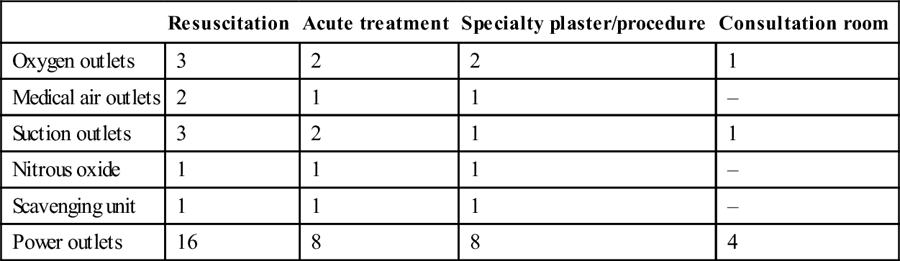
Edited by George Jelinek Sue Ieraci and Julie Considine Patients requiring emergency care have the right to timely care by skilled staff. The aim of staffing an emergency department is ultimately to provide care in an acceptable time according to the patient’s clinical urgency (triage category). Staff working in the emergency department also have the right to safe and manageable working conditions and reasonable job satisfaction. As the activity of an emergency department fluctuates in both volume and acuity, a threshold level of staffing and resources is required in order to be prepared for likely influxes of patients. In addition, the staffing number and mix needs to take account of the important teaching role of emergency departments. The precise numbers and designation of medical, nursing, allied health and other staff employed will be determined by the local work practices (what tasks are carried out and by whom). This chapter discusses staffing requirements under the current Australasian model of emergency department work practices. This includes a major supervisory and teaching role for consultants and a significant proportion of specialist trainees and junior medical staff in the medical workforce, with a range of tasks, including venepuncture, test requisitioning and written documentation. In addition, roles are expanding into wider realms, such as toxicology, ultrasound and academic and observation medicine. Nursing roles range from bedside monitoring, physical care and treatment to advanced practice roles, including the initiation of tests and treatment. Emergency department (ED) case mix and costing studies have sought to measure the medical time commitment for various clinical conditions. Table 27.1.1 describes the approximate average medical time commitment for each of the Australasian Triage Scale categories [1]: Table 27.1.2 Benchmarks for waiting time by triage category Table 27.1.1 Australasian Triage Scale categories The medical workforce of Australasian emergency departments currently includes the following categories: The specialist practice of emergency medicine includes non-clinical roles (including departmental management and administration, planning, education, research and medicopolitical activities) as well as clinical roles. The non-clinical workload of an individual department varies with its size and role, the structure of its staffing and the other management systems within the institution. For senior staff, clinical work generally includes coordination of patient flow, bed management and supervision and bedside teaching of junior staff, in addition to direct patient care. Some emergency physicians may have other particular roles, such as retrieval and hyperbaric medicine or toxicology services. The increasing number of academic staff may have major research and teaching commitments. To cover these roles, the ACEM recommends a minimum of 30% non-clinical time for consultants (more for directors of departments and directors of emergency medicine training) and 15% non-clinical time for registrars. Throughout Australasia, EDs are experiencing increasing levels of activity. The calculation of medical staff numbers required for a particular department must include not only the extent of consultant cover required, but also the clinical workload and performance, local work practices and the nature of clinical and non-clinical roles. Because of variations in roles and work practices between sites, it is not possible to devise a staffing profile that is universally appropriate. Other recent changes in staffing patterns include employment across a network, increasing part-time work and sessional contract arrangements. Many emergency physicians are diversifying their practice profile to achieve a balanced and sustainable career, combining salaried and contract work, different types of hospitals and part-time work with a range of other interests. Australian models for calculating ED nursing workload include the Emergency Care Workload Unit [3] (based on triage category and admission status) and the Victorian Nurse-to-Patient Ratio model [4] (using patient dependencies). Additionally, a minimum skill mix is required to manage the acute and complex workload. In addition to the bedside nursing workload, there are requirements to provide for education and training, patient flow and both clinical and departmental administrative roles. Larger departments require clinical managers on every shift. In Australia, there are three levels of nurses registered with the Australian Health Professionals Regulation Agency (AHPRA): Enrolled nurses work under the supervision of registered nurses and their scope of practice is generally limited to general adult or paediatric areas. One of the major changes to enrolled nurse scope of practice in recent years is their ability to administer medications and, depending on their level of education and registration notation, they may administer oral or parenteral (including intravenous) medications. The majority of nurses working in emergency departments are registered nurses who have completed a 3-year bachelor degree typically followed by a 12-month graduate nurse programmme. In many states, 6–12 month transition programmes to specialty practice in emergency nursing are offered to novice nurses wishing to pursue a career in emergency nursing and are often a precursor to postgraduate studies in emergency nursing. Australian emergency nurses have one of the highest standards of education worldwide with the majority holding a graduate certificate or graduate diploma in emergency nursing. Postgraduate qualifications are considered by many as the industry standard for complex emergency nursing roles, such as resuscitation and triage. Triage assessment is a nursing role in Australia and emergency nurses are often responsible for advanced patient assessment, initiation of investigations and symptom relief care prior to medical assessment. Emergency nurses are also primarily responsible for ongoing surveillance and escalation of care in the event of deterioration. Advanced emergency nursing roles for postgraduate qualified emergency nurses are widespread in Australia and nurse initiated pathology, X-rays and analgesia are among common examples. There are also a number of Masters and PhD prepared emergency nurses in Australia working in various advanced clinical roles, joint clinical–academic appointments, nursing education and nursing management. At the time of writing, there were over 700 endorsed nurse practitioners in Australia and emergency nursing has the largest cohort of nurse practitioners. In Australia, to be endorsed as a nurse practitioner, nurses must complete a clinically based master’s degree or a specific nurse practitioner master’s degree, demonstrate experience in advanced nursing practice in a clinical leadership role in emergency nursing and have undertaken an approved course of study for prescribing scheduled medicines as determined by the NMBA. Nurse practitioners form a key workforce strategy in managing demand for emergency care and are able independently to manage specific patient groups within their defined scope of practice, including prescribing medications, ordering diagnostic tests, referring to specialists and discharging patients home. Published research shows that emergency nurse practitioners can provide safe, efficient and timely care and are a valuable member of the emergency department team [5,6]. Allied health, clerical and other ancillary staff are essential to the efficient provision of emergency department services. They should be specifically trained and experienced for emergency department work. Clerical staff have a crucial role, encompassing reception, registration, data entry and communications within and outside the department, as well as maintenance of medical records. Dedicated paramedical staff, including therapists and social workers, are important in providing thorough assessment and management of patients, including participating in disposition decisions and discharge support. Other staff, such as porters and ward assistants, play an important role in releasing clinical staff from non-clinical roles as well as movement of patients within and beyond the emergency department. Traditional hospital work practices involve systems and tasks that are inefficient for the smooth running of modern, busy emergency departments. In a work environment with a rapid patient throughput and large numbers of staff, efficient work practices are crucial in optimizing clinical performance as well as job satisfaction. A review of staff numbers and seniority cannot provide maximum benefit without consideration of the way the work is done, what tasks are done and by whom. A review of emergency department work practices can encompass the following principles: As the emergency department workforce develops greater seniority and specialization and the demands of patient care increase, it is no longer possible to justify outdated work practices. Local research has shown that it is possible to improve clinical service provision by reorganizing roles and tasks in a sustainable way [7]. The opportunity exists to create a work environment that both delivers good clinical service and is rewarding and satisfying for staff. Matthew WG Chu The emergency department (ED) is a core clinical unit within a hospital. The experience and satisfaction of patients attending the ED are significant contributors to the public image of the hospital. Its primary function is to receive, triage, stabilize and provide emergency care to patients who present with a wide range of undifferentiated conditions which may be critical to semi-urgent in nature. The ED may contribute between 15 and 75% of a hospital’s total number of admissions. It plays an important role in the hospital’s response to major incidents and trauma and in the reception and management of disaster victims. To optimize its core function, the department should be purpose-built, providing a safe environment for patients, their carers and staff. The physical environment includes an effective communication system, appropriate signposting, adequate ambulance access and clear observation of relevant areas from the triage area. There should be easy access to the resuscitation area and quiet and private areas should cater for patients and their relatives. Adequate staff facilities and tutorial areas should be available. Clean and dirty utilities and storage areas are also required. The design of the department should promote rapid access to every area with the minimum of cross-traffic. There must be proximity between the resuscitation and the acute treatment areas for non-ambulant patients. Supporting areas, such as clean and dirty utilities, the pharmacy room and equipment stores, should be centrally located to prevent staff traversing long distances. The main aggregation of clinical staff will be at the staff station in the acute treatment area. This is the focus around which the other clinical areas should be grouped. Lighting should conform to national standards and clinical care areas should have exposure to daylight whenever possible to minimize patient disorientation. Climate control is essential for the comfort of both patients and staff. Each clinical area needs to be serviced with medical gases, suction, scavenging units and power outlets. The minimum suggested configuration for each type of clinical area is outlined in Table 27.2.1. Table 27.2.1 Configurations for clinical areas Medical gases should be internally piped to all patient care areas and adequate cabling should ensure the availability of power outlets to all clinical and non-clinical areas. Although patient and emergency call facilities are often considered, there is often inadequate provision for telephone and information technology ports. The availability of wireless technology to support equipment, such as computer on wheels (COWS), is desirable. Emergency power must be available to all lighting and power outlets in the resuscitation and acute treatment areas. All computer terminals in the department should have access to emergency power and emergency lighting should be available in all other areas. The electricity supply should be surge protected to protect electronic and computer equipment, physiological monitoring areas should be cardiac protected and other patient care areas should be body protected. Approximately 35–45% of the total area of the department is circulation space. An example of this would be the provision of corridors wide enough to allow the easy passage of two hospital beds with attached intravenous fluids. Although circulation space should be kept to a minimum, functionality, fire safety and occupational health and safety requirements also need to be considered. The floor covering in all patient care areas should be durable and non-slip, easy to clean, impermeable to water and body fluids and with properties that reduce sound transmission and absorb shocks. Areas accommodating the administrative functions, interview and counselling and support of distressed relatives should be carpeted. The appropriate size of the ED depends on a number of factors: the census, patient mix and acuity, the admission rate, the defined performance levels manifested in waiting times, the length of stay of patients in the ED and the role delineation of the department. Departments of inadequate size are uncomfortable for patients, often function inefficiently and may significantly impair patient care. Overcrowding of patients increases mortality and morbidity with the risk of infectious disease transmission and increases harmful cognitive stimulation for patients with mental disturbance. For the average Australasian ED with an admission rate of approximately 25–35%, its total internal area (excluding departmental radiological imaging facilities and observation/holding ward) should be approximately 50 m2/1000 yearly attendances. The total number of patient treatment areas (excluding interview, plaster and procedure rooms) should be at least 1/1100 yearly attendances and the number of resuscitation areas should be at least one for every 15 000 yearly attendances. It is recommended that, for departments with average patient acuity, at least half the total number of treatment areas should have physiological monitoring available. The design of individual treatment areas should be determined by their specific functions. Adequate space should be allowed around the bed for patient transfer, assessment, performance of procedures and storage of commonly used items. The use of modular storage bins or other materials employing a similar design concept should be considered. To prevent transmission of confidential information, each area should be separated by solid partitions that extend from floor to ceiling. The entrance to each area should be able to be closed by a movable partition or curtain. Each acute treatment bed should have access to a physiological monitor. Central monitoring is recommended and monitors should ideally be of the modular type, with recording and print capabilities. The minimum monitored physiological parameters should include oxygen saturation (SpO2), non-invasive blood pressure (NIBP), electrocardiogram (ECG) and temperature. Monitors may be mounted adjacent to the bed on an appropriate pivoting bracket or be movable. All patient care areas, including toilets and bathrooms, require individual patient call facilities and emergency call facilities, so urgent assistance can be summoned when required. In addition, an examination light, a sphygmomanometer, ophthalmoscope and otoscope, waste disposal unit should all be immediately available. Hand washing facilities should be easily accessible. This area is used for the resuscitation and treatment of critically ill or injured patients. It must be large enough to fit a standard resuscitation bed, allow access to all parts of the patient and allow movement of staff and equipment around the work area. As space must also be provided for equipment, monitors, storage, wash-up and disposal facilities, the minimum suitable size for such a room is usually 35 m2 (including storage area) or 25 m2 (excluding storage area) for each bed space in a multibedded room. The area should also have visual and auditory privacy for both the occupants of the room and for other patients, their carers and relatives. The resuscitation area should be easily accessible from the ambulance entrance and the staff station and be separate from the patient circulation areas. In addition to standard physiological monitoring, invasive pressure, capnography and temperature probe monitoring should be available. Other desirable features include a ceiling-mounted operating theatre light, a radiolucent resuscitation trolley with cassette trays, overhead X-ray and lead lining of walls and partitions between beds. This area is used for the assessment, treatment and observation of patients with acute medical or surgical illnesses. Each bed space must be large enough to fit a standard mobile bed, with adequate storage and circulation space. The recommended minimum space between beds is 2.4 m and each treatment area should be at least 12 m2. All of these beds should be positioned to enable direct observation from the staff station and easy access to the clean and dirty utility rooms, procedure room, pharmacy room and patient shower and toilet. These rooms should be used for the management of patients who require isolation, privacy or who are a source of visual, olfactory or auditory distress to others. Deceased patients may also be placed there for the convenience of grieving relatives. These rooms must be completely enclosed by floor-to-ceiling partitions but allow controlled visual access and have a solid door. Each department should have at least two such rooms. The isolation room is used to treat potentially infectious patients. The isolation room should be located in an area which does not allow cross infection to other patients in the emergency department. Each isolation room should have negative-pressure ventilation, an ante room with change and scrub facilities and be self-contained with en-suite facilities. A decontamination area should be available for patients contaminated with toxic substances. In addition to the design requirements of an isolation room, this room must have a floor drain and contaminated water trap. The decontamination area should be directly accessible from the ambulance bay and be located in an area which will prevent the ED from being contaminated in the event of a chemical or biological incident. Single rooms should otherwise have the same requirements as acute treatment area bed spaces. This is a specialty area designed specifically for the assessment, protection and containment of patients with actual or potential behavioural disturbances. Ideally, each unit comprises two separate but adjacent rooms allowing for interview, behavioural assessment and treatment functions. Each room should have two doors large enough to allow a patient to be carried through and must be lockable only from the outside. One of the doors may be of the ‘barn door’ type, enabling the lower section to be closed while the upper section remains open. This allows direct observation of and communication with the patient without requiring staff to enter the room. Each room should be squarely configured and be at least 16 m2 in size to enable a restraint team of five members to contain a patient without the potential of injury to a staff member. The examination/treatment room will facilitate physical examination or chemical restraint when indicated. The unit should be shielded from external noise, located as far away as possible from external sources of stimulation (e.g. noise, traffic) and must be designed in such a way that direct observation of the patient by staff outside the room is possible at all times. Services, such as electricity, medical gases and air vents or hanging points, should not be accessible to the patient. It is preferable that furniture be made of material which would prevent it being used as a weapon or inflicting self-harm. A smoke detector should be fitted and closed-circuit television may be considered as an adjunct to direct visual monitoring. Psychiatric Emergency Care Centres (PECC) have been introduced in some hospitals. They are located within or adjacent to an ED and consist of 4–6 rooms with the configurations previously mentioned. Governance is dictated by the local operational policies. Consultation rooms are provided for the examination and treatment of ambulant patients who are not suffering a major or serious illness. These rooms have similar space requirements to acute treatment area bed spaces. In addition, they are equipped with office furniture with a computer terminal, a radiological viewing panel and a basin for hand washing. Consultation rooms may be adapted and equipped to serve specific functions, such as ENT or ophthalmology treatment, or as part of a fast track area to treat patients with non-complex single system diseases. When the fast track model of care is adopted, the provision of an adjacent subwaiting area for patients waiting for the results of investigations will promote the efficient use of the available floor space. The plaster room allows for the application of splints, plaster of Paris and for the closed reduction of displaced fractures or dislocations and should be at least 20 m2 in size. Physiological equipment to monitor the patient undergoing procedural sedation or regional anaesthesia is required. Specific features of such a room include a storage area for plaster, splints and bandages; X-ray viewing panel/digital imaging systems facility; provision of oxygen and suction; a nitrous oxide delivery system; a trolley with plaster supplies and equipment; and a sink and drainer with a plaster trap. Ideally, a splint and crutch store should be directly accessible in the plaster room. A procedure room(s) may be required to undertake procedures, such as lumbar puncture, tube thoracostomy, thoracocentesis, peritoneal lavage, bladder catheterization or suturing. It requires noise insulation and should be at least 20 m2 in size excluding a storage area for minor equipment and supporting sterile supplies. Physiological equipment to monitor the patient undergoing procedures, a ceiling mounted operating theatre light, X-ray viewing panel/digital imaging systems facility, provision of oxygen and suction, a nitrous oxide delivery system, a waste disposal unit and hand washing facilities should all be available. A single central staff area is recommended for staff servicing the different treatment areas, as this enables better communication between, and coordination of, staff members. The staff station in the acute treatment area should be the major staff area within the department. The staff area should be of an ‘arena’ or ‘semi-arena’ design, whereby the main areas of clinical activity are directly observable. The station may be raised in order to give uninterrupted vision of patients and should be centrally located. In larger departments, interlocking pods each involving a centrally located staff station overseeing an acute treatment area may be arranged to ensure patient visibility is maximized. The staff station should be constructed to ensure that confidential information can be conveyed without breach of privacy. Sliding windows and adjustable blinds may be used to modulate external stimuli and a separate write-up area may be considered. Sufficient space should be available to house an adequate number of telephones, computer terminals, printers and data outlets and X-ray viewing panels/digital imaging systems, dangerous drug/medication cupboards, emergency and patient call displays, under-desk duress alarm, valuables storage area, police blood alcohol sample safe, photocopier and stationery store, and write-up areas and workbenches. Direct telephone lines, bypassing the hospital switchboard, should be available to allow staff to receive admitting requests from outside medical practitioners or to participate in internal or external emergencies when the need arises. A dedicated line to the ambulance and police service is essential, as is the provision of a facsimile line. A pneumatic tube system for the transport of specimens to pathology, drugs from pharmacy and the transfer of medical records and imaging requests may also be located in this area. Many EDs possess a short-stay unit, i.e. emergency medical unit (EMU) which is managed under its governance and operates as an extension of the department. The purpose of these units is to manage patients who would benefit from extended observation and treatment but have an expected length of stay of less than 24 hours. It is considered that the minimum functional unit size is eight beds. It is configured along similar lines to a hospital ward with its own staff station. The capacity is calculated to be 1 bed per 4000 attendances per year and its size will be influenced by its function and case mix. As short-stay units are usually high volume users of mental health, social work, physiotherapy, drug and alcohol and community support services, appropriate space should be allocated to allow these services to operate effectively. A medical assessment and planning unit (MAPU) or medical assessment unit (MAU) is an inpatient hospital unit which may either be co-located or built near an ED. It is managed by the inpatient medical service. The purpose is to facilitate the assessment and treatment of patients who require intensive coordinated multidisciplinary team interventions to minimize the length of stay and optimize health outcomes. The expected length of stay of patients utilizing this type of unit tends to be less than 72 hours. Its configuration and function is determined by case mix and local operational policies. It is usually configured up to 30 beds along similar lines to a hospital ward. The clean utility area requires sufficient space for the storage of clean and sterile supplies and procedural equipment and bench tops to prepare procedure trays. The dirty utility should have sufficient space to house a stainless steel bench top with sink and drainer, pan and bottle rack, bowl and basin rack, utensil washer, pan/bowl washer/sanitizer and slop hopper and storage space for testing equipment (such as for urinalysis). A separate store room may be used for the storage of equipment and disposable medical supplies. A common design fault is to underestimate the amount of storage space required for a modern department. A pharmacy/medication room may be used for the storage of medications and vaccines used by the department and should be accessible to all clinical areas. Entry should be secure with a self-closing door and the area should have sufficient space to house a refrigerator for the storage of heat-sensitive drugs and vaccines. Other design features should include spaces for a linen trolley, mobile radiology equipment, patient trolleys and wheelchairs. Beverage-making facilities for patients and relatives, a blanket-warming cupboard, disaster equipment store, a cleaners’ room and shower and toilet facilities also need to be accommodated. An interview room allows for the interviewing or counselling of patients, carers and relatives in private. It should be acoustically treated and removed from the main clinical area of the department. A distressed relatives’ room should be provided for the relatives of seriously ill or deceased patients. Consideration for the provision of two rooms should be given in larger departments to allow the separation of relatives of patients who have been protagonists in violent incidents or clashes. They should be acoustically insulated and have access to beverage-making facilities, a toilet and telephones. A single-room treatment area should be in close proximity to these rooms to enable relatives to be with dying patients and should be of a size appropriate to local cultural practices. The waiting area should provide sufficient space for waiting patients as well as relatives or carers and should be open and easily observed from the triage and reception areas. Seating should be comfortable and adequate space should be allowed for wheelchairs, prams, walking aids and patients being assisted. There should be an area where children may play and support facilities, such as television, should be available. Easy access from the waiting room to the triage and reception area, toilets and baby change rooms and light refreshment should be possible. Public telephones should be accessible and dedicated telephones with direct lines to taxi firms should be encouraged. The area should be monitored to safeguard security and patient well-being and it is desirable to have a separate waiting area for children. The waiting area should be at least 5 m2/1000 yearly attendances and should contain at least one seat per 1000 yearly attendances. The department should be accessed by two separate entrances: one for ambulance patients and the other for ambulant patients. It is recommended that each contain a separate foyer that can be sealed by the remote activation of security doors. Access to treatment areas should also be restricted by the use of security doors. Both entrances should direct the patient flow towards the reception/triage area, which should have clear vision to the waiting room and the ambulance entrance. The triage area should have access to a vital signs monitor, computer terminal, hand basin, examination light, telephones, chairs and desk and patient weighing scales. There should be adequate storage space nearby for bandages, minor medical equipment and stationery. Staff at the reception counter receive patients arriving for treatment and direct them to the triage area. After triage assessment, patients or relatives will generally be directed back to the reception/clerical area, where clerical staff will conduct registration interviews, collate the medical record and print identification labels. Clerks may interview patients or relatives at the bedside but return to the reception area to finalize the administrative details. The counter should provide seating and be partitioned for privacy for interviews. There should be the ability for direct communication between the reception/triage area and the staff station in the acute treatment area to occur. The design should take due consideration for staff safety. This area should have access to an adequate number of telephones, computer terminals, printers, facsimile machines and the photocopier. It should also have sufficient storage space for stationery and medical records. This room provides facilities for formal undergraduate and postgraduate education and meetings. It should be in a quiet, non-clinical area near the staff room and offices. Provision should be made to accommodate webcasting, webconferencing, simulation and procedural skills training as well as local lectures and small group teaching. Technological support systems integrating computer, screen projection facilities, broadband access to capitalize on advances in web technology, electronic picture archiving and communication systems are essential. Equipment to support traditional teaching methods utilizing whiteboard, tube X-ray viewer system and examination couch must also be available. Telemedicine is becoming increasing important, particularly for EDs in hospitals which are either remotely located or have limited access to subspecialty support. In these EDs, the telemedicine equipment may be located in the resuscitation area or in a dedicated room where patient encounters, such as mental health assessments, may be undertaken or the transmission of images, such as burns or digital X-rays, expedited. A dedicated facility with appropriate power and communications cabling is necessary. For facilities that receive the telemedicine transmissions, the room should be of a suitable size to allow simultaneous interactions by members of the consulting service teams. It should be in close proximity to the staff station. Offices provide space for the administrative, managerial, quality improvement activities, teaching and research roles of the ED. The number of offices required will be determined by the number and type of staff. In a large department, offices may be needed for the director, deputy director, nurse manager, academic staff, specialists, registrars, nurse consultants/practitioners, nurse educator, secretary, social worker/mental health crisis worker, information support officer, research and projects officers and clerical supervisor. Larger departments will require the incorporation of a meeting room into the office area. A room should be provided within the department to allow staff a break and to relax from the intensity of their clinical work. Food and drink should be able to be prepared and stored and appropriate table and seating arrangements should be provided in bright and attractive surroundings. It should be located away from patient care areas and have access to natural lighting and appropriate floor and wall coverings. A staff change area with lockers, toilets and shower facilities should also be provided. Over the last 20 years, EDs have been facing significant challenges. There has been a never-ending increase in demand. The work environment has become increasingly pressured. This has been compounded by resource constraints and the introduction of electronic information management technology. The provision of care has been increasingly complex. Changes in technology have enabled the management of greater numbers of patients in the community who would previously have required hospitalization. As financial pressures on hospitals have also increased, the importance of the ED has grown considerably and modern departments have significantly expanded facilities. Future design considerations are likely to centre on advances in the areas of information technology, telecommunications and newer non-invasive diagnostic modalities. In addition to these technologically driven changes, a greater emphasis will be placed on developing ED design configurations which will support redefined service delivery models to maximize efficient work practices aimed to minimize the number of patient moves, to ensure patients receive timely definitive care and to allow time-critical interventions to be delivered. Computerized patient tracking systems using electronic tags and built-in sensors will provide additional information that may further improve operational efficiency. The electronic medical record will make detailed medical information immediately available and will greatly facilitate the provision of timely care, quality improvement and research activities. Digital radiography, personal communication devices, voice recognition systems, wireless technology and portable computers and expanded telemedicine facilities will make the ED of the future as reliant on electricity and cabling as it is on oxygen and suction. The increasing age of the population needs also to be considered when designing an ED. Older patients have multiple co-morbidities leading to impaired mobility, vision and balance as well as being at increased risk of delirium due to underlying disease or hospitalization. They are likely to require greater space for the use of mobility aids and require greater shielding from sources of cognitive overstimulation than other patients. Standard hospital trolleys may pose a falls risk and contribute to the development of pressure areas. Strategies, such as the use of alternative hospital beds with pressure relieving mattresses and more comfortable ‘reclining lounge chair’ style seating, should be adopted for this subset of patients. Adequate lighting, the availability of natural lighting and the maintenance of a normal diurnal ‘night–day’ light pattern should be considered in the design to cater for the elderly patients who may spend prolonged periods of time in the emergency department. Diane King A primary role of the emergency department (ED) is to deliver the best possible care to all presenting patients. In order to deliver optimal care, a system of quality management must be part of the culture for all staff and be applied to all functions of the department. A quality framework provides the structure for the wide-ranging aspects of practice that are involved. Quality management requires effective leadership and commitment to improving processes and systems through analysis of data, change of processes and practice, staff engagement accountability and communication. Quality management is a continuous cycle, with measurement and monitoring required to establish that improvement is required in a practice or process, planning of the change, implementation, with re-evaluation and monitoring to ensure the change has the desired effect. Consumer involvement is a fundamental part of quality management. In the emergency setting, consumers include patients, families and carers, staff and the other clinical and hospital staff who interface with the ED. The traditional approach of quality assurance involves a number of retrospective attempts to police various activities of the ED. The types of tools used in this approach are pathology result checking, missed fractures, medical record reviews, death audits and patient complaints. The role of quality improvement in healthcare has evolved from the 1990s as it became evident that healthcare is prone to significant error and that, despite medical advances and escalating costs, the delivery of safe, acceptable and effective care is frequently lacking. Most industries adopted the quality improvement model to improve safety, reliability and efficiency. The implementation in the healthcare environment is noteworthy for the complexity of its systems, difficulty measuring clinical outcomes and competing priorities [1]. A modern quality system provides a framework that includes monitoring, audit and improvement of the clinical aspects of care, processes and structure, competence of staff, including education and training, and has clear governance and accountability [2]. The Deming cycle (described by WE Deming) is a fundamental tool for the approach to quality in any system. The PDSA (plan, do, study, act) cycle should incorporate the important sequential steps of planning, staff engagement, implementation, measurement, re-measurement and re-evaluation, followed by an improved plan and so on. A QI system covers a number of dimensions. These are variously described, but include: There are a number of vital characteristics of a CQI programme that are necessary for its successful operation. A CQI programme: A more detailed outline of TQM is beyond the scope of this book, however, the recent literature abounds with discussion on the various tools used, pitfalls in introduction and so on [5–8]. The quality agenda has been facilitated by various bodies, including The Australian Council on Healthcare Standards (ACHS), that, in 1997, introduced its Evaluation and Quality Improvement Programme (EQuIP) as a framework for hospitals to establish quality processes. This is a requirement for accreditation with the ACHS. In 2006, the Australian Commission for Safety and Quality of Health Care was established to oversee improvements in the Australian context (previously the Australian Council for Safety and Quality). In the USA, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the Institute for Healthcare Improvement have led the way in the move from QA to QI [9,10]. The Australasian College for Emergency Medicine, the American College of Emergency Physicians and the UK College of Emergency Medicine are facilitating the process of QI by their training role, introduction of clinical indicators, policy development and standards for EDs. In addition, the International Federation for Emergency Medicine (IFEM) has developed a consensus document outlining a framework for measuring quality in 2012 available on the IFEM website. The ED is a complex environment, which involves close interaction with the rest of the hospital and the community. The inputs are uncontrollable and unregulated and the ‘customers’ are under a high level of stress because of the nature of their problems, the unfamiliarity of the environment and the lack of control they perceive at a time when they are feeling personally vulnerable. The ED is dealing simultaneously with life-threatening illness and minor complaints. It is an area under a high level of scrutiny from all quarters: the patients, the families and friends, the other departments in the hospital and the wider community–both medical and non-medical. This in itself is error prone and is compounded by the fact that many of the staff working in the ED are rotating through the department for relatively short periods of time, are often relatively junior and are undergoing training themselves. This training role is of critical importance in most EDs and must not be forgotten in any process dealing with quality issues. All these aspects of an ED make the maintenance of quality difficult and all the more imperative. In order to establish a system where quality care can be delivered with any degree of reliability, it is important that all staff are committed to the process and that management provides appropriate leadership and resources. The delivery of quality involves a continuing process of data collection (performance measures), analysis, feedback and introduction of strategies to improve the system, followed by re-analysis of the performance measures (the quality cycle). The following are not exhaustive but are commonly used measures:
Administration
27.1 Emergency department staffing
General principles
Estimating medical workload
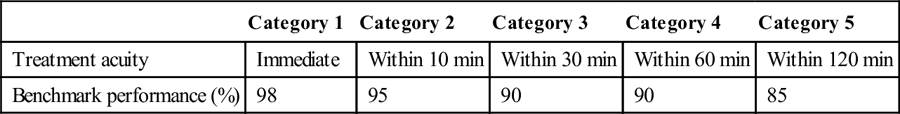
 The workforce should be resourced and organized so that patients are treated within the benchmark times for their clinical acuity (triage category). The Australasian College for Emergency Medicine (ACEM) has defined benchmarks for waiting time by triage category (Table 27.1.2) [2].
The workforce should be resourced and organized so that patients are treated within the benchmark times for their clinical acuity (triage category). The Australasian College for Emergency Medicine (ACEM) has defined benchmarks for waiting time by triage category (Table 27.1.2) [2].
Category 1
Category 2
Category 3
Category 4
Category 5
Treatment acuity
Immediate
Within 10 min
Within 30 min
Within 60 min
Within 120 min
Benchmark performance (%)
98
95
90
90
85
NTS category
Medical time (min)
Category 1
160
Category 2
80
Category 3
60
Category 4
40
Category 5
20
Structure of medical staff
 consultants (specialist emergency physicians), including a medical director
consultants (specialist emergency physicians), including a medical director
 registrars (specialist trainees)
registrars (specialist trainees)
 senior non-specialist staff: experienced hospital medical officers
senior non-specialist staff: experienced hospital medical officers
Estimating nursing workload
Nurse staffing structure
Allied health, clerical and other support staff
Optimizing work practices
27.2 Emergency department layout
Introduction
Design considerations
Resuscitation
Acute treatment
Specialty plaster/procedure
Consultation room
Oxygen outlets
3
2
2
1
Medical air outlets
2
1
1
–
Suction outlets
3
2
1
1
Nitrous oxide
1
1
1
–
Scavenging unit
1
1
1
–
Power outlets
16
8
8
4
Size and composition of the emergency department
Clinical areas
Individual treatment areas
Resuscitation area
Acute treatment area
Single rooms
Acute mental health area
Consultation area
Plaster room
Procedure room
Staff station
Short-stay unit
Medical assessment and planning unit
Clinical support areas
Non-clinical areas
Waiting area
Reception/triage area
Reception/clerical office
Tutorial room
Telemedicine area
Offices
Staff facilities
Likely developments over the next 5–10 years
27.3 Quality assurance/quality improvement
Introduction
History
Definitions
 Quality–‘doing those things necessary to meet the needs and reasonable expectations of those we service and doing those things right every time’ [3].
Quality–‘doing those things necessary to meet the needs and reasonable expectations of those we service and doing those things right every time’ [3].
 Quality assurance (QA)–‘a system used to establish standards for patient care, to monitor how well standards of care are met, and to correct unwarranted deviations from the standards’ [4]. This implies intervention to correct deficiencies and is often externally driven.
Quality assurance (QA)–‘a system used to establish standards for patient care, to monitor how well standards of care are met, and to correct unwarranted deviations from the standards’ [4]. This implies intervention to correct deficiencies and is often externally driven.
 Quality improvement (QI)–raising quality performance to ever increasing levels.
Quality improvement (QI)–raising quality performance to ever increasing levels.
Continuous quality improvement
 access and equity, e.g. waiting times and access to inpatient beds
access and equity, e.g. waiting times and access to inpatient beds
 acceptability or patient centredness, e.g. complaint rates, patient satisfaction surveys
acceptability or patient centredness, e.g. complaint rates, patient satisfaction surveys
 efficiency: cost-effectiveness and value, e.g. appropriate imaging, avoiding waste.
efficiency: cost-effectiveness and value, e.g. appropriate imaging, avoiding waste.
 requires leadership (management) commitment and strategic planning
requires leadership (management) commitment and strategic planning
 focuses around clear governance structures and accountability
focuses around clear governance structures and accountability
 has effective communication and change management
has effective communication and change management
National bodies
Quality in the ED
Common quality measures in ED
 time to thrombolysis or percutaneous coronary intervention (PCI)
time to thrombolysis or percutaneous coronary intervention (PCI)
 waiting time by triage category
waiting time by triage category
 death audits–and morbidity or adverse event reviews
death audits–and morbidity or adverse event reviews
 flow measures: 4 hour total ED times, times to inpatient bed
flow measures: 4 hour total ED times, times to inpatient bed
 chart audits for specific complaints, e.g. management of headache, abdominal pain, etc.
chart audits for specific complaints, e.g. management of headache, abdominal pain, etc.
 time to analgesia: generally and for specific conditions, such as abdominal pain or fractures
time to analgesia: generally and for specific conditions, such as abdominal pain or fractures
 time to antibiotic for sentinel diagnoses, such as febrile neutropaenia or pneumonia
time to antibiotic for sentinel diagnoses, such as febrile neutropaenia or pneumonia
 trauma audits–missed cervical fractures, delay in craniotomy
trauma audits–missed cervical fractures, delay in craniotomy
 X-ray and pathology report follow up
X-ray and pathology report follow up
 equipment functioning and supply
equipment functioning and supply
 safety of the working environment including, for example, electrical safety or violent incidents
safety of the working environment including, for example, electrical safety or violent incidents
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


27. Administration
Only gold members can continue reading. Log In or Register to continue



































