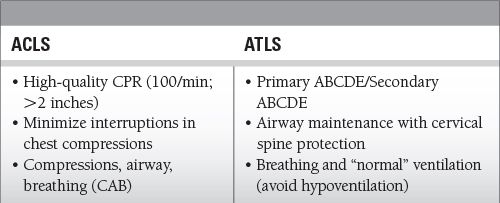
High-quality CPR with adequate rate (100/min) and depth (2 inches)
 Minimize interruptions in chest compressions
Minimize interruptions in chest compressions
 Avoid excessive ventilation
Avoid excessive ventilation
 Treat most significant injury first
Treat most significant injury first
 Expose patient, but prevent hypothermia
Expose patient, but prevent hypothermia
 Early and successful treatment during ACLS/ATLS protocols starts with effective leadership by code team leader
Early and successful treatment during ACLS/ATLS protocols starts with effective leadership by code team leader
Common Themes to Remember
Epidemiology
 Leading cause of death overall is diseases of the heart—598,607 people annually
Leading cause of death overall is diseases of the heart—598,607 people annually
 Leading cause of death from ages 1 to 44 years is accidents (unintentional injuries)—117,176 people annually
Leading cause of death from ages 1 to 44 years is accidents (unintentional injuries)—117,176 people annually
 Trauma is the leading cause of mortality globally
Trauma is the leading cause of mortality globally
Key Pathophysiology
 ACLS: 5 Hs and 5 Ts (discussed in detail below)
ACLS: 5 Hs and 5 Ts (discussed in detail below)
 ATLS: identify life-threatening injuries and treat
ATLS: identify life-threatening injuries and treat
2010 ACLS Guidelines
 Key changes from the 2005 ACLS Guidelines
Key changes from the 2005 ACLS Guidelines
 Capnography for confirming and monitoring ETT placement
Capnography for confirming and monitoring ETT placement
 Importance of high-quality CPR (adequate rate 100/min and depth > 2 inches)
Importance of high-quality CPR (adequate rate 100/min and depth > 2 inches)
 Atropine is no longer recommended for use in pulseless electrical activity (PEA) or asystole.
Atropine is no longer recommended for use in pulseless electrical activity (PEA) or asystole.
 Chronotropic drug infusions as an alternative to pacing in symptomatic and unstable bradycardia.
Chronotropic drug infusions as an alternative to pacing in symptomatic and unstable bradycardia.
 Adenosine is recommended as a safe and potentially effective therapy in the initial management of stable undifferentiated regular monomorphic wide-complex tachycardia.
Adenosine is recommended as a safe and potentially effective therapy in the initial management of stable undifferentiated regular monomorphic wide-complex tachycardia.
 Consider activating emergency response system
Consider activating emergency response system
 Airway and ventilation
Airway and ventilation
 Every second without CPR means a lack of cardiac and cerebral perfusion
Every second without CPR means a lack of cardiac and cerebral perfusion
 The mainstay of ACLS starts with effective CPR consisting of adequate depth (≥2 inches [5 cm]) and rate (100/min) of compressions allowing complete recoil; rotate compressor every 2 minutes.
The mainstay of ACLS starts with effective CPR consisting of adequate depth (≥2 inches [5 cm]) and rate (100/min) of compressions allowing complete recoil; rotate compressor every 2 minutes.
 Advanced airway placement in cardiac arrest should not delay initial CPR and defibrillation for ventricular fibrillation (VF) cardiac arrest.
Advanced airway placement in cardiac arrest should not delay initial CPR and defibrillation for ventricular fibrillation (VF) cardiac arrest.
 Securing the airway should be done by experienced providers, using their “best” method first—ideally done in <10 seconds.
Securing the airway should be done by experienced providers, using their “best” method first—ideally done in <10 seconds.
 Indications for emergency endotracheal intubation are inability to ventilate with bag and mask and the absence of airway protective reflexes.
Indications for emergency endotracheal intubation are inability to ventilate with bag and mask and the absence of airway protective reflexes.
 Use of 100% inspired oxygen during CPR optimizes arterial oxyhemoglobin content and thus oxygen delivery.
Use of 100% inspired oxygen during CPR optimizes arterial oxyhemoglobin content and thus oxygen delivery.
 Continuous waveform capnography is recommended in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an ETT.
Continuous waveform capnography is recommended in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an ETT.
 Breath sounds should not be heard over the epigastrium.
Breath sounds should not be heard over the epigastrium.
 Compression: ventilation ratio of 30:2 (if no advanced airway)
Compression: ventilation ratio of 30:2 (if no advanced airway)
 Deliver 1 breath every 6 to 8 seconds (if advanced airway is present)
Deliver 1 breath every 6 to 8 seconds (if advanced airway is present)
 Management of cardiac arrest
Management of cardiac arrest
 Shout for help/activate emergency response
Shout for help/activate emergency response
 Start CPR
Start CPR
 Cardiac arrest rhythms: VF, pulseless ventricular tachycardia (VT), PEA, and asystole
Cardiac arrest rhythms: VF, pulseless ventricular tachycardia (VT), PEA, and asystole
 Both BLS and ACLS with integrated postcardiac arrest care
Both BLS and ACLS with integrated postcardiac arrest care
 High-quality CPR for all cardiac arrest rhythms is of fundamental importance —>2 inches for depth and >100/min for rate
High-quality CPR for all cardiac arrest rhythms is of fundamental importance —>2 inches for depth and >100/min for rate
 Only rhythm-specific therapy proven to increase survival to hospital discharge is defibrillation of VF/pulseless VT
Only rhythm-specific therapy proven to increase survival to hospital discharge is defibrillation of VF/pulseless VT
 Diagnose and treat the 5 Hs and 5 Ts
Diagnose and treat the 5 Hs and 5 Ts
 5 Hs
5 Hs
 Hypoxia
Hypoxia
 Hypovolemia
Hypovolemia
 Hydrogen ion (acidosis)
Hydrogen ion (acidosis)
 Hypokalemia/Hyperkalemia
Hypokalemia/Hyperkalemia
 Hypothermia
Hypothermia
 5 Ts
5 Ts
 Toxins
Toxins
 Tamponade (cardiac)
Tamponade (cardiac)
 Tension pneumothorax
Tension pneumothorax
 Thrombosis, pulmonary
Thrombosis, pulmonary
 Thrombosis, coronary
Thrombosis, coronary
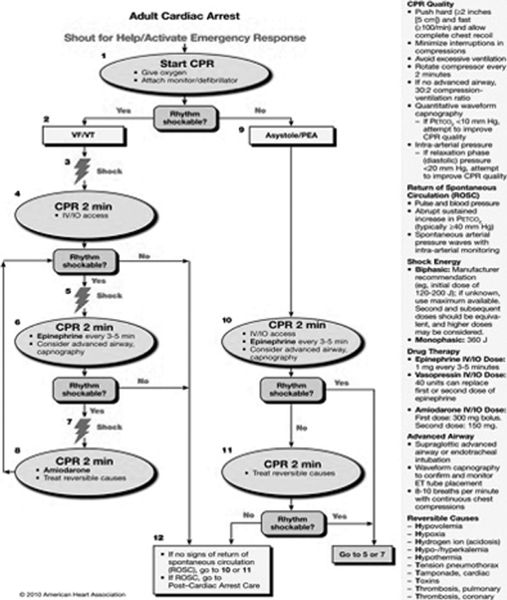
 VF (disorganized electrical activity) or pulseless VT (organized electric activity of the ventricular myocardium)
VF (disorganized electrical activity) or pulseless VT (organized electric activity of the ventricular myocardium)
 If rhythm check by an automated external defibrillator, manual defibrillator, or a provider identifies VF or pulseless VT a single shock should be delivered.
If rhythm check by an automated external defibrillator, manual defibrillator, or a provider identifies VF or pulseless VT a single shock should be delivered.
 Biphasic defibrillation: use initial energy dose of 120 to 200 J
Biphasic defibrillation: use initial energy dose of 120 to 200 J
 Monophasic defibrillation: use initial energy dose of 360 J
Monophasic defibrillation: use initial energy dose of 360 J
 After initial shock, resume CPR immediately for 2 minutes before the next rhythm check.
After initial shock, resume CPR immediately for 2 minutes before the next rhythm check.
 If VF or pulseless VT persists after at least one shock and a cycle of CPR, epinephrine 1 mg or vasopressin 40 units may be given.
If VF or pulseless VT persists after at least one shock and a cycle of CPR, epinephrine 1 mg or vasopressin 40 units may be given.
 Amiodarone 300 mg bolus for first dose and 150 mg for second dose may be given if VF/VT is refractory to above treatments.
Amiodarone 300 mg bolus for first dose and 150 mg for second dose may be given if VF/VT is refractory to above treatments.
 If amiodarone is unavailable, lidocaine may be considered.
If amiodarone is unavailable, lidocaine may be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


