeon consulting on the case (see also Chapter 59). All forms of intracranial monitoring are potentially hazardous in patients with severe coagulopathy, but they may provide helpful information on changes in intracranial pressure and improve selection for liver transplantation.30
Prevention and Management of Complications
Hypoglycemia
Hypoglycemia (blood glucose <40 mg/L) develops in the majority of children. It may contribute to central nervous system impairment and other organ dysfunction. Factors contributing to hypoglycemia include (1) failure of hepatic glucose synthesis and release, (2) hyperinsulinemia (due to diminished of hepatic degradation), (3) increased glucose utilization (due to anaerobic metabolism), and (4) secondary bacterial infection.33–36
Frequent bedside monitoring of blood glucose concentrations (every 2 to 4 hours) and the intravenous administration of glucose (10% to 50% dextrose) are required to prevent this complication. Patients may typically require 5 to 8 mg/kg/min of dextrose infused to meet these goals; however, clinicians should avoid excessively high rates of glucose infusion and the resulting hyperglycemia. Increased insulin production, secondary to excess glucose infusion, leads to increased glucose need and net lipogenesis that can be avoided by permitting the blood glucose to remain between 40 and 60 mg/L. Profound refractory hypoglycemia carries a grave prognostic implication and often heralds the imminent death of the patient.
Coagulopathy and Hemorrhage
The management of coagulopathy and hemorrhage is a major challenge in the overall care of the child with acute liver failure. Profound disturbances in hemostasis develop secondary to failure of hepatic synthesis of clotting factors and fibrinolytic factors, reduction in platelet numbers and function, and/or intravascular coagulation.37,38 The coagulation factors synthesized by hepatocytes include factors I (fibrinogen), II (prothrombin), V, VII, IX, and X, and a reduction in synthesis leads to the prolongation of prothrombin and partial thromboplastin time
Administration of recombinant factor VIIa (40 μg/kg) reliably corrects the coagulation defect in patients with acute liver failure for a period of 6 to 12 hours and may be useful in preparation for invasive procedures.39 Double-volume exchange transfusion may also temporarily improve coagulation to control life-threatening hemorrhage, especially in patients with DIC. Hemofiltration may be necessary to control fluid balance and provide fluid “space” if large amounts of coagulation support are required. Platelet counts should be maintained above 50 × 103/μL by infusion of platelets. DIC is rarely severe enough to warrant the risks of heparin infusion to break the vicious cycle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree