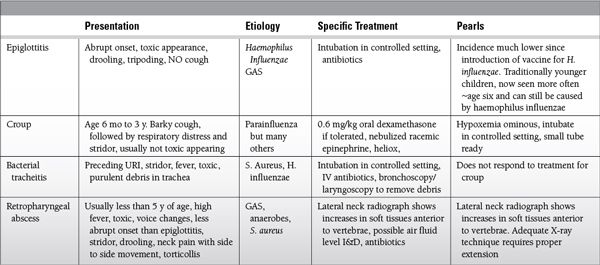
Bacterial infection leading to swollen epiglottis with risk for airway obstruction
 Much less common since introduction of conjugate vaccine against Haemophilus influenzae type B (HIB)
Much less common since introduction of conjugate vaccine against Haemophilus influenzae type B (HIB)
 Since HIB vaccine, cause more likely to be group A streptococcus (GAS) and seen in children older than 6 years
Since HIB vaccine, cause more likely to be group A streptococcus (GAS) and seen in children older than 6 years
 Ten percent of epiglottitis cases still caused by H. influenzae even in vaccinated.
Ten percent of epiglottitis cases still caused by H. influenzae even in vaccinated.
 Presentation: abrupt onset, stridor, tripoding, drooling, fever, toxic appearing, muffled voice, NO cough, thumbprint sign on lateral neck x-ray
Presentation: abrupt onset, stridor, tripoding, drooling, fever, toxic appearing, muffled voice, NO cough, thumbprint sign on lateral neck x-ray
 Management: keep child calm preferably in caregiver’s arms, intubation in controlled setting, IV antibiotics
Management: keep child calm preferably in caregiver’s arms, intubation in controlled setting, IV antibiotics
Croup (Laryngotracheobronchitis)
 Viral infection causing subglottic edema
Viral infection causing subglottic edema
 Most common in children 6 months to 3 years of age
Most common in children 6 months to 3 years of age
 Parainfluenza, but can be caused by many different viruses
Parainfluenza, but can be caused by many different viruses
 Presentation: barky cough, followed by respiratory distress and stridor, usually not toxic appearing
Presentation: barky cough, followed by respiratory distress and stridor, usually not toxic appearing
 Management: one dose of 0.6 mg/kg of oral dexamethasone if able, otherwise parenteral; nebulized racemic epinephrine if stridor at rest, heliox to improve laminar flow
Management: one dose of 0.6 mg/kg of oral dexamethasone if able, otherwise parenteral; nebulized racemic epinephrine if stridor at rest, heliox to improve laminar flow
 Desaturation is an ominous sign and consideration should be given to intubation in a controlled setting with several smaller sized endotracheal tubes (ETT) available in anticipation of a swollen airway.
Desaturation is an ominous sign and consideration should be given to intubation in a controlled setting with several smaller sized endotracheal tubes (ETT) available in anticipation of a swollen airway.
Bacterial Tracheitis
 Bacterial superinfection of trachea usually in setting of viral URI
Bacterial superinfection of trachea usually in setting of viral URI
 Staphylococcus aureus or HIB (usually in unvaccinated patients)
Staphylococcus aureus or HIB (usually in unvaccinated patients)
 Presentation
Presentation
 Preceding upper respiratory infection (URI), stridor, cough, fever, toxic appearing, copious sputum, and purulent debris in trachea
Preceding upper respiratory infection (URI), stridor, cough, fever, toxic appearing, copious sputum, and purulent debris in trachea
 Less abrupt onset than epiglottitis, more systemically ill than croup
Less abrupt onset than epiglottitis, more systemically ill than croup
 NOT responsive to treatments for croup
NOT responsive to treatments for croup
 Management: intubation in controlled setting, IV antibiotics, bronchoscopy/laryngoscopy to remove debris
Management: intubation in controlled setting, IV antibiotics, bronchoscopy/laryngoscopy to remove debris
 Consider pediatric otolaryngology consultation once intubated
Consider pediatric otolaryngology consultation once intubated
 Clear trachea and ETT of debris frequently to minimize chances of obstruction
Clear trachea and ETT of debris frequently to minimize chances of obstruction
Retropharyngeal and Lateral Pharyngeal Abscess
 Bacterial infection filling potential space of the posterior wall of esophagus and anterior border of cervical vertebrae
Bacterial infection filling potential space of the posterior wall of esophagus and anterior border of cervical vertebrae
 GAS, anaerobes, S. aureus
GAS, anaerobes, S. aureus
 Usually younger than 5 years of age (space obliterated in older)
Usually younger than 5 years of age (space obliterated in older)
 Presentation: stridor, drooling, neck pain with side to side movement, torticollis, high fever, toxic, voice changes, less abrupt onset than epiglottitis; lateral neck radiograph shows increases in soft tissues anterior to vertebrae, possible air fluid level; ensure proper extension on plain radiographs, nasopharyngitis with development of high fever, dysphagia, severe throat pain, noisy breathing, and stiff neck. Lower incidence of respiratory distress and stridor compared to epiglottitis and bacterial tracheitis, need for immediate intubation rare; infants under 1 year of age may present with fever, drooling, and stridor or, with isolated fever and lethargy.
Presentation: stridor, drooling, neck pain with side to side movement, torticollis, high fever, toxic, voice changes, less abrupt onset than epiglottitis; lateral neck radiograph shows increases in soft tissues anterior to vertebrae, possible air fluid level; ensure proper extension on plain radiographs, nasopharyngitis with development of high fever, dysphagia, severe throat pain, noisy breathing, and stiff neck. Lower incidence of respiratory distress and stridor compared to epiglottitis and bacterial tracheitis, need for immediate intubation rare; infants under 1 year of age may present with fever, drooling, and stridor or, with isolated fever and lethargy.
 Management: IV antibiotics, pediatric otolaryngology consultation, incision and drainage (I&D)
Management: IV antibiotics, pediatric otolaryngology consultation, incision and drainage (I&D)
 Lateral pharyngeal abscess less common, requires CT for diagnosis
Lateral pharyngeal abscess less common, requires CT for diagnosis
Peritonsillar Abscess
 Purulent material in peritonsillar fossa, GAS, S. aureus, trismus, and voice changes, drooling, uvular deviation, tonsillar asymmetry, the treatment is incision and drainage (I&D) and antibiotics
Purulent material in peritonsillar fossa, GAS, S. aureus, trismus, and voice changes, drooling, uvular deviation, tonsillar asymmetry, the treatment is incision and drainage (I&D) and antibiotics
Bronchiolitis
 Usually caused by respiratory syncytial virus in winter and early spring
Usually caused by respiratory syncytial virus in winter and early spring
 Upper airway secretions, lower airway inflammation and debris
Upper airway secretions, lower airway inflammation and debris
 Mostly supportive care with oxygen, hydration, pulmonary toilet, CPAP, BiPAP, intubation if needed. Many respond to noninvasive positive pressure ventilation.
Mostly supportive care with oxygen, hydration, pulmonary toilet, CPAP, BiPAP, intubation if needed. Many respond to noninvasive positive pressure ventilation.
 Many wheeze with bronchiolitis; B2 agonists helpful in only a minority, use only if clinical improvement after first dose.
Many wheeze with bronchiolitis; B2 agonists helpful in only a minority, use only if clinical improvement after first dose.
 Hypertonic saline nebulizations have shown some benefit, though can cause bronchospasm in those with underlying reactive airway disease.
Hypertonic saline nebulizations have shown some benefit, though can cause bronchospasm in those with underlying reactive airway disease.
 Steroids do not improve outcomes.
Steroids do not improve outcomes.
Foreign Body Aspiration
 Peak 6 months to 4 years of age
Peak 6 months to 4 years of age
 Drooling dysphagia, stridor without fever, cough, unilateral wheeze, decreased breath sounds
Drooling dysphagia, stridor without fever, cough, unilateral wheeze, decreased breath sounds
 History of coughing or choking
History of coughing or choking
 Foreign body not radiopaque, but secondary signs on x-ray: unilateral difference in aeration, air trapping, atelectasis
Foreign body not radiopaque, but secondary signs on x-ray: unilateral difference in aeration, air trapping, atelectasis
 Airway fluoroscopy, bronchoscopy
Airway fluoroscopy, bronchoscopy
 If child can cough and talk, allow them to remain in a position of comfort and provide supplemental oxygen
If child can cough and talk, allow them to remain in a position of comfort and provide supplemental oxygen
 Consider delaying interventions that might cause agitation and worsen airway resistance
Consider delaying interventions that might cause agitation and worsen airway resistance
 Do not try to remove foreign bodies causing severe partial upper airway obstruction
Do not try to remove foreign bodies causing severe partial upper airway obstruction
SUGGESTED READINGS
ATLS: Advanced Trauma Life Support for Doctors. ATLS Student Course Manual. 8th ed. 2008.
Chameides L, Samson RA, Schexnayder, SM, Hazinski, MF. eds. Pediatric Advanced Life Support Provider Manual. American Heart Association Inc.; 2011.
Cote CJ, Ryan JF, Goudsouzian NG. A Practice of Anesthesia for Infants and Children. 3rd ed. Philadelphia, PA: WB Saunders; 2000.
D’Agostino J. Pediatric airway nightmares. Emerg Med Clin N Am. 2010;28(1):119-126.
Eicher DJ, Wagner CL, Katikaneni LP, et al. Moderate hypothermia in neonatal encephalopathy: safety outcomes. Pediatr Neurol. 2005;32(1): 18-24.
Harper, MB, Fleisher, GR. Infectious disease emergencies. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010:303-322.
Hopkins A, Lahiri T, Salerno R, Heath B. Changing epidemiology of life-threatening upper airway infections: the reemergence of bacterial tracheitis. Pediatrics. 2006;118(4):1418-1421.
Kim KS. Acute bacterial meningitis in Infants and Children. Lancet Infect Dis. 2010;10:32-42.
Pickering LJ, ed. Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Section 3, pp204-735. American Academy of Pediatrics; 2009.
Schunk JE. Foreign body-ingestion/aspiration. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine, 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010:276-282.
Shargorodsky J, Whittemore KR, Lee GS. Bacterial tracheitis: a therapeutic approach. Laryngoscope. 2010;120(12):2498-2501.
Vassallo SA, Baboolal HA. Anesthesia for pediatric surgery. In: Dunn PF, ed. Clinical Anesthesia Procedures of the Massachusetts General Hospital. 7th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2007:515-539.
21.2
Surgical Emergencies
Phoebe Yager and Robert A. Finkelstein
Surgical Emergencies
Omphalocele
 Abdominal contents herniate through umbilicus (usually bowel, possibly liver)
Abdominal contents herniate through umbilicus (usually bowel, possibly liver)
 Supraumbilical portions outside abdominal wall covered by peritoneum and amniotic sac
Supraumbilical portions outside abdominal wall covered by peritoneum and amniotic sac
 Caused by defect in folding of embryonic disc
Caused by defect in folding of embryonic disc
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


