The primary focus in the management of shock is to identify its origin and treat accordingly.
 There are several forms of shock as described in other chapters; this chapter will focus primarily on fluid resuscitation and transfusion in trauma, which is primarily related to hemorrhagic or hypovolemic shock.
There are several forms of shock as described in other chapters; this chapter will focus primarily on fluid resuscitation and transfusion in trauma, which is primarily related to hemorrhagic or hypovolemic shock.
 Resuscitation is not a surrogate for, and should not delay, definitive hemorrhage control.
Resuscitation is not a surrogate for, and should not delay, definitive hemorrhage control.
 The technique of resuscitating hypovolemic or hemorrhagic shock patients can have a major impact on outcomes.
The technique of resuscitating hypovolemic or hemorrhagic shock patients can have a major impact on outcomes.
Epidemiology of Shock in Trauma
 Approximately 5% of the trauma patients present in severe shock to the emergency department
Approximately 5% of the trauma patients present in severe shock to the emergency department
 The most common etiology of shock in the trauma setting is hemorrhage, which should be assumed until complete elucidation of the etiology.
The most common etiology of shock in the trauma setting is hemorrhage, which should be assumed until complete elucidation of the etiology.
 Shock accounts for between 20% and 40% of all mortality in trauma
Shock accounts for between 20% and 40% of all mortality in trauma
 Other causes of shock in trauma: neurogenic shock, cardiogenic (obstructive) shock, or a profound systemic inflammatory response from a large burden of traumatic injury
Other causes of shock in trauma: neurogenic shock, cardiogenic (obstructive) shock, or a profound systemic inflammatory response from a large burden of traumatic injury
Diagnosis of Shock and Resuscitation Monitoring
 Shock is a state of inadequate tissue perfusion due to the imbalance of oxygen delivery and the tissues’ needs.
Shock is a state of inadequate tissue perfusion due to the imbalance of oxygen delivery and the tissues’ needs.
 Depending on the severity of shock, different organs may be more or less affected, giving rise to different symptoms, with marked cardiac and brain-related symptoms only noted with severe cases.
Depending on the severity of shock, different organs may be more or less affected, giving rise to different symptoms, with marked cardiac and brain-related symptoms only noted with severe cases.
 Various cardiovascular and neuroendocrine compensating responses—tachycardia, vasoconstriction—take place after the initial shock insult, and the damage of this state may be either through a direct mechanism or through one of these unchecked compensatory responses.
Various cardiovascular and neuroendocrine compensating responses—tachycardia, vasoconstriction—take place after the initial shock insult, and the damage of this state may be either through a direct mechanism or through one of these unchecked compensatory responses.
 Hypotension and tachycardia are not sensitive parameters to diagnose shock, as 25% of those in shock will have a normal heart rate or blood pressure (BP). When present, hypotension and tachycardia may represent profound disarray of the circulatory system.
Hypotension and tachycardia are not sensitive parameters to diagnose shock, as 25% of those in shock will have a normal heart rate or blood pressure (BP). When present, hypotension and tachycardia may represent profound disarray of the circulatory system.
 The use of pulmonary artery catheters (PACs) may have some benefit among severely injured elderly patients; however, this requires further study.
The use of pulmonary artery catheters (PACs) may have some benefit among severely injured elderly patients; however, this requires further study.
 In an undifferentiated population of trauma patients in shock, there is no improvement in mortality with the use of PACs to achieve supranormal resuscitation endpoints.
In an undifferentiated population of trauma patients in shock, there is no improvement in mortality with the use of PACs to achieve supranormal resuscitation endpoints.
 Abnormal levels of arterial pH, bicarbonate, base deficit, and lactic acid suggest inadequate tissue perfusion and the persistence of abnormal values correlate with worse outcomes. Hence, these seem to be better markers of shock than standard vital signs, but have the drawback of taking longer to be assessed.
Abnormal levels of arterial pH, bicarbonate, base deficit, and lactic acid suggest inadequate tissue perfusion and the persistence of abnormal values correlate with worse outcomes. Hence, these seem to be better markers of shock than standard vital signs, but have the drawback of taking longer to be assessed.
Hypotensive Resuscitation (Permissive Hypotension)
 “Hypotensive resuscitation” refers to the concept of limiting fluid resuscitation to the minimum required to maintain organ function until the underlying cause of the hypotension (usually hemorrhage) has been addressed. Resuscitation is targeted to avoid complete hemodynamic collapse, rather than to normalize BP.
“Hypotensive resuscitation” refers to the concept of limiting fluid resuscitation to the minimum required to maintain organ function until the underlying cause of the hypotension (usually hemorrhage) has been addressed. Resuscitation is targeted to avoid complete hemodynamic collapse, rather than to normalize BP.
 Restricting resuscitation to lower BP goals has been shown to be beneficial in various animal studies.
Restricting resuscitation to lower BP goals has been shown to be beneficial in various animal studies.
 The use of delayed fluid resuscitation in penetrating torso injuries is supported by level I data in humans.
The use of delayed fluid resuscitation in penetrating torso injuries is supported by level I data in humans.
 Reducing the goal BP and the amount of fluid administered during resuscitation leads to lower rates of acute respiratory distress syndrome (ARDS), abdominal compartment syndrome, blood loss, and improved inflammatory profiles.
Reducing the goal BP and the amount of fluid administered during resuscitation leads to lower rates of acute respiratory distress syndrome (ARDS), abdominal compartment syndrome, blood loss, and improved inflammatory profiles.
 The use of lower goals of BP during resuscitation has gained greater attention in different study populations, but has yet to be proved superior for all mechanisms of trauma.
The use of lower goals of BP during resuscitation has gained greater attention in different study populations, but has yet to be proved superior for all mechanisms of trauma.
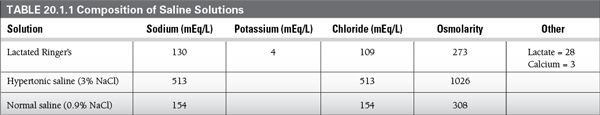
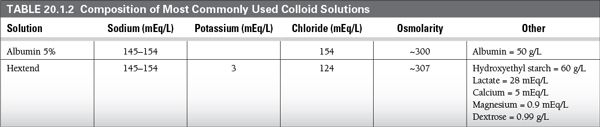
Fluid Choices (See TABLE 20.1.1 and TABLE 20.1.2)
 Crystalloids
Crystalloids
 Crystalloids are the recommended initial resuscitation fluid by the Advanced Trauma Life Support curriculum.
Crystalloids are the recommended initial resuscitation fluid by the Advanced Trauma Life Support curriculum.
 Lactated Ringer’s solution is the preferred initial fluid for trauma patients due to lower risk of hyperchloremic metabolic acidosis when compared with normal saline.
Lactated Ringer’s solution is the preferred initial fluid for trauma patients due to lower risk of hyperchloremic metabolic acidosis when compared with normal saline.
 The administration of large volumes of crystalloids may have deleterious effects such as dilutional coagulopathy, ARDS, and increased abdominal pressure.
The administration of large volumes of crystalloids may have deleterious effects such as dilutional coagulopathy, ARDS, and increased abdominal pressure.
 Over-resuscitation with crystalloids has attributable morbidity.
Over-resuscitation with crystalloids has attributable morbidity.
 Crystalloids should be considered like any other medications with indications, side effects, adverse effects, and contraindications.
Crystalloids should be considered like any other medications with indications, side effects, adverse effects, and contraindications.
 Hypertonic saline
Hypertonic saline
 The use of 3 to 7.5% saline has been studied in trauma patients requiring resuscitation. There is no compelling evidence to support the use of hypertonic saline for routine resuscitation.
The use of 3 to 7.5% saline has been studied in trauma patients requiring resuscitation. There is no compelling evidence to support the use of hypertonic saline for routine resuscitation.
 The theoretical advantage is mobilization of fluid from cells to intravascular and interstitial spaces, without a significant increase in total water content.
The theoretical advantage is mobilization of fluid from cells to intravascular and interstitial spaces, without a significant increase in total water content.
 The slower rate of third space redistribution of hypertonic solutions allows resuscitation with smaller amounts of fluids.
The slower rate of third space redistribution of hypertonic solutions allows resuscitation with smaller amounts of fluids.
 Excluding the routine use of hypertonic saline, much higher concentrations of NaCl, such as 23.4%, are effective measures to control intracranial pressure in patients with traumatic brain injury.
Excluding the routine use of hypertonic saline, much higher concentrations of NaCl, such as 23.4%, are effective measures to control intracranial pressure in patients with traumatic brain injury.
 Colloids
Colloids
 The protein content of colloid solutions allows them to remain in the intravascular space and generate an oncotic pressure that shifts fluid from cells to the intravascular compartment.
The protein content of colloid solutions allows them to remain in the intravascular space and generate an oncotic pressure that shifts fluid from cells to the intravascular compartment.
 Colloids may improve microvascular perfusion, but are much more expensive than crystalloids, and have been implicated in a variety of damaging immunological effects.
Colloids may improve microvascular perfusion, but are much more expensive than crystalloids, and have been implicated in a variety of damaging immunological effects.
 Synthetic colloids have also been associated with coagulopathy in high doses.
Synthetic colloids have also been associated with coagulopathy in high doses.
 Dextran has been implicated in lethal cases of anaphylaxis, pulmonary edema, and platelet dysfunction, as well as renal damage.
Dextran has been implicated in lethal cases of anaphylaxis, pulmonary edema, and platelet dysfunction, as well as renal damage.
 Several trials and metanalyses over the last 10 years have demonstrated no difference in outcomes of critically ill patients comparing crystalloid versus colloid resuscitation.
Several trials and metanalyses over the last 10 years have demonstrated no difference in outcomes of critically ill patients comparing crystalloid versus colloid resuscitation.
 Blood products
Blood products
 Blood products are replacing crystalloids in the early resuscitation of the hemorrhaging patient.
Blood products are replacing crystalloids in the early resuscitation of the hemorrhaging patient.
 Blood products can re-establish the coagulation system in the bleeding patient. The drawbacks include the cost, and the risk of transfusion reactions and transmission of blood-borne pathogens.
Blood products can re-establish the coagulation system in the bleeding patient. The drawbacks include the cost, and the risk of transfusion reactions and transmission of blood-borne pathogens.
 Usually, blood product resuscitation is initiated with the administration of packed red blood cells (PRBCs). Rapid availability of such components is usually achieved through the use of type O PRBCs to the hemorrhaging patients until type-specific and cross-matched units are available.
Usually, blood product resuscitation is initiated with the administration of packed red blood cells (PRBCs). Rapid availability of such components is usually achieved through the use of type O PRBCs to the hemorrhaging patients until type-specific and cross-matched units are available.
 Massive transfusion has been historically defined as the transfusion of ten or more units of RBCs in less than 24 hours. Massive transfusion protocols are now common in trauma centers to coordinate the release of blood products in a timely fashion to patients who will probably require massive transfusion, and to facilitate the communication between the blood bank and the trauma or critical care team.
Massive transfusion has been historically defined as the transfusion of ten or more units of RBCs in less than 24 hours. Massive transfusion protocols are now common in trauma centers to coordinate the release of blood products in a timely fashion to patients who will probably require massive transfusion, and to facilitate the communication between the blood bank and the trauma or critical care team.
 The use of fresh frozen plasma (FFP) has been recommended at an early phase to offset the coagulopathy that takes place in exsanguinating patients. When massive transfusion (>10 U PRBC) is anticipated, transfusion in a 1:1 to 1:2 ratio (FFP to PRBC) is recommended to prevent dilutional coagulopathy and has been associated with improved survival.
The use of fresh frozen plasma (FFP) has been recommended at an early phase to offset the coagulopathy that takes place in exsanguinating patients. When massive transfusion (>10 U PRBC) is anticipated, transfusion in a 1:1 to 1:2 ratio (FFP to PRBC) is recommended to prevent dilutional coagulopathy and has been associated with improved survival.
 Platelets should generally be transfused in a 1:1 to 1:2 ratio (PLT to PRBC) during massive transfusion
Platelets should generally be transfused in a 1:1 to 1:2 ratio (PLT to PRBC) during massive transfusion
 Essential parameters to be monitored during massive transfusion are hematocrit, platelet count, international normalized ratio (INR), activated prothrombin time (aPTT), and fibrinogen.
Essential parameters to be monitored during massive transfusion are hematocrit, platelet count, international normalized ratio (INR), activated prothrombin time (aPTT), and fibrinogen.
SUGGESTED READINGS
Ertmer C, Kampmeier T, Rehberg S, Lange M. Fluid resuscitation in multiple trauma patients. Curr Opin Anesthesiol. 2011;24:202-208.
Fouche Y, Sikorski R, Dutton RP. Changing paradigms in surgical resuscitation. Crit Care Med. 2010;38(Suppl 9):S411-S420.
Fukudome E, de Moya MA. Monitoring of the trauma patient. In: Cohn SM, ed. Acute Care Surgery and Trauma: Evidence-Based Practice. Informa Healthcare; 2009.
McSwain NE, Champion HR, Fabian TC, et al. Stat of the art of fluid resuscitation 2010: prehospital and immediate transition to the hospital. J Trauma. 2011;70(Suppl 5):S2-S10.
Santry HP, Alam HB. Fluid resuscitation: past, present, and the future. Shock. 2010;33(3):229-241.
Spoerke N, Michalek J, Schreiber M, and the Trauma Outcomes Group. Crystalloid resuscitation improves survival in trauma patients receiving low ratios of fresh frozen plasma to packed red blood cells. J Trauma. 2011;71(Suppl 2):S380-S383.
20.2
Basic Management
Dante Yeh
Epidemiology (in the United States)
 Trauma is the leading cause of death between ages 1 and 44.
Trauma is the leading cause of death between ages 1 and 44.
 Unintentional injury accounts for 28.4 million emergency department (ED) visits annually.
Unintentional injury accounts for 28.4 million emergency department (ED) visits annually.
 Blunt injury mechanism is more commonly encountered, with motor vehicle crashes being the predominant cause.
Blunt injury mechanism is more commonly encountered, with motor vehicle crashes being the predominant cause.
 Alcohol intoxication is the leading risk factor for injury (both intentional and unintentional).
Alcohol intoxication is the leading risk factor for injury (both intentional and unintentional).
Differential Diagnosis of Hypotension in the Trauma Patient
 Hypovolemic shock
Hypovolemic shock
 Hemorrhage is the most common etiology and must be ruled out first. Possible locations of hemorrhage include:
Hemorrhage is the most common etiology and must be ruled out first. Possible locations of hemorrhage include:
 Thorax, abdomen, pelvis/retroperitoneum, thigh, bony fractures, external (scene of the trauma)
Thorax, abdomen, pelvis/retroperitoneum, thigh, bony fractures, external (scene of the trauma)
 For most external bleeding, direct manual compression (an “educated finger”) is sufficient,
For most external bleeding, direct manual compression (an “educated finger”) is sufficient,
 Failing this, proximal tourniquet control is recommended until operative repair is achieved.
Failing this, proximal tourniquet control is recommended until operative repair is achieved.
 Intracranial injury is never the cause of hemorrhagic shock.
Intracranial injury is never the cause of hemorrhagic shock.
 In an unstable patient, pelvic binder is indicated only for open-book fractures to decrease pelvic volume and tamponade bleeding. For all other fractures (e.g., vertical shear or lateral compression), binding the pelvis is at best ineffectual and at worst harmful.
In an unstable patient, pelvic binder is indicated only for open-book fractures to decrease pelvic volume and tamponade bleeding. For all other fractures (e.g., vertical shear or lateral compression), binding the pelvis is at best ineffectual and at worst harmful.
 Obstructive shock—tension pneumothorax and cardiac tamponade
Obstructive shock—tension pneumothorax and cardiac tamponade
 Tension pneumothorax results in mediastinal shift which causes angulation of the superior vena cava (SVC) and inferior vena cava (IVC) and thereby limiting preload.
Tension pneumothorax results in mediastinal shift which causes angulation of the superior vena cava (SVC) and inferior vena cava (IVC) and thereby limiting preload.
 If clinically suspected, should be treated with immediate needle decompression followed by tube thoracostomy.
If clinically suspected, should be treated with immediate needle decompression followed by tube thoracostomy.
 Do NOT wait for chest X-ray diagnosis; the delay may be fatal.
Do NOT wait for chest X-ray diagnosis; the delay may be fatal.
 Cardiac tamponade limits diastolic filling and subsequent cardiac output,
Cardiac tamponade limits diastolic filling and subsequent cardiac output,
 Ultrasound of pericardium is highly accurate for the diagnosis,
Ultrasound of pericardium is highly accurate for the diagnosis,
 Unstable patients with cardiac tamponade require immediate ED resuscitative thoracotomy to relieve the tamponade.
Unstable patients with cardiac tamponade require immediate ED resuscitative thoracotomy to relieve the tamponade.
 Patients with traumatic pericardial effusion with normal vital signs may be transported to the operating room.
Patients with traumatic pericardial effusion with normal vital signs may be transported to the operating room.
 Neurogenic shock
Neurogenic shock
 Spinal cord injury above the T1 level results in sympathectomy and loss of vasomotor tone. In the euvolemic patient, hypotension is treated with vasopressors.
Spinal cord injury above the T1 level results in sympathectomy and loss of vasomotor tone. In the euvolemic patient, hypotension is treated with vasopressors.
 For incomplete blunt spinal cord injuries, the use of steroids is controversial and highly variable in clinical practice.
For incomplete blunt spinal cord injuries, the use of steroids is controversial and highly variable in clinical practice.
 For complete spinal cord injury and penetrating spinal cord injury, steroids are not indicated.
For complete spinal cord injury and penetrating spinal cord injury, steroids are not indicated.
 Cardiogenic shock
Cardiogenic shock
 In trauma patients with pre-existing cardiac disease or those suffering blunt cardiac injury, hypotension may result from cardiac failure. Treatment is supportive.
In trauma patients with pre-existing cardiac disease or those suffering blunt cardiac injury, hypotension may result from cardiac failure. Treatment is supportive.
Management and Treatment
 Airway
Airway
 Indications for post-traumatic intubation: inability to protect airway (GCS<8), extensive facial trauma, hypoxia/hypoventilation, impending airway compromise, combativeness (to facilitate radiologic evaluation)
Indications for post-traumatic intubation: inability to protect airway (GCS<8), extensive facial trauma, hypoxia/hypoventilation, impending airway compromise, combativeness (to facilitate radiologic evaluation)
 Rapid-sequence induction should be performed in all trauma patients requiring intubation.
Rapid-sequence induction should be performed in all trauma patients requiring intubation.
 The likelihood of an unstable cervical spine injury resulting from penetrating trauma is negligible; cervical immobilization is not required.
The likelihood of an unstable cervical spine injury resulting from penetrating trauma is negligible; cervical immobilization is not required.
 For blunt mechanism injury, the cervical collar may be removed for intubation with in-line stabilization provided.
For blunt mechanism injury, the cervical collar may be removed for intubation with in-line stabilization provided.
 Breathing
Breathing
 Asymmetric breath sounds may result from large pneumothorax and/or hemothorax.
Asymmetric breath sounds may result from large pneumothorax and/or hemothorax.
 In the stable patient, supine chest x-ray (CXR) and thoracic ultrasound may be used as adjuncts to the physical examination.
In the stable patient, supine chest x-ray (CXR) and thoracic ultrasound may be used as adjuncts to the physical examination.
 In an unstable patient with asymmetrical breath sounds, needle decompression (second intercostal space, mid-clavicular line) should be performed prior to intubation as positive pressure ventilation may result in further hemodynamic compromise.
In an unstable patient with asymmetrical breath sounds, needle decompression (second intercostal space, mid-clavicular line) should be performed prior to intubation as positive pressure ventilation may result in further hemodynamic compromise.
 Circulation
Circulation
 The ideal intravenous catheters for resuscitation are short and wide: large bore (14 g) peripheral access (at least two) or introducer (subclavian or femoral) is preferred.
The ideal intravenous catheters for resuscitation are short and wide: large bore (14 g) peripheral access (at least two) or introducer (subclavian or femoral) is preferred.
 Heart rate and blood pressure are insensitive and patients may be in shock with clinically “normal” vital signs.
Heart rate and blood pressure are insensitive and patients may be in shock with clinically “normal” vital signs.
 Serum lactate and base deficit can detect occult hypoperfusion.
Serum lactate and base deficit can detect occult hypoperfusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree