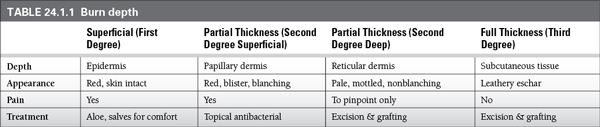
Burn depth: burn depth is dependent on the specific heat of the causative agent and the length of exposure.
 Wounds may evolve in the first 24 to 72 hours post injury, and the initial assessment of burn depth may be inaccurate.
Wounds may evolve in the first 24 to 72 hours post injury, and the initial assessment of burn depth may be inaccurate.
 First-degree burns affect only the epidermis.
First-degree burns affect only the epidermis.
 The area is erythematous and the skin remains intact.
The area is erythematous and the skin remains intact.
 Partial thickness burns (second degree) are divided into superficial and deep, based on the level of dermal injury.
Partial thickness burns (second degree) are divided into superficial and deep, based on the level of dermal injury.
 Superficial partial thickness burns extend into the papillary dermis, and are erythematous and blistered in appearance.
Superficial partial thickness burns extend into the papillary dermis, and are erythematous and blistered in appearance.
 Deep second partial thickness burns extend into the reticular dermis.
Deep second partial thickness burns extend into the reticular dermis.
 These wounds appear mottled and nonblanching and can lead to significant scar and contracture formation.
These wounds appear mottled and nonblanching and can lead to significant scar and contracture formation.
 Full-thickness burns (third degree) involve all layers of the epidermis and dermis, and sometimes deeper into the subcutaneous tissue.
Full-thickness burns (third degree) involve all layers of the epidermis and dermis, and sometimes deeper into the subcutaneous tissue.
 Unless very small (<5 cm), full-thickness burns require excision and skin grafting (See Table 24.1.1).
Unless very small (<5 cm), full-thickness burns require excision and skin grafting (See Table 24.1.1).
 Burn size: burn size is calculated using the rule of nines (see Figure 24.1.1).
Burn size: burn size is calculated using the rule of nines (see Figure 24.1.1).
 The circumferential upper extremities are each 9% total body surface area (TBSA).
The circumferential upper extremities are each 9% total body surface area (TBSA).
 The circumferential lower extremities are each 18% TBSA.
The circumferential lower extremities are each 18% TBSA.
 The anterior torso and posterior torso each represent 18% TBSA.
The anterior torso and posterior torso each represent 18% TBSA.
 The head and neck are 9% TBSA
The head and neck are 9% TBSA
 The genitalia is 1% TBSA
The genitalia is 1% TBSA
 For smaller burns, and those in a scattered distribution, size is estimated by visualizing the patient’s open hand, which is equal to 1% TBSA.
For smaller burns, and those in a scattered distribution, size is estimated by visualizing the patient’s open hand, which is equal to 1% TBSA.
 In children, the head contributes to a larger area, while the legs represent less body surface area.
In children, the head contributes to a larger area, while the legs represent less body surface area.
Common Causes to Remember
 Heat/Thermal
Heat/Thermal
 Electrical
Electrical
 Chemical
Chemical
Epidemiology
 Each year in the United States, burn injury results in 500,000 emergency department visits and 60,000 hospital admissions.
Each year in the United States, burn injury results in 500,000 emergency department visits and 60,000 hospital admissions.
 House fires are responsible for 1.2 per 100,000 deaths.
House fires are responsible for 1.2 per 100,000 deaths.
 Two-thirds of all burns occur in the home with scald burns being the most common.
Two-thirds of all burns occur in the home with scald burns being the most common.
 Globally, both the incidence and mortality of burn injury are higher.
Globally, both the incidence and mortality of burn injury are higher.
 House fires are responsible for 5.8 per 100,000 deaths in developing nations.
House fires are responsible for 5.8 per 100,000 deaths in developing nations.
 Risk factors for burn injury include:
Risk factors for burn injury include:
 Low socioeconomic status
Low socioeconomic status
 Drug and alcohol abuse
Drug and alcohol abuse
 Disability
Disability
 Homelessness
Homelessness
 Age extremes
Age extremes
 Burn injury ranks as the fourth leading cause of child injury-related death.
Burn injury ranks as the fourth leading cause of child injury-related death.
 The pediatric and geriatric populations are potential victims of nonaccidental burn injury and all suspected cases of abuse or neglect should be thoroughly investigated.
The pediatric and geriatric populations are potential victims of nonaccidental burn injury and all suspected cases of abuse or neglect should be thoroughly investigated.
Management and Treatment
 The initial approach to the burn patient follows the same primary survey used in trauma.
The initial approach to the burn patient follows the same primary survey used in trauma.
 The establishment of an airway is the first priority!
The establishment of an airway is the first priority!
 All patients with impaired mental status or those in respiratory distress should be promptly intubated.
All patients with impaired mental status or those in respiratory distress should be promptly intubated.
 Patients with deep burns to the head and neck and those with suspected inhalation injury should also be intubated early before tissue swelling obstructs the airway.
Patients with deep burns to the head and neck and those with suspected inhalation injury should also be intubated early before tissue swelling obstructs the airway.
 Large TBSA burns require large volumes of fluid that can lead to significant interstitial edema and intubation is warranted when large volume resuscitation is anticipated.
Large TBSA burns require large volumes of fluid that can lead to significant interstitial edema and intubation is warranted when large volume resuscitation is anticipated.
 After an airway is obtained, breathing and ventilation must be assessed.
After an airway is obtained, breathing and ventilation must be assessed.
 Circumferential burns to the torso may require escharotomy to allow for proper chest expansion.
Circumferential burns to the torso may require escharotomy to allow for proper chest expansion.
 Carbon monoxide toxicity must also be considered in patients with presumed inhalation injury and is treated with 100% inhaled oxygen.
Carbon monoxide toxicity must also be considered in patients with presumed inhalation injury and is treated with 100% inhaled oxygen.
 Reliable IV access must be established, either in the form of two large-bore peripheral lines (14 to 16 gauge) or a central venous catheter.
Reliable IV access must be established, either in the form of two large-bore peripheral lines (14 to 16 gauge) or a central venous catheter.
 If necessary, access can be placed through burned skin.
If necessary, access can be placed through burned skin.
 Arterial catheterization is also recommended for larger-sized burns and in patients with significant comorbidities.
Arterial catheterization is also recommended for larger-sized burns and in patients with significant comorbidities.
 The Parkland formula (wt [kg] × % TBSA × 2 to 4 mL) is used to calculate fluid requirement for burns larger than 20% TBSA.
The Parkland formula (wt [kg] × % TBSA × 2 to 4 mL) is used to calculate fluid requirement for burns larger than 20% TBSA.
 Half of the calculated volume is given as an hourly rate over the first 8 hours; the second half is infused over the next 16 hours.
Half of the calculated volume is given as an hourly rate over the first 8 hours; the second half is infused over the next 16 hours.
 Time delays and fluids given en route must also be taken into account.
Time delays and fluids given en route must also be taken into account.
 For example, consider the case of a 70-kg female who presents one hour following 40% TBSA flame injury. She was given 2 L of crystalloid en route:
For example, consider the case of a 70-kg female who presents one hour following 40% TBSA flame injury. She was given 2 L of crystalloid en route:
 70 kg × 40% TBSA × 4 mL = 11.2 L in first 24 hours
70 kg × 40% TBSA × 4 mL = 11.2 L in first 24 hours
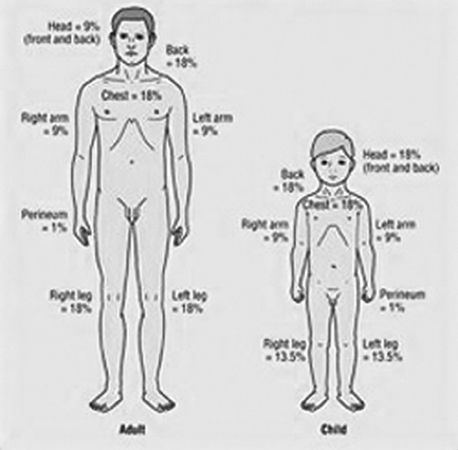
Figure 24.1.1 Rule of nines.
 Divide 11.2 L by two = 5.6 L first 8 hours, 5.6 L next 16 hours
Divide 11.2 L by two = 5.6 L first 8 hours, 5.6 L next 16 hours
 Subtract fluids given and time passed: 5.6 L – 2 L = 3.6 L/7 h = 514 mL/h over first 7 hours
Subtract fluids given and time passed: 5.6 L – 2 L = 3.6 L/7 h = 514 mL/h over first 7 hours
 Second half of fluid given over 16 hours = 5.6 L/16 h = 350 mL/h over remaining 16 hours
Second half of fluid given over 16 hours = 5.6 L/16 h = 350 mL/h over remaining 16 hours
 Ringer lactate solution is the crystalloid of choice for most patients; children less than 2 years of age should have 5% dextrose added to the solution.
Ringer lactate solution is the crystalloid of choice for most patients; children less than 2 years of age should have 5% dextrose added to the solution.
 Fluid boluses are not typically utilized in the burn patient unless the mean arterial pressure is less than 60 mmHg.
Fluid boluses are not typically utilized in the burn patient unless the mean arterial pressure is less than 60 mmHg.
 The bolus should be followed by a 10% increase in the hourly fluid rate.
The bolus should be followed by a 10% increase in the hourly fluid rate.
 Once resuscitation is complete, the crystalloid rate can be slowly decreased by 10% per hour.
Once resuscitation is complete, the crystalloid rate can be slowly decreased by 10% per hour.
 The use of albumin in first 24 hours post injury is controversial and most burn surgeons do not advocate routine use until the capillary leak is resolved.
The use of albumin in first 24 hours post injury is controversial and most burn surgeons do not advocate routine use until the capillary leak is resolved.
 Resuscitation Parameters
Resuscitation Parameters
 An indwelling Foley catheter should be placed in all burns greater than 20% TBSA.
An indwelling Foley catheter should be placed in all burns greater than 20% TBSA.
 Fluids should be closely monitored with a goal urine output of 0.5 mL/kg/h in adults and 1 to 2 mL/kg/h in children.
Fluids should be closely monitored with a goal urine output of 0.5 mL/kg/h in adults and 1 to 2 mL/kg/h in children.
 A number of laboratory parameters are also helpful in guiding resuscitation. These include:
A number of laboratory parameters are also helpful in guiding resuscitation. These include:
 base excess/deficit
base excess/deficit
 serum lactate
serum lactate
 bicarbonate
bicarbonate
 venous oxygen saturation
venous oxygen saturation
 Overly aggressive fluid resuscitation can have deleterious effects on the burn patient and are associated with high mortality rates. These include:
Overly aggressive fluid resuscitation can have deleterious effects on the burn patient and are associated with high mortality rates. These include:
 pulmonary edema
pulmonary edema
 congestive heart failure
congestive heart failure
 abdominal compartment syndrome
abdominal compartment syndrome
 ocular compartment syndrome
ocular compartment syndrome
 If the patient is not resuscitating appropriately, consideration should be given to instituting advanced hemodynamic monitoring.
If the patient is not resuscitating appropriately, consideration should be given to instituting advanced hemodynamic monitoring.
 Wound Management: the goals of burn wound care are to provide comfort, a moist environment, and to minimize the risk of infection.
Wound Management: the goals of burn wound care are to provide comfort, a moist environment, and to minimize the risk of infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree