Immediate Management of Life-Threatening Problems
First, determine if the patient is stable or not. Distinguishing stability or instability is best performed pragmatically through multiple, simultaneous steps.
Look at the patient and identify if the patient is ill appearing.
Evaluate responsiveness, focusing on eye opening, and verbal and motor responses.
Assess airway, breathing, and circulation.
Record and review a complete set of vital signs.
Gauge perfusion to the brain and extremities.
Continue the physical examination with inspection of the abdomen, looking for signs of an acute abdomen: rebound tenderness, board-like rigidity or guarding, or an obvious pulsatile mass.
If appropriate, perform a rectal examination earlier than later, inspecting for blood.
In the acute patient, emergency bedside ultrasound is helpful in identifying aortic aneurysm/dissection, intraperitoneal fluid, and/or IVC collapse (volume status).
If instability is confirmed, measures to stabilize the patient must be taken immediately.
Caution—A number of patients presenting to the ED with abdominal pain will have a source of that pain outside the abdomen, anatomically, as when epigastric or upper abdominal pain is caused by an acute myocardial infarction, pulmonary embolus, or pneumonia. Occasionally, abdominal pain is due to a metabolic derangement, as is the case with diabetic ketoacidosis. In brief, the differential diagnosis should extend beyond intra-abdominal pathology.
Some patients with abdominal pain will require surgical evaluation. Those requiring early surgical evaluation or intervention include patients with an acute abdomen, a pulsatile abdominal mass, or shock with abdominal pain. If hypotension or hemodynamic instability is present with abdominal pain, especially with gastrointestinal bleeding or a rigid abdomen, there is a strong possibility of underlying life-threatening pathology, and surgical consultation should be immediately sought. One of the most critical decisions an ED physician can make is whether a surgeon should be involved or not. Therefore, it is of paramount importance to consider this question early and frequently throughout the evaluation.
Treat hypotension or frank shock (Chapter 11).
Give oxygen at a rate of 2–10 L/min by nasal cannula or mask. Keep oxygen saturation above 95%.
Insert two large-bore (≥16-gauge) intravenous catheters in an upper extremity.
Obtain blood for a complete blood count (CBC) with differential, serum electrolyte measurements, lipase measurement, renal function tests, liver function tests, serum pregnancy test, serum lactate, and a rapid bedside glucose test. Also, send a tube of blood for typing and crossmatching.
Consider emergency bedside ultrasound to evaluate for free intraperitoneal fluid and aortic aneurysm.
Immediately begin rapid infusion of crystalloid solution. Titrate rate of infusion to the blood pressure; initially, give a 1-L bolus over 10–20 minutes (adult dose). Remember to exercise caution in patients with congestive heart failure.
Insert a urinary catheter to monitor urine output, a sensitive indicator of visceral blood flow. Send a urine sample for analysis.
Obtain a blood gas to assess the patient’s acid–base status and overall physiologic condition.
Insert a nasogastric tube if the patient shows evidence of intestinal obstruction. Also consider NG placement if peritonitis, severe ileus, or gastrointestinal bleeding are suspected.
Obtain a 12-lead ECG and begin continuous cardiac monitoring.
If bacterial peritonitis or perforated viscous is suspected, begin broad-spectrum antibiotics after appropriate cultures have been obtained (Table 15–1).
| Minor to Moderate Disease | |
|---|---|
| Drug | Dose |
| Ampicillin-sulbactam | 3.0 g IV every 6 hours |
Metronidazole PLUS
| 500 mg IV every 6 hours
|
| Moxifloxacin | 400 mg IV daily |
| Ertapenem | 1 g IV daily |
| Ticarcillin-clavulanate | 3.1 g every 6 hours |
| Severe Disease | |
| Drug | Dose |
| Imipenem | 500 mg IV every 8 hours |
| Meropenem | 1 g IV every 8 hours |
| Piperacillin-Tazobactam | 4.5 g IV every 8 hours |
|
|
|
|
Note: Persistent shock despite fluid resuscitation in the patient with acute abdominal pain requires urgent laparotomy. Some patients will not be such that they can be stabilized prior to surgical intervention and must be taken for emergency intervention despite instability. Early surgical consultation is imperative.
1This chapter is a revision of the chapter by Melissa Platt, MD, Samir Doshi, MD, & Eric Telfer, MD, from the 6th edition.
Further Evaluation of the Patient with Abdominal Pain
After the patient has been stabilized, reassess as described below unless immediate surgery is required (Table 15–2).
| Disease | Location of Pain and Prior Attacks | Mode of Onset and Type of Pain | Associated Gastrointestinal Symptoms | Physical Examination | Helpful Tests and Examinations |
|---|---|---|---|---|---|
| Acute appendicitis | Periumbilical or localized generally to right lower abdominal quadrant | Insidious to acute and persistent | Anorexia common; nausea and vomiting in some | Low-grade fever, epigastric tenderness initially; later, right lower quadrant | Slight leukocytosis; CT scan of the abdomen or ultrasound of the appendix may be helpful if diagnosis is uncertain |
| Intestinal obstruction | Diffuse | Sudden onset; Crampy | Vomiting common | Abdominal distention; high-pitched rushes | Dilated, fluid-filled loops of bowel on abdominal X-ray; CT scan with contrast |
| Perforated duodenal ulcer | Epigastric; history of ulcer in many | Abrupt onset; steady; worse when supine | Anorexia; nausea and vomiting | Epigastric tenderness; involuntary guarding | Upright abdominal X-ray shows air under diaphragm; CT scan |
| Diverticulitis | Left lower quadrant; history of previous attacks | Gradual onset; steady or crampy | Mild diarrhea common | Fever common; mass and tenderness in left lower quadrant | CT scan shows inflammation |
| Inflammatory bowel disease | Diffuse; primarily in lower abdomen; prior attacks common | Gradual onset; often crampy | Diarrhea common, often with blood and mucus | Fever; diffuse abdominal tenderness | Blood and leukocytes in stool; CT scan; abnormal results on proctosigmoidoscopy or barium enema |
| Acute cholecystitis | Epigastric or right upper quadrant; may be referred to right shoulder | Insidious to acute | Anorexia; nausea and vomiting | Right upper quadrant tenderness; may have fever | Right upper quadrant sonography shows gallstones, gall bladder wall thickening or pericholecystic fluid; radionucleotide scan shows nonvisualization of the gallbladder |
| Biliary colic | Intermittent right upper quadrant; prior attacks common | Often abrupt onset; dull to sharp | Anorexia; nausea and vomiting common | Right upper quadrant tenderness | Sonography shows gallstones |
| Ischemic colitis | Epigastric; diffuse; prior attacks common | Often abrupt; crampy | Diarrhea, commonly bloody | Diffuse abdominal tenderness; vascular disease elsewhere | Barium enema shows “thumbprinting” of mucosa; CT scan; visceral angiography shows vascular obstruction |
| Ruptured abdominal aortic aneurysm | Epigastrium and back | Abrupt; sharp and severe | Variable; may be none | Hypotension or shock; abdominal aneurysm; pulsatile mass | Sonography, CT scan, or anglography shows aneurysm |
| Rupture of spleen | Left upper quadrant or diffuse; may be referred to left shoulder; history of trauma common | Abrupt; severe | Usually none | Hypotension or shock; peritonitis; left upper quadrant tenderness; fractured left ribs in some | CT scan or liver–spleen scan shows rupture; U/S shows free fluid |
| Renal colic | Costovertebral or along course of ureter | Sudden; severe and sharp | Frequently nausea and vomiting | Flank tenderness | Hematuria; noncontrast CT scan of the abdomen or excretory urogram (obstruction, hydronephrosis) |
| Acute pancreatitis | Epigastric penetrating to back | Acute; persistent, dull, severe | Anorexia; nausea and vomiting common | Epigastric tenderness | Elevated serum lipase; CT scan shows pancreatic inflammation |
| Acute salpingitis | Bilateral adnexal; later, may be generalized | Gradually becomes worse | Nausea and vomiting may be present | Cervical motion elicits tenderness; mass if tubo-ovarian abscess is present | Ultrasound can rule out tubo-ovarian abscess |
| Ectopic pregnancy | Unilateral early; may have shoulder pain after rupture | Sudden or intermittently vague to sharp | Frequently none | Adnexal mass; tenderness | Pelvic ultrasound reveals adnexal mass or blood; positive pregnancy test |
The importance of a good, thorough history cannot be overemphasized. The initial assessment and plan will be based on the physician’s initial “stability” assessment and the meticulous history obtained thereafter. That history is crucial in helping the physician decide what laboratory and radiographic studies to acquire, what the differential diagnosis is, whether the patient needs surgical evaluation, whether the patient requires admission, etc.
The approach offered here is intended for nontraumatic abdominal pain. A history of abdominal trauma requires a different diagnostic approach, which has been discussed in Chapter 25. Pelvic pain in the female has been discussed in more detail in Chapter 38.
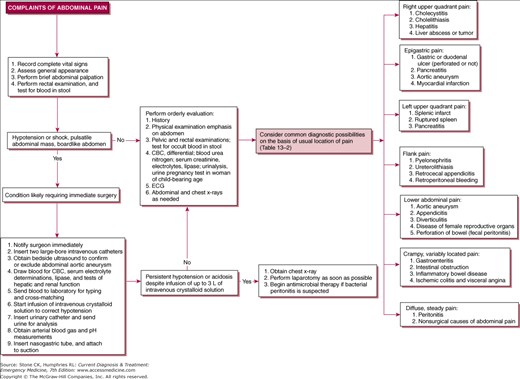
See Figure 15–2 and Table 15–2.
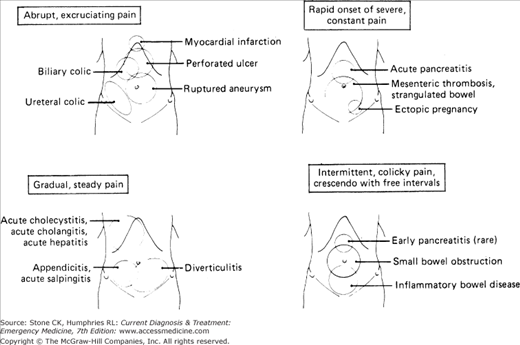
The abrupt onset of severe abdominal pain should suggest a vascular accident or a rupture of a hollow viscus, especially if its severity is maximal at onset. On the other hand, pain that begins abruptly, but is only moderately severe at the time of onset, and worsens rapidly with time suggests neprholithiasis, acute pancreatitis, mesenteric thrombosis, or small-bowel strangulation. If the pain is of lower abdominal or pelvic origin, ruptured ectopic pregnancy or ovarian follicle cyst should also be considered in females (Chapter 38).
Gradual onset of slowly worsening pain is the characteristic of peritoneal inflammation or infection. Patients with appendicitis or diverticulitis often report a gradual onset of pain that escalates.
See Figure 15–2.
Severe abdominal pain may be caused by many conditions, including renal colic, biliary colic, and various vascular conditions such as myocardial infarction, mesenteric ischemia, and rupture of an abdominal aortic aneurysm. Other conditions that cause severe pain include acute pancreatitis, perforation of a hollow viscus, and peritonitis.
Dull, vague, poorly localized pain is typically gradual in onset. When these two findings are coupled, they suggest an inflammatory process or a low-grade infection, appendicitis, or diverticulitis, for example.
Intermittent, crampy abdominal pain is common in gastroenteritis. Crampy pain that occurs in regular cycles, rising and falling in a crescendo fashion, is more characteristic of a mechanical small-bowel obstruction, especially if pain-free intervals are present.
Occasionally, a patient will complain of a sense of abdominal fullness with a notion that a bowel movement will provide relief. A bowel movement, whether spontaneous or induced, usually fails to relieve discomfort, however. This is known as the “gas stoppage” sign and is characteristic of retrocecal appendicitis. It may also be present when any inflammatory lesion is walled off from the free peritoneal cavity.
The parietal peritoneum is innervated by somatic nerve fibers, producing pain that is generally well localized. In contrast, pain arising from visceral fibers alone tends to be poorly localized. Common examples of conditions associated with visceral pain sensation are hollow viscus distention and visceral ischemia.
(See Table 15–2.) In general, when abdominal pain becomes localized, it does so over or near the involved viscus, the right lower quadrant pain of appendicitis or the right upper quadrant pain of cholecystitis, for example. On the other hand, anatomic variants (eg, retrocecal appendix) must be kept in mind, and one must maintain a wide differential, considering all the possible etiologies of the pain.
Radiation of pain or shift in localization of pain has particular diagnostic significance.
Ipsilateral diaphragmatic irritation by air, blood, or infection in the peritoneal cavity can cause shoulder pain. A classic example is cholecystitis, which may be associated with right shoulder pain.
Diffuse periumbilical and epigastric pain that gradually localizes to the right lower quadrant is a classic sign of appendicitis. With early appendicitis, only the visceral peritoneum surrounding the appendix is inflamed, and the localization is therefore poor. As the inflammation spreads to the parietal peritoneum, the pain localizes to the right lower quadrant. The retrocecal appendix, which is found in 15% of cases, is an important exception, with pain remaining poorly localized secondary to lack of parietal peritoneum involvement.
Pain radiating from the flank to the groin or genitalia usually signifies ureteral colic, as seen in urolithiasis. The physician must also consider testicular pathology such as testicular torsion in any male patient with abdominal pain, whether that pain radiates to the groin or not.
Anorexia, nausea, and vomiting are common with abdominal pain, especially abdominal pain having its source in the upper abdomen; nonetheless, severe intra-abdominal processes can occur without any of these symptoms. For example, one may retain a normal appetite with appendicitis if the appendix is isolated from the peritoneum, as may be the case with a retrocecal appendix or an appendix that is isolated by omentum.
Nausea and vomiting are infrequently the initial or dominant symptoms with surgical acute abdomen, making these symptoms preceding abdominal pain more indicative of less acute conditions such as food poisoning, gastroenteritis, acute gastritis, and acute pancreatitis. However, these symptoms may have developed after initial onset of pain in abdominal emergencies by the time the patient has sought medical attention.
Fever is common with many causes of abdominal pain, usually suggesting infection. Fever with continual rigors is most common in infections of the biliary and urinary system (eg, cholangitis and pyelonephritis). Fever with chills, jaundice, and hypotension suggests suppurative cholangitis, a surgical emergency. High fever with peritoneal signs in a female patient with no apparent general systemic illness otherwise is suggestive of acute salpingitis with pelvic peritonitis. Interestingly, appendicitis with high fever and rigors is uncommon unless peritonitis, most likely from viscus perforation, has developed. Recall that absence of fever is common in the elderly and immunosuppressed patients.
Constipation and obstipation may suggest intestinal obstruction or ileus but are usually not the primary symptoms in acute surgical intra-abdominal disease. Diarrhea, though common with gastroenteritis, is a nonspecific symptom that can be associated with colitis, diverticulitis, appendicitis, and salpingitis.
The basic steps of the physical examination of the acute abdomen are outlined in Table 15–3. Remember that physical findings may be subtle in elderly or immuno-compromised patients.
|
The abdominal examination starts with visual inspection of abdomen and external genitalia. Significant findings include masses, distention, pregnancy, previous surgical scars, ecchymosis, a board-like abdomen, and stigmata of severe hepatic disease.
While a silent abdomen, ie, complete absence of audible peristalsis, is thought to signify diffuse peritonitis, peristalsis may persist in the face of established peritonitis. Also, note that because peristalsis is related to meal intake, it may be necessary to listen for as long as 2–3 minutes to establish the absence of peristalsis, especially in those who have not eaten in quite a while. In general, it must be understood that auscultation may be less contributory to diagnosis, especially with findings of absent or normal bowel sounds. Even so, high-pitched bowel sounds can be suggestive of bowel obstruction.
Examine the inguinal and femoral canals and the genitalia, primarily looking for incarcerated hernias that may be causing intestinal obstruction. This must be done by asking the patient to cough but should be done gently so as to cause as little discomfort as possible. It is optimal if this portion of the examination can take place with the patient standing as well.
In most acute inflammatory conditions arising within the abdomen, coughing elicits pain in the involved area. Directing the patient to point one finger to the area of pain provides objective localization of the lesion. With this information, the examiner can proceed to examine the abdomen and deliberately examine last the area now known to be most tender.
The next step is to establish the presence or absence of true muscle spasm by gently depressing the rectus abdominis muscle without causing pain. Have the patient flex their knees at 90° to aid in relaxation of the abdominal muscles. The patient is then asked to take a long, slow breath. If the spasm is voluntary, the muscle will immediately relax underneath the gentle pressure of the palpating hand. If there is true spasm, the muscle will remain taut and rigid through the respiratory cycle. This maneuver alone may be sufficient to establish the presence of peritonitis.
Except for rare neurologic disorders, renal colic, or rectus muscle injury, only peritoneal inflammation produces abdominal muscle rigidity. In renal colic, the spasm is confined to the entire rectus muscle on the involved side. This distinction is important because marked rigidity of the entire length of one rectus muscle with relaxation of the opposite rectus cannot occur in peritonitis as the peritoneal cavity is not compartmentalized. In generalized peritonitis, both muscles are usually involved to the same degree.
Abdominal tenderness must be assessed with one finger, because it is impossible to localize peritoneal inflammation accurately if palpation or tenderness is done with the entire hand. Careful one-finger palpation, beginning as far away as possible from the area of tenderness elicited by coughing and gradually working toward it, will usually enable the examiner to delineate the area of abdominal tenderness precisely. In early acute appendicitis, this area is often no larger than 2–3 cm in diameter. Diffuse abdominal tenderness without involuntary rigidity of musculature suggests gastroenteritis or some other inflammatory process of the intestines without peritonitis. It is helpful if the examiner divides the abdomen into four quadrants during this section of the examination and tries to localize the area of pain.
Do not test for peritoneal inflammation by looking for classic rebound tenderness (deep palpation of the abdomen with abrupt release). This maneuver yields little additional information, often causes considerable discomfort, and may limit further examination.
Gentle percussion of the costovertebral angles should follow palpation. This should elicit pain in individuals with pyelonephritis, retroperitoneal abscesses, and retrocecal appendicitis. Excessively vigorous percussion is not helpful in localizing tenderness and may limit further examination.
Having established the presence or absence of muscular rigidity and localized the area of tenderness, the examiner now palpates more deeply for the presence of abdominal masses. Often, it is difficult to perform a reliable physical examination of the abdomen in an anxious patient. Some patients are so anxious that they begin to guard with voluntary contraction of the abdominal musculature before the examiner performs even light palpation. This barrier to palpation can occasionally be overcome by palpating with a stethoscope during auscultation of bowel sounds or by asking the patient to flex the legs at the hips and knees.
Among the more common lesions identifiable by careful palpation in patients with acute abdominal pain are the distended, tender gallbladder found in acute cholecystitis, the right lower quadrant tender mass of appendicitis with early abscess formation, the left lower quadrant mass of sigmoid diverticulitis, and the midline pulsatile mass of abdominal aortic aneurysm.
Percussion aids in determining size and density of underlying matter. It can be used in estimation of liver, spleen, or bladder size and in differentiating etiologies of abdominal distention, specifically organomegaly, ascites, and obstruction.
Several maneuvers in physical examination may help localize an acute abdominal lesion.
The patient flexes the thigh against the resistance of the examiner’s hand. A painful response indicates an inflammatory process involving the psoas muscle.
The patient’s thigh is flexed to a right angle and gently rotated, first internally and then externally. If pain is elicited, an inflammatory lesion involving the obturator muscle (pelvic appendicitis, diverticulitis, pelvic inflammatory disease) is present.
As the patient takes a slow, deep breath, the examiner elicits an abrupt cessation in inspiration by deep palpation of the right upper quadrant. This finding is suggestive of cholecystitis.
The importance of pelvic and rectal examination cannot be overstressed. The pelvic examination in women provides essential information not revealed by other maneuvers. Evaluation of lower abdominal pain in women is discussed further in Chapter 38.
Examination of stool for gross or occult blood must be considered in patients with abdominal pain. Occult blood may result from intestinal tumors, inflammatory bowel disease, ischemic bowel disease, and lesions of the upper gastrointestinal tract. More specifically in men, rectal examination plus simultaneous lower abdominal palpation often reveals masses or localized pain not disclosed by abdominal examination alone.
Bedside ultrasound is increasingly used as an adjunct to the physical exam in the emergency department. It is now a required component of training for all emergency medicine residencies. Uses include:
Focused Abdominal Sonography for Trauma (FAST exam).
Identification of free peritoneal fluid including blood, pus, or ascites.
Measurement of the cross-sectional abdominal aortic diameter to identify dissection or aneurysm.
Transvaginal and/or transabdominal ultrasound for identification of an intrauterine pregnancy, ectopic pregnancy, and other anatomic gynecological pathologies.
Identification of gall stones, a dilated common bile duct, or pericholecystic fluid.
Evaluation for hydronephrosis.
Testing of IVC collapse to evaluate intravascular volume status.
Such testing will be increasingly widespread as the skills required become commonplace among emergency physicians.
CBC with differential, lipase measurements, and urinalysis are indicated in most cases. Electrolyte determinations and tests of renal function are especially important if vomiting, diarrhea, hypotension, or shock are present. Liver function testing can be helpful in patients with suspected liver or gallbladder disease.
The hematocrit reflects changes both in plasma volume and red cell volume. It is diagnostically most useful if markedly elevated (indicating dehydration) or depressed (indicating anemia). Furthermore, the hematocrit can be followed to assess for, or estimate the degree of, blood loss. The hematocrit should be corrected toward normal values in preparation for surgery in hemodynamically unstable patients.
The white cell count may be helpful if it is significantly elevated. However, it is neither sensitive nor specific. Normal or even low counts can occur in established peritonitis or sepsis (although usually with a marked shift to the left), and elevated counts may occur in gastroenteritis. A shift to the left on a blood smear may be a clue to an inflammatory reaction in the presence of a normal or only moderately elevated white count. Recall that in elderly and immunosuppressed patients the count may be low or normal.
Patients with abdominal pain and elevated lipase usually have acute pancreatitis. Although serum amylase is often still obtained, lipase is both more sensitive and specific than serum amylase and has greater diagnostic value. Serum amylase may also be elevated in other conditions such as obstruction, mesenteric ischemia, perforated viscus, renal failure, ectopic pregnancy. If pancreatitis is suspected, ordering lipase alone may be sufficient. Unfortunately, the degree to which either marker is elevated cannot predict the severity of the condition or any associated complications of pancreatitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree