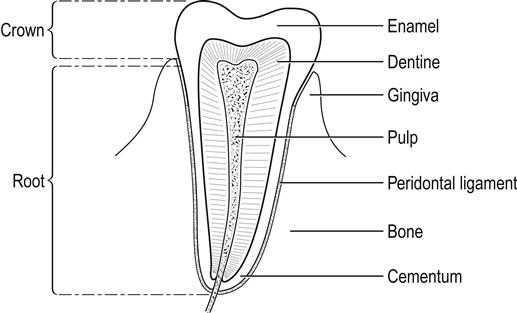
Edited by Peter Cameron Sashi Kumar The tooth consists of the crown, which is exposed, and the root, which lies within the socket covered by the gum and serves to anchor the tooth. The gingival pulp carries the neurovascular structures via the root canal and is covered by dentine which, in turn, is covered by enamel, the hardest substance in the body (Fig. 17.1.1). The deciduous teeth are 20 in number and erupt between the ages of 6 months and 2 years. The permanent dentition begins to erupt at around age 6 and, in the adult, consists of 32 teeth. The most common cause of toothache or odontalgia is caries. Dental caries-related emergencies account for up to 52% of first contact with a dentist for children below the age of 3 years [1]. Dental caries is the cause of emergency visits to a dentist in 73% of paediatric patients [2]. Pain associated with dental caries is of a dull, throbbing nature, localized to a specific area and aggravated by changes in temperature in the oral cavity (hypersensitivity to hot and cold food or fluids). Examination reveals tenderness of the offending tooth when tapped with a tongue depressor or a mirror. Management includes symptomatic pain relief using analgesics, such as paracetamol with or without codeine, non-steroidal anti-inflammatory drugs (NSAIDs) and urgent referral to the dentist. Pain is the most common cause of self-referral to the emergency department for dental problems. The common conditions causing dental pain are acute apical periodontitis and reversible and irreversible pulpitis resulting from dental caries [3]. Symptoms include painful swollen gums with or without halitosis. On occasions, frank pus or bleeding from the gums may be the presenting symptom. At all stages, varying degrees of pain associated with inflammation are invariably present [4]. Infected gums could be an early clinical sign of undiagnosed diabetes, HIV, graft-versus-host disease in radiation therapy for head and neck malignancy and bone marrow transplantation. Management includes diagnosis of the periodontal disease and the offending tooth. Symptomatic pain relief can be achieved with analgesics, NSAIDs and warm saline rinses. Routine antibiotic therapy is not required unless there is evidence of gross infection locally, regional lymphadenopathy or fever. In all cases, urgent review by the dentist is mandatory. Acute necrotizing ulcerative gingivitis (ANUG) is a severe form of gingivitis which could be related to stress and needs antibiotic cover and urgent referral to the dentist. Dry socket occurs between 2 and 5 days following dental extraction. The dull throbbing pain is due to the collection of necrotic clot and debris in the socket. The condition is diagnosed on the history and examination, which confirms the acutely tender extraction site. Treatment consists of irrigation of the extraction site to remove the necrotic material and packing the socket with sterile gauze soaked in local anaesthetic, such as cophenylcaine, followed by urgent dental review [5]. Bleeding from the socket post-extraction within 48 h is due to reactionary haemorrhage due to opening up of the small divided blood vessels. Bleeding after 5 days is secondary haemorrhage due to infection that destroys the organizing blood clot. General causes, such as hypertension and warfarin therapy, need to be addressed to control the bleeding. Management is essentially reassurance, careful suction to clear the debris and clot in the socket, followed by packing with gauze soaked in lignocaine with adrenaline or cophenylcaine and pressure. Dilute aminocaproic acid (IV Amicar) 5 mL in 10 mL of normal saline to rinse the mouth. Use Amicar or tranexamic acid-soaked gauze to bite on, applying direct pressure for about 30 min and repeat as required to control the bleeding. Occasionally, the gingival flaps may need to be sutured under local anaesthetic. Tooth avulsion is probably the most serious tooth injury. An avulsed tooth, if reimplanted in the socket within 30 min, has a 90% survival rate [6]. The mechanism of injury in such cases is usually either accidental sports-related facial injuries or assault. If the patient makes telephone contact with the emergency department, the patient is advised to locate the tooth because, even if the crown is broken, the root may be intact. The tooth should not be handled by the root to avoid damage to the periodontal ligament fibres; it is washed in running cold water and replaced in the socket. If this is not possible, place the tooth in the cheek or under the tongue and proceed immediately to the dentist. Do not scrub the tooth [7,8]. The best transportation medium for an avulsed tooth is saliva. Cold milk or iced salt water are suitable alternatives. If the patient arrives in the emergency department with the tooth, clean it by holding it by the crown in cold running water; any foreign debris should be removed with forceps. The tooth should not be allowed to dry. Following irrigation, the tooth should be placed in the socket as near the original position as possible and the patient referred to a dentist for stabilization with an archbar or orthodontic bands. If the reimplanted tooth remains mobile after 2 weeks, it should be extracted. The complications of reimplantation are ankylosis and loss of viability. The 2010 Dental Trauma Guide by the Danish Dental Association supported by the International Association of Dental Traumatology provides an interactive drop down menu on how to deal with every possible dental trauma [9]. Concussion is an injury to the tooth without displacement or mobility. Subluxation is when the tooth is mobile but not displaced. Periapical X-rays as baseline, soft diet for a week and local dentist follow up. Most common injury to upper primary incisors after a fall. If the crown is visible leave the tooth to re-erupt. If the whole tooth is intruded, extraction is required as it might affect the permanent dentition underneath. If there is excessive mobility or displacement, extraction is recommended. Avulsed primary teeth should not be replanted. Unless there is extensive soft-tissue damage, antibiotics are not required. The incidence of fractured teeth is reported to be 5 and 4.4 per 100 adults per year for all teeth and posterior teeth, respectively [10]. Based on the above statistics, it can be deduced that the likelihood of experiencing a fractured frontal/anterior tooth is about 1 in 20 in a given year in adults and 1 in 23 for posterior teeth. Traumatic injuries to the teeth have been classified as follows [11]: Class I: simple fracture of the enamel of the crown. Class II: extensive fracture of the crown involving dentine. Class III: extensive fracture of the crown involving dentine and dental pulp. Class IV: extensive involvement and exposure of the entire pulp. Class V: totally avulsed or luxated teeth. Class VI: fracture of the root with or without loss of crown structure. Class VII: displacement of tooth without fracture of crown or root. Class VIII: fracture of the crown in its entirety (Fig. 17.1.2).
Dental Emergencies
17.1 Dental emergencies
Anatomy
Dental caries
Periodontal emergencies
Alveolar osteitis (dry socket)
Postdental extraction bleeding
Traumatic dental emergencies
Management
Dentoalveolar trauma in children
Concussion and subluxation
Management
Intrusive luxation
Management
Extrusive and lateral subluxation
Avulsion
Dental fractures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree