Key Clinical Questions
Introduction
Acute kidney injury (AKI) is defined as a potentially reversible sudden deterioration in renal function due to prerenal, intrarenal, or postrenal causes. AKI is frequently accompanied by dysregulation of extracellular fluid volume and electrolytes and a marked increase in the retention of nitrogenous and nonnitrogenous waste products over a period of hours to weeks. AKI may be oliguric (< 400 mL/day) or nonoliguric (> 400 mL/day). AKI can also be defined as an acute and sustained increase in serum creatinine of 0.5 mg/dL (44.2 micromol/L), if the baseline is less than 2.5 mg/dL (221 mmol/L), or an increase in serum creatinine more than 20% if the baseline is more than 2.5 mg/dL (221 mmol/L).
There have been several attempts to achieve consensus among intensivists and nephrologists on the definition of AKI. The Acute Dialysis Quality Initiative (ADQI) group published the RIFLE classification of AKI in 2004 based on three severity categories (risk, injury, and failure) and two clinical outcome categories (loss and end-stage renal disease) (Table 246-1). The parameters assessed in the RIFLE classification are changes in serum creatinine level or glomerular filtration rate (GFR) or urine output (UO) from the patient’s baseline. The baseline serum creatinine level and GFR may not be readily available. Hence the consensus committee recommends the use of the Modification of Diet in Renal Disease (MDRD) equation to estimate GFR/1.73 m2. The proportional decrease in GFR is calculated from 75 mL/min per 1.73 m2, the agreed-upon lower limit of normal.
|
A modified RIFLE criteria schema has been proposed by the Acute Kidney Injury Network (AKIN).The AKIN diagnostic criteria (Table 246-2) and the classification/staging system (Table 246-3) for AKI are an abrupt (within 48 hours) reduction in kidney function currently defined as an absolute increase in serum creatinine of more than or equal to 0.3 mg/dL (≥ 26.4 μmol/L), a percentage increase in serum creatinine of more than or equal to 50% (1.5-fold from baseline), or a reduction in urine output (documented oliguria of less than 0.5 mL/kg per hour for more than 6 hours). The absolute increase in the serum creatinine levels (≥ 0.3 mg/dL) in this diagnostic criterion is based on epidemiologic data demonstrating that changes in serum creatinine levels of 0.3 to 0.5 mg/dL are associated with increased mortality risk. Also, the timeline of “within 48 hours” is deliberately included in the diagnostic criteria because of data demonstrating poorer outcomes within this period. The clinical utility and universal adoption of either RIFLE or AKIN criteria remain uncertain, and future studies are needed to demonstrate their validity.
| An abrupt (within 48 hours) reduction in kidney function currently defined as an absolute increase in serum creatinine of more than or equal to 0.3 mg/dL (≥ 26.4 μmol/L), a percentage increase in serum creatinine of more than or equal to 50% (1.5-fold from baseline), or a reduction in urine output (documented oliguria of less than 0.5 mL/kg per hour for more than 6 hours). |
| Stage | Serum Creatinine Criteria | Urine Output Criteria |
|---|---|---|
| 1 | Increase in serum creatinine of more than or equal to 0.3 mg/dL (≥ 26.4 μmol/L) or increase to more than or equal to 150% to 200% (1.5- to 2-fold) from baseline | Less than 0.5 mL/kg per hour for more than 6 hours |
| 2* | Increase in serum creatinine to more than 200% to 300% (> 2- to 3-fold) from baseline | Less than 0.5 mL/kg per hour for more than 12 hours |
| 3† | Increase in serum creatinine to more than 300% (> 3-fold) from baseline (or serum creatinine of more than or equal to 4.0 mg/dL [≥ 354 μmol/L] with an acute increase of at least 0.5 mg/dL [44 μmol/L]) | Less than 0.3 mL/kg per hour for 24 hours or anuria for 12 hours |
Epidemiology
The prevalence of AKI has been reported to be approximately 1% of all hospital admissions in the United States. Major causes of hospital-acquired AKI include volume depletion resulting in decreased renal perfusion, major surgery, septic shock, congestive cardiac failure, contrast nephropathy, and aminoglycoside antibiotics. Acute tubular necrosis (ATN) is identified as the most frequent clinicopathologic entity in hospital-acquired AKI, followed by prerenal azotemia, acute-onset chronic renal failure, and urinary tract obstruction.
AKI occurs in 1 to 25% of the patients admitted in critical care units, with major causes including sepsis, multiorgan failure, hypotension, nephrotoxin administration, and prerenal factors. AKI affects mostly older patients who have chronic morbidities or are severely ill on admission to the hospital. The overall in-hospital mortality rate in intensive care unit (ICU)-associated AKI is approximately 60%.
Community-acquired AKI accounts for 1% of the hospital admissions in the United States. Community-acquired AKI in developed nations mainly affects older patients, with causes including acute tubular necrosis, prerenal azotemia, acute-onset chronic renal failure, and obstructive uropathy. In the developing countries, AKI is predominantly a disease of infants and children and is due to prerenal etiologies, such as dehydration from acute diarrheal illness. Falciparum malaria, HIV/AIDS, obstetrical mishaps, dengue fever, snake bites, insect stings, botanical and chemical nephrotoxins, acute glomerulonephritis, hemolytic uremic syndrome, and alternative medical therapies are important etiological factors of AKI in the tropics. Crush injury from natural disasters such as earthquake contributes to regional epidemics of AKI.
Causes of AKI
The causes of AKI can be classified under three broad categories: prerenal, renal, and postrenal (Table 246-4). Prerenal azotemia and ischemic ATN account for 75% of AKI.
|
Prerenal causes are characterized by a reversible loss of kidney function and a drop in GFR due to decreased renal perfusion, while the integrity of renal structural components is maintained. Prerenal causes account for approximately 70% of community-acquired AKI and 40% of hospital-acquired cases. Prerenal azotemia is typically due to decreased effective circulating volume, true hypovolemia, or impaired renal perfusion.
Decreased effective circulating volume may be due to cardiac failure, aortic stenosis, nephrotic syndrome, cirrhosis, hepatorenal syndrome, acute pancreatitis, cardiac tamponade, sepsis, or systemic vasodilatation in conjunction with sepsis or anesthesia.
Intravascular volume depletion, a possible result of dehydration due to vomiting, diarrhea, poor fluid intake, fever, and diaphoresis, is the most common cause of prerenal azotemia in the outpatient setting. Excessive urination (polyuria) due to excess diuretics, diabetes insipidus, or poorly controlled diabetes mellitus can also cause AKI. Other causes of volume depletion include gastrointestinal bleeding and plasma loss due to burns, trauma, and anaphylaxis.
Decreased renal perfusion may result from renal artery stenosis or renal vein thrombosis, or more often from drugs such as nonsteroidal antiinflammatory drugs (NSAIDs), which interfere with glomerular autoregulation, especially in patients above the age of 60 with additional risk factors for prerenal azotemia, such as atherosclerotic vascular disease, preexisting CKD, hypotension, diuretic use, cirrhosis, nephrotic syndrome, and congestive cardiac failure. Immunosuppressive drugs, such as tacrolimus and cyclosporine, lead to acute kidney injury by inducing vasoconstriction of the afferent and efferent glomerular arterioles of the kidneys. Angiotensin-converting enzyme (ACE) inhibitors may cause AKI in patients with unilateral or bilateral renal artery stenosis.
Intrarenal causes of AKI are characterized by the loss of kidney function due to structural damages to glomeruli, tubules, vessels, or interstitium and are often categorized based on the primary site of renal injury.
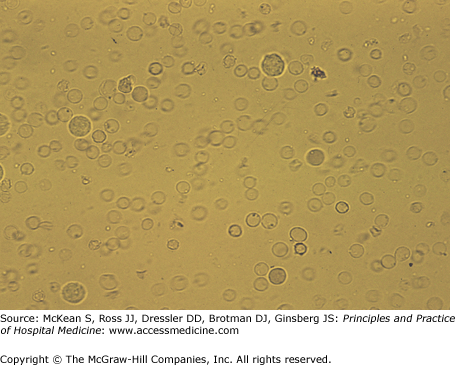
Acute tubular necrosis (ATN) (Figure 246-1), is the most common cause of intrinsic renal failure and is also the most common cause of hospital-acquired acute kidney injury. It usually results from tubular ischemia and inflammation, as in sepsis and shock, or tubular toxins such as heme pigments, for example, myoglobin from rhabdomyolysis or hemoglobin from intravascular hemolysis, cisplatin, ethylene glycol, and myeloma light chains. Ischemic tubular necrosis may occur in patients with sustained prerenal azotemia. Ifosfamide, a chemotherapeutic agent is known to cause acute tubular dysfunction in the proximal tubule.
Hospital-acquired ATN is often multifactorial. For example, it may occur in a septic patient exposed to a potentially nephrotoxic drug, such as an aminoglycoside or amphotericin, or after the administration of a radiocontrast agent in a hypovolemic patient with preexisting renal dysfunction.
Patients with severe renal ischemia may develop cortical necrosis with injury to both tubules and glomeruli. Causes include severe sepsis, dehydration, snake bites, obstetrical catastrophes, thrombotic microangiopathies, and malaria. The prognosis for recovery is less favorable than for ATN.
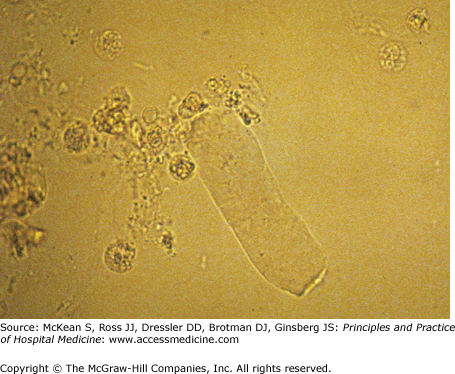
Glomerular disease in the form of rapidly progressive glomerulonephritis (RPGN) and acute proliferative glomerulonephritis may cause AKI (Figure 246-2). RPGN may be primary or secondary in origin, the latter being associated with systemic diseases like systemic lupus erythematosus, Wegener granulomatosus, polyarteritis nodosa, Henoch-Schönlein purpura, and Goodpasture syndrome. RPGN can also progress to end-stage renal disease (ESRD) in days to weeks. Acute proliferative glomerulonephritis occurs in patients with bacterial endocarditis, poststreptococcal infection, and postpneumococcal infection.
Vascular disease (ie, microvascular and macrovascular renal arterial disease) can cause AKI. Thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, HELLP syndrome (hemolytic anemia, elevated liver enzymes, low platelet count), glomerular capillary thrombosis, and atheroembolic disease may all cause AKI. Patients undergoing interventional or invasive procedures involving the major vessels and those with arrhythmias are at an increased risk for AKI from atheroemboli (Figures 246-3, 246-4, and 246-5).