Epidemiology
 As of the end of 2011, over 23,000 lung transplants have been performed in the United States.
As of the end of 2011, over 23,000 lung transplants have been performed in the United States.
 Limiting factor is the availability of organs.
Limiting factor is the availability of organs.
 Compared to other organ transplants, long-term survival is worse than that of liver and kidney, but better than small bowel.
Compared to other organ transplants, long-term survival is worse than that of liver and kidney, but better than small bowel.
Key Pathophysiology
 Early mortality can be divided into
Early mortality can be divided into
 30 day mortality: 10 to 15%, related to the transplant procedure and immediate postoperative complications
30 day mortality: 10 to 15%, related to the transplant procedure and immediate postoperative complications
 1 year mortality: 30%; leading cause is infection from high-dose immunosuppression
1 year mortality: 30%; leading cause is infection from high-dose immunosuppression
 Recipients with certain preoperative diagnoses carry greater risks for specific complications
Recipients with certain preoperative diagnoses carry greater risks for specific complications
 CF patients are at higher risk of infection due to preoperative presence of infection.
CF patients are at higher risk of infection due to preoperative presence of infection.
 Complex congenital heart disease at higher risk for bleeding
Complex congenital heart disease at higher risk for bleeding
 Severe PHTN with single lung transplant at higher risk of severe ischemia-reperfusion injury and may require prolonged mechanical ventilation
Severe PHTN with single lung transplant at higher risk of severe ischemia-reperfusion injury and may require prolonged mechanical ventilation
 Recipients of older grafts with longer ischemia times at risk of early and late graft dysfunction
Recipients of older grafts with longer ischemia times at risk of early and late graft dysfunction
 Pulmonary denervation
Pulmonary denervation
 Bronchial hyper-responsiveness
Bronchial hyper-responsiveness
 Decreased inhalation cough response (despite intact laryngeal cough response)
Decreased inhalation cough response (despite intact laryngeal cough response)
 Denervation has been shown to have little effect on resting minute volume, tidal volume, respiratory rate, and breathing pattern.
Denervation has been shown to have little effect on resting minute volume, tidal volume, respiratory rate, and breathing pattern.
 Gas exchange
Gas exchange
 Hypoxic pulmonary vasoconstriction seems to remain intact in transplanted lungs.
Hypoxic pulmonary vasoconstriction seems to remain intact in transplanted lungs.
 Stunning of type 2 pneumocytes leads to decreased surfactant production immediately following transplantation, leading to increased risk of atelectasis.
Stunning of type 2 pneumocytes leads to decreased surfactant production immediately following transplantation, leading to increased risk of atelectasis.
 Loss of lymphatic drainage in the transplanted lung leads to increased risk of pulmonary edema.
Loss of lymphatic drainage in the transplanted lung leads to increased risk of pulmonary edema.
 8 weeks after successful transplantation, these factors tend to normalize.
8 weeks after successful transplantation, these factors tend to normalize.
 The pulmonary reimplantation response (PRR)/ischemia-reperfusion injury
The pulmonary reimplantation response (PRR)/ischemia-reperfusion injury
 Non-cardiogenic pulmonary edema in the immediate postoperative period, after ruling out rejection, infection, and cardiogenic causes
Non-cardiogenic pulmonary edema in the immediate postoperative period, after ruling out rejection, infection, and cardiogenic causes
 Ischemic vascular injury of the allograft results in increased permeability and interstitial and alveolar edema
Ischemic vascular injury of the allograft results in increased permeability and interstitial and alveolar edema
 Clinically results in hypoxemia with radiographic infiltrates
Clinically results in hypoxemia with radiographic infiltrates
 May also be associated with hypotension and decreased cardiac output
May also be associated with hypotension and decreased cardiac output
 Some studies report at least mild injury in up to 57% of recipients.
Some studies report at least mild injury in up to 57% of recipients.
 Associated with prolonged ischemia time
Associated with prolonged ischemia time
Differential Diagnosis
 30 day mortality
30 day mortality
 Graft failure (30%)
Graft failure (30%)
 Primary graft failure: most commonly attributed to ischemia-reperfusion injury; can lead to diffuse alveolar damage and death
Primary graft failure: most commonly attributed to ischemia-reperfusion injury; can lead to diffuse alveolar damage and death
 Nonspecific graft failure: diagnosis of exclusion when failure is either multifactorial in nature or not subject to postmortem confirmation
Nonspecific graft failure: diagnosis of exclusion when failure is either multifactorial in nature or not subject to postmortem confirmation
 Infection (23.5%)
Infection (23.5%)
 Cardiovascular (11.5%)
Cardiovascular (11.5%)
 Acute rejection (5%)
Acute rejection (5%)
 Any occurrence associated with higher mortality rate, length of hospitalization, and compromised recovery
Any occurrence associated with higher mortality rate, length of hospitalization, and compromised recovery
 1 year mortality
1 year mortality
 Infection (38.7%)
Infection (38.7%)
 Graft failure (17.5%)
Graft failure (17.5%)
 Lymphoma (3.3%): both infections and lymphoma are considered to be side effects of high-dose immunosuppression, required due to the high rate of rejection of lung grafts when compared with other organs
Lymphoma (3.3%): both infections and lymphoma are considered to be side effects of high-dose immunosuppression, required due to the high rate of rejection of lung grafts when compared with other organs
Management and Treatment
 Early postoperative care focuses on weaning from ventilator support, fluid management, immunosuppression, detection of early rejection, and prevention/treatment of infection
Early postoperative care focuses on weaning from ventilator support, fluid management, immunosuppression, detection of early rejection, and prevention/treatment of infection
 Generally, standard ventilation strategies suffice
Generally, standard ventilation strategies suffice
 Lung isolation is rarely indicated
Lung isolation is rarely indicated
 Positive End Expiratory Pressure (PEEP) is usually indicated, except in the case of single lung transplant for COPD (leads to overinflation of the more compliant, grafted lung)
Positive End Expiratory Pressure (PEEP) is usually indicated, except in the case of single lung transplant for COPD (leads to overinflation of the more compliant, grafted lung)
 Pulmonary HTN—lability in hemodynamics and oxygenation are to be expected; these patients may benefit from prolonged mechanical ventilation
Pulmonary HTN—lability in hemodynamics and oxygenation are to be expected; these patients may benefit from prolonged mechanical ventilation
 PRR—prolonged mechanical support and longer ICU stays
PRR—prolonged mechanical support and longer ICU stays
 Judicious fluid and hemodynamic management—graft is prone to edema due to increased vascular permeability and loss of lymphatic drainage; vasopressor and inotropic support is preferred over fluid resuscitation
Judicious fluid and hemodynamic management—graft is prone to edema due to increased vascular permeability and loss of lymphatic drainage; vasopressor and inotropic support is preferred over fluid resuscitation
 Treatment for PRR follows conventional paradigms for acute lung injury
Treatment for PRR follows conventional paradigms for acute lung injury
Outcomes
 PRR: no effect on 1 and 3 year survival
PRR: no effect on 1 and 3 year survival
 Double lung transplant half life is 4.9 to 7.9 years
Double lung transplant half life is 4.9 to 7.9 years
 Single lung transplant half life is 3.7 to 5.9 years
Single lung transplant half life is 3.7 to 5.9 years
 Most limiting factor to long-term survival is the occurrence of obliterative bronchiolitis and its clinical correlate, bronchiolitis obliterans syndrome, which portends chronic rejection
Most limiting factor to long-term survival is the occurrence of obliterative bronchiolitis and its clinical correlate, bronchiolitis obliterans syndrome, which portends chronic rejection
 Chronic morbidity associated with immunosuppression
Chronic morbidity associated with immunosuppression
 Calcineurin inhibitors: renal disease, hypertension, neurotoxicity
Calcineurin inhibitors: renal disease, hypertension, neurotoxicity
 Steroids: osteoporosis, adrenal suppression, weight gain
Steroids: osteoporosis, adrenal suppression, weight gain
Heart Transplantation
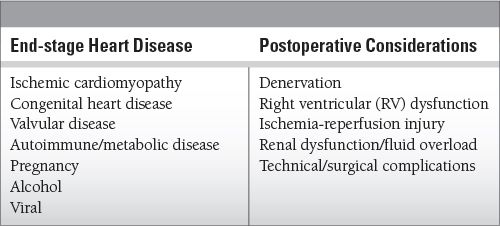
Common Causes to Remember
Epidemiology
 Heart transplantation has been in clinical use for the past 40 years, although early attempts resulted in high mortality due to lack of effective immunosuppression.
Heart transplantation has been in clinical use for the past 40 years, although early attempts resulted in high mortality due to lack of effective immunosuppression.
 As of the end of 2011, more than 50,000 hearts transplantation surgeries have been performed in the United States.
As of the end of 2011, more than 50,000 hearts transplantation surgeries have been performed in the United States.
Key Pathophysiology
 The denervated heart
The denervated heart
 Changes in heart rate are dependent upon circulating catecholamines
Changes in heart rate are dependent upon circulating catecholamines
 Reinnervation generally occurs within 1 year after transplant
Reinnervation generally occurs within 1 year after transplant
 Preoperative PHTN is a major risk factor for post-transplant acute RV failure. Contraindications for transplantation include:
Preoperative PHTN is a major risk factor for post-transplant acute RV failure. Contraindications for transplantation include:
 Pulmonary arterial systolic pressure greater than 50 to 60 mmHg
Pulmonary arterial systolic pressure greater than 50 to 60 mmHg
 Pulmonary vascular resistance (PVR) greater than 240 to 320 dynes-sec/cm5
Pulmonary vascular resistance (PVR) greater than 240 to 320 dynes-sec/cm5
 Transpulmonary gradient greater than 15 mmHg
Transpulmonary gradient greater than 15 mmHg
 Acute renal failure/oliguria
Acute renal failure/oliguria
 Frequently presents within the first 24 to 48 hours due to the effects of cardiopulmonary bypass and cyclosporine A initiation
Frequently presents within the first 24 to 48 hours due to the effects of cardiopulmonary bypass and cyclosporine A initiation
 Rejection
Rejection
 Majority of cases are subclinical
Majority of cases are subclinical
 Rarely, can manifest as arrhythmias, orthopnea, fever, or dyspnea
Rarely, can manifest as arrhythmias, orthopnea, fever, or dyspnea
 Only 5 to 10% of cases produce significant hemodynamic compromise
Only 5 to 10% of cases produce significant hemodynamic compromise
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


