Chapter 7 Acute coronary syndromes
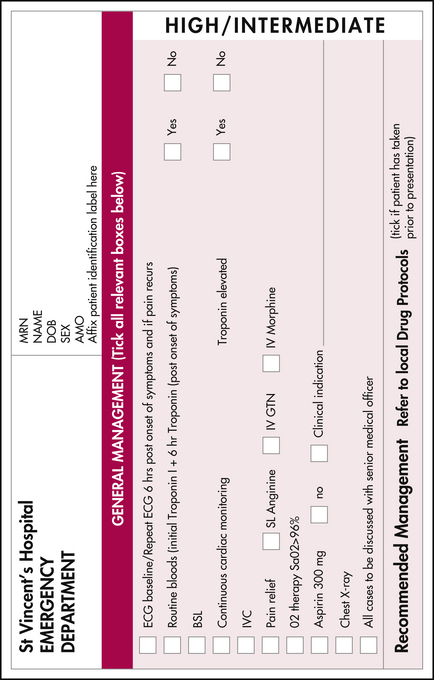
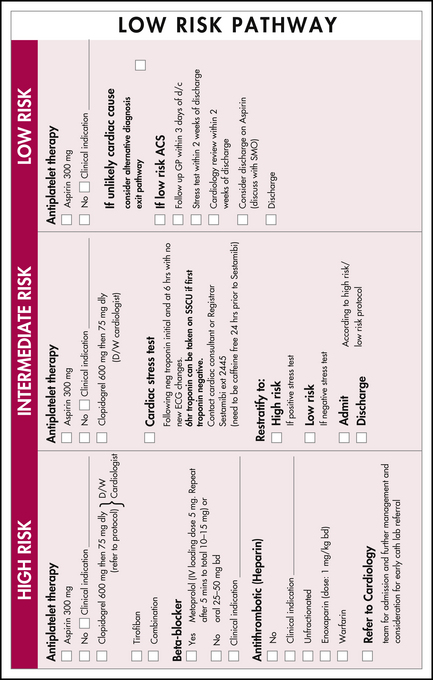
Symptoms and signs which may indicate an acute coronary syndrome (ACS) need to be identified as soon as possible, ideally by the patient, so that treatment can be initiated to avoid or minimise myocardial damage and to avert the risk of life-threatening complications. A defibrillator must be immediately available with staff trained in its use. Assign a high priority at triage to patients with a history of chest pain, breathlessness, syncope or palpitations. Provide ECG monitoring and supplemental oxygen and insert an intravenous cannula as soon as possible. Send blood samples for testing and provide analgesia (nitrates and/or morphine) and, unless contraindicated, give oral aspirin (300 mg).
ASSESSMENT
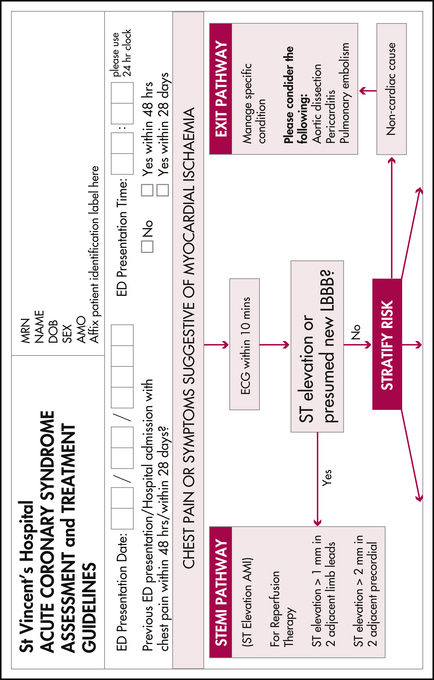
In some cases no ACS can be demonstrated and an alternative diagnosis is established, such as aortic dissection, pericarditis or pulmonary embolism
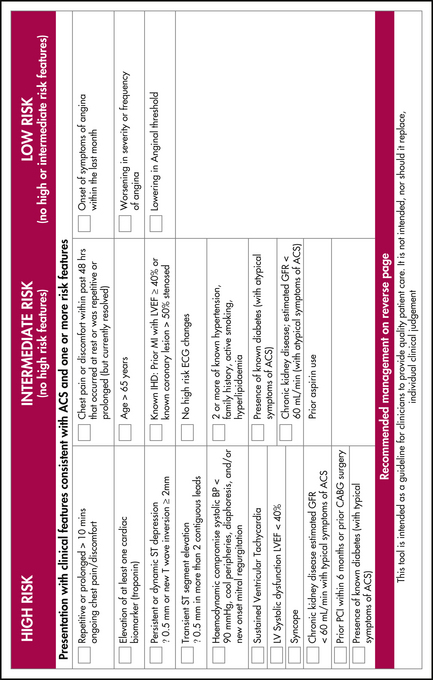
Table 7.1 Initial patient assessment and stratification
| STEACS | NSTEACS |
|---|---|
| ST-elevation acute coronary syndrome usually referred to as STEMI (ST–segment elevation myocardial injury) |
or a non-cardiovascular cause such as pneumonia, musculoskeletal pain or gastro-oesophageal disease may be identified. In a significant subgroup of presentations, immediately serious illness can be excluded and, although no diagnosis is reached, the patient can be discharged for follow-up outpatient assessment.
DIAGNOSING AND STRATIFYING ACUTE CORONARY SYNDROMES
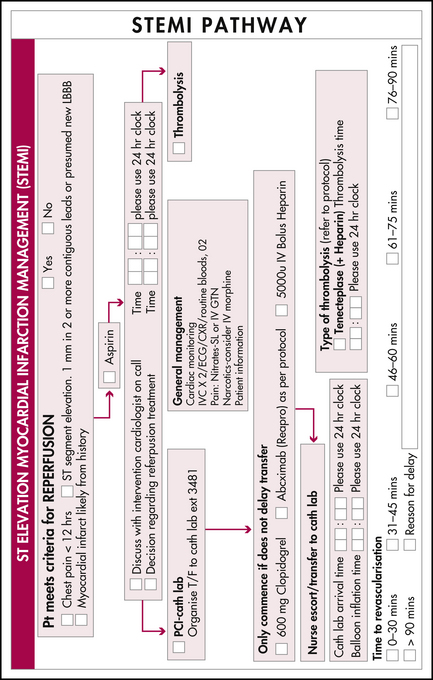
History, examination, investigation and management proceed rapidly and concurrently and senior staff should be contacted as soon as possible (see Figure 7.1).
Tests to include are listed in Table 7.2.
Table 7.2 Tests to aid in the diagnosis and stratification of patients with ACS∗
| Test | Comment |
|---|---|
| Full blood count | Anaemia or polycythaemia may need treatment, baseline platelet count (particularly if heparin is to be used) |
| Coagulation PT and APTT | Guides anticoagulant therapy |
| Serum chemistry | |
| Renal function | |
| Troponin I or T∗∗ | May take up to 6 hours to rise, two or more measurements over time may be required; remains elevated 5–14 days |
| Serum lipids | Initiating treatment of hyperlipidaemia within the first few days may be required |
| Blood glucose | Diabetes may be undiagnosed (especially mild NIDDM); close control of blood glucose levels improves outcomes |
| Chest X-ray | May show heart failure, cardiomegaly. Do not delay urgent treatment to obtain a CXR. Do not send potentially unstable patient out of resuscitation monitoring area for CXR |
APTT, activated partial thrombin time; CXR, chest X-ray; eGFR, estimated glomerular filtration rate; NIDDM, non-insulin dependent diabetes mellitus; PT, prothrombin time
∗ Additional tests such as high-sensitivity C-reactive protein (CRP) and B-type natriuretic protein (BNP) or Pro-BNP are still being evaluated. In some settings bedside cardiac echocardiography can be valuable as it may be able to provide information on wall motion (myocardial ischaemia or infarction), ejection fraction (heart failure, systolic or diastolic dysfunction), valvular disease (aortic stenosis, acute mitral valve chordae disruption), free wall rupture, aortic or pericardial disease. Drug screening (cocaine, amphetamines) may be relevant. An alternative diagnosis of pulmonary embolism can sometimes be made when significant right heart abnormality is seen on echo.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree