Intravenous (IV) fluids are given for different purposes and should be prescribed with the same care and attention as drugs.
 IV fluids can cause red-cell destruction if the tonicity of the fluid leads to rapid changes in the water level in the red cell.
IV fluids can cause red-cell destruction if the tonicity of the fluid leads to rapid changes in the water level in the red cell.
 Hypotonic fluids are often given to replace insensible losses as a “maintenance fluid,” replace body water deficits or to supplement dextrose.
Hypotonic fluids are often given to replace insensible losses as a “maintenance fluid,” replace body water deficits or to supplement dextrose.
 Isotonic fluids are often given to resuscitate the intravascular and extracelluar spaces.
Isotonic fluids are often given to resuscitate the intravascular and extracelluar spaces.
 Hypertonic fluids are commonly given to treat intracranial hypertension, and some give hypertonic solutions for resuscitation after trauma; in the United States this is mostly done under experimental protocols.
Hypertonic fluids are commonly given to treat intracranial hypertension, and some give hypertonic solutions for resuscitation after trauma; in the United States this is mostly done under experimental protocols.
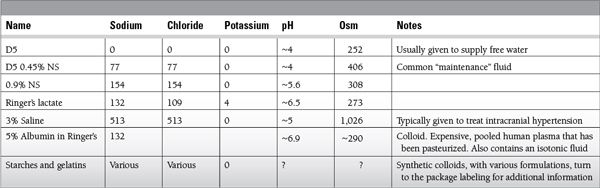
 Colloids can be manufactured volume expanders like starches, dextrans, and gelatins.
Colloids can be manufactured volume expanders like starches, dextrans, and gelatins.
 Human albumin is also a colloid but is a pooled, pasteurized blood product that can be used as a volume expander, or given to raise plasma oncotic pressure.
Human albumin is also a colloid but is a pooled, pasteurized blood product that can be used as a volume expander, or given to raise plasma oncotic pressure.
 Adult daily requirement for fluid depends on size and comorbid issues.
Adult daily requirement for fluid depends on size and comorbid issues.
 1 to 1.5 cc/kg/h is a commonly used guideline for adult maintenance fluid.
1 to 1.5 cc/kg/h is a commonly used guideline for adult maintenance fluid.
 Formulas for pediatric maintenance fluid are typically variants of the 4-2-1 rule.
Formulas for pediatric maintenance fluid are typically variants of the 4-2-1 rule.
 Fluid replacement of deficits and losses varies greatly with the etiology.
Fluid replacement of deficits and losses varies greatly with the etiology.
 Sepsis and many shock states respond to fluid therapy.
Sepsis and many shock states respond to fluid therapy.
 Burns and large open wound can create large fluid losses.
Burns and large open wound can create large fluid losses.
 Gastrointestinal losses of fluids, diarrhea, Naso-gastric (NG) suction, enterocutaneous fistulae can create large fluid losses, that require replacement.
Gastrointestinal losses of fluids, diarrhea, Naso-gastric (NG) suction, enterocutaneous fistulae can create large fluid losses, that require replacement.
 Inappropriate urine production as in diabetes insipidus, post-obstructive. Diuresis or the diuretic phase of acute tubular necrosis may also require large volume replacement
Inappropriate urine production as in diabetes insipidus, post-obstructive. Diuresis or the diuretic phase of acute tubular necrosis may also require large volume replacement
Epidemiology
 Almost every patient will receive some IV fluid, but patients with inability to take enteral fluids will be more reliant on IV therapy.
Almost every patient will receive some IV fluid, but patients with inability to take enteral fluids will be more reliant on IV therapy.
 Sepsis and trauma are the two common conditions where large volumes of IV fluids are given.
Sepsis and trauma are the two common conditions where large volumes of IV fluids are given.
 Pancreatitis and large surface area burns initially require large fluid resuscitation.
Pancreatitis and large surface area burns initially require large fluid resuscitation.
Management and Treatment
 Assessing volume status can be difficult but full use of physical examination with data from vital signs, physiologic monitors like the central venous pressure, and diagnostic tests like bedside ultrasound or Brain Natriuretic peptid (BNP) can be used to assess volume status and help to determine the need for fluid therapy.
Assessing volume status can be difficult but full use of physical examination with data from vital signs, physiologic monitors like the central venous pressure, and diagnostic tests like bedside ultrasound or Brain Natriuretic peptid (BNP) can be used to assess volume status and help to determine the need for fluid therapy.
 Consider the use of IV fluids to replace insensible as well as measurable fluid losses.
Consider the use of IV fluids to replace insensible as well as measurable fluid losses.
 Each degree Celsius of fever over 38 can raise the insensible water losses by 500 cc/d.
Each degree Celsius of fever over 38 can raise the insensible water losses by 500 cc/d.
 If a patient is hypovolemic, resuscitation with IV fluids to restore their circulating volume, will often, but not always, be beneficial.
If a patient is hypovolemic, resuscitation with IV fluids to restore their circulating volume, will often, but not always, be beneficial.
 Withhold IV fluid from patients with intravascular volume overload or decompensated congestive heart failure.
Withhold IV fluid from patients with intravascular volume overload or decompensated congestive heart failure.
Outcomes
 There are insufficient outcome data to guide the use of most IV fluids.
There are insufficient outcome data to guide the use of most IV fluids.
 The largest trial of relevance is the Saline versus Albumin Fluid Evaluation (SAFE) trial that compared albumin to normal saline, and found the two to be equivalent, but with important differences in some subgroups.
The largest trial of relevance is the Saline versus Albumin Fluid Evaluation (SAFE) trial that compared albumin to normal saline, and found the two to be equivalent, but with important differences in some subgroups.
 While hypovolemia can produce tissue ischemia and injury, we are learning that volume overload can be detrimental as well.
While hypovolemia can produce tissue ischemia and injury, we are learning that volume overload can be detrimental as well.
 IV fluids can lead to production of inflammatory mediators.
IV fluids can lead to production of inflammatory mediators.
 Hypertonic fluids produce an immunosuppressant effect.
Hypertonic fluids produce an immunosuppressant effect.
 Hydroxyethyl starches are associated with increased risk of renal failure and death in critically ill patients with sepsis.
Hydroxyethyl starches are associated with increased risk of renal failure and death in critically ill patients with sepsis.
 Albumin may be safe or even beneficial in septic patients.
Albumin may be safe or even beneficial in septic patients.
 The SAFE trial suggests that albumin worsens morbidity and mortality in patients with brain injury.
The SAFE trial suggests that albumin worsens morbidity and mortality in patients with brain injury.
 Some clinicians, including those behind the Lund model of managing the brain injured, however, continue to report improved outcome with the routine use of albumin solutions.
Some clinicians, including those behind the Lund model of managing the brain injured, however, continue to report improved outcome with the routine use of albumin solutions.
SUGGESTED READINGS
Finfer S, Norton R, Bellomo R, et al. The SAFE study: saline vs. albumin for fluid resuscitation in the critically ill. Vox Sang. 2004;87(Suppl 2): 123-131.
Grände PO. The Lund concept for the treatment of patients with severe traumatic brain injury. J Neurosurg Anesthesiol. 2011;23(4):358-362.
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.4 versus ringer’s acetate in severe sepsis. N Engl J Med 2012;367(2):124-34.
SAFE Study Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian Red Cross Blood Service, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874-884.
SAFE Study Investigators, Finfer S, McEvoy S, et al. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Med. 2011;37:86-96.
15.2
Sodium Balance
Jonathan Charnin
 Sodium is the most plentiful plasma ion, and is regulated in the range of 135 to 145 meq/L, and serum osmolarity is maintained between 275 and 290 mosmol/L.
Sodium is the most plentiful plasma ion, and is regulated in the range of 135 to 145 meq/L, and serum osmolarity is maintained between 275 and 290 mosmol/L.
 Calculated serum osmolarity is most closely related to two times the sodium concentration Osm = (2 [sodium] + [Glucose]/18 + [BUN]/2.8).
Calculated serum osmolarity is most closely related to two times the sodium concentration Osm = (2 [sodium] + [Glucose]/18 + [BUN]/2.8).
 Contributions from glucose and Blood Urea Nitrogen (BUN) are small in the absence of hyperglycemia or marked uremia
Contributions from glucose and Blood Urea Nitrogen (BUN) are small in the absence of hyperglycemia or marked uremia
 Derangements in sodium are commonly caused by changes in the amount of body water.
Derangements in sodium are commonly caused by changes in the amount of body water.
 Less commonly by low or high salt intake
Less commonly by low or high salt intake
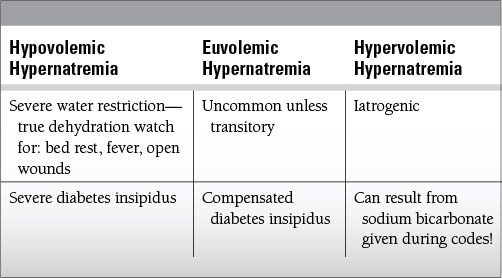
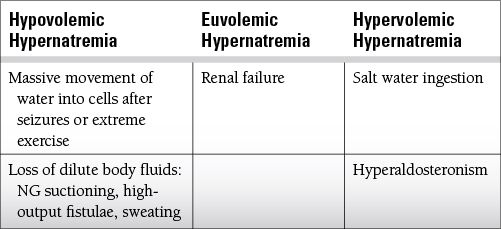
 A patient may be hypovolemic, euvolemic or hyponatremic with concurrent hypernatremia or concurrent hyponatremia, but the etiologies are usually distinct.
A patient may be hypovolemic, euvolemic or hyponatremic with concurrent hypernatremia or concurrent hyponatremia, but the etiologies are usually distinct.
 The history and physical examination provide clues to the etiology of the disturbance, and the crucial assessment of volume status.
The history and physical examination provide clues to the etiology of the disturbance, and the crucial assessment of volume status.
Common Causes to Remember
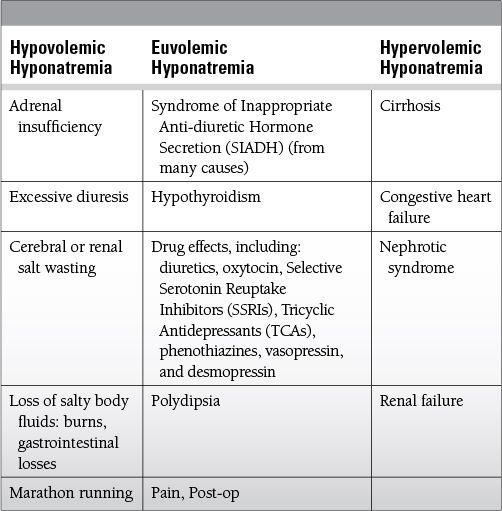
 Some common specific derangements
Some common specific derangements
 Iatrogenic hypernatremia—treatment of cerebral edema often involves hyperosmolar therapy
Iatrogenic hypernatremia—treatment of cerebral edema often involves hyperosmolar therapy
 In this setting hypertonic saline may be given to drive up the sodium, or mannitol may be given to pull water out of the intracellular space, leaving hypernatremia behind after the osmotic diuresis of mannitol.
In this setting hypertonic saline may be given to drive up the sodium, or mannitol may be given to pull water out of the intracellular space, leaving hypernatremia behind after the osmotic diuresis of mannitol.
 It should be cautioned, however, that mannitol can also cause a transient hyponatremia when administered rapidly.
It should be cautioned, however, that mannitol can also cause a transient hyponatremia when administered rapidly.
 Hypernatremia of water deficit—patients who lack the ability to satisfy their thirst may present with a hypernatremia from days without water intake.
Hypernatremia of water deficit—patients who lack the ability to satisfy their thirst may present with a hypernatremia from days without water intake.
 While circulating volume should be restored quickly, caution should be taken to avoid overly rapid correction of this hypernatremia.
While circulating volume should be restored quickly, caution should be taken to avoid overly rapid correction of this hypernatremia.
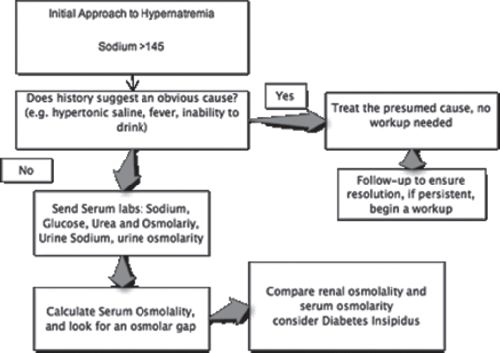
 Diabetes insipidus—causes filtration of plasma without water retention in the kidneys that commonly produces hypovolemic hypernatremia
Diabetes insipidus—causes filtration of plasma without water retention in the kidneys that commonly produces hypovolemic hypernatremia
 “Central” from lack of antidiuretic hormone (ADH) release from the pituitary
“Central” from lack of antidiuretic hormone (ADH) release from the pituitary
 “Nephrogenic” from dysfunction of the aquaporin channels in the kidney
“Nephrogenic” from dysfunction of the aquaporin channels in the kidney
 Adrenal insufficiency—produces concurrent hyponatremia and hyperkalemia, often with postural or overt hypotension
Adrenal insufficiency—produces concurrent hyponatremia and hyperkalemia, often with postural or overt hypotension
 Cerebral salt wasting—this state of relative or absolute hyponatremia looks like SIADH, but occurs in patients with brain injury who are thought to be hypovolemic (unlike true SIADH)
Cerebral salt wasting—this state of relative or absolute hyponatremia looks like SIADH, but occurs in patients with brain injury who are thought to be hypovolemic (unlike true SIADH)
 The generous urine production in brain injured patients can appear similar to diabetes insipidus (DI), but unlike DI, the urine osmolality will tend to be higher than the plasma osmolality.
The generous urine production in brain injured patients can appear similar to diabetes insipidus (DI), but unlike DI, the urine osmolality will tend to be higher than the plasma osmolality.
 SIADH—the syndrome of inappropriate ADH produces euvolemic hyponatremia, although the volume state can vary.
SIADH—the syndrome of inappropriate ADH produces euvolemic hyponatremia, although the volume state can vary.
 Some patients with this condition have inappropriate retention of water, without the hormone.
Some patients with this condition have inappropriate retention of water, without the hormone.
 Watch for normal urine osmolality in the setting of low serum osmolality and hyponatremia.
Watch for normal urine osmolality in the setting of low serum osmolality and hyponatremia.
 Hyperosmotic hyponatremia—seen with high plasma levels of sugars or other osmotically active non-electrolytes where hyperglycemia and high plasma mannitol levels are the most common.
Hyperosmotic hyponatremia—seen with high plasma levels of sugars or other osmotically active non-electrolytes where hyperglycemia and high plasma mannitol levels are the most common.
Epidemiology
 Hypernatremia is common in the critically ill who may have increased losses but lack the ability to satisfy their thirst.
Hypernatremia is common in the critically ill who may have increased losses but lack the ability to satisfy their thirst.
 Hypernatremia was reported in 9% of 981 intensive care unit (ICU) patients.
Hypernatremia was reported in 9% of 981 intensive care unit (ICU) patients.
 Mortality associated with hypernatremia may be higher than 40%, but this is because hypernatremia is a marker for more severe illness.
Mortality associated with hypernatremia may be higher than 40%, but this is because hypernatremia is a marker for more severe illness.
 Hypernatremia is more common among critically ill patients with brain injuries, often due to hypertonic saline use to control brain swelling.
Hypernatremia is more common among critically ill patients with brain injuries, often due to hypertonic saline use to control brain swelling.
 Hyponatremia is common in the critically ill, and is more common than hypernatremia, ranging from 13% to 15% on admission to the ICU depending on definition.
Hyponatremia is common in the critically ill, and is more common than hypernatremia, ranging from 13% to 15% on admission to the ICU depending on definition.
Key Pathophysiology
 Water moves freely into an out of cells, sodium is kept outside of cells by membrane ion pumps.
Water moves freely into an out of cells, sodium is kept outside of cells by membrane ion pumps.
 Hypernatremia is usually a result of inadequate water intake, but excess sodium intake can produce hypernatremia.
Hypernatremia is usually a result of inadequate water intake, but excess sodium intake can produce hypernatremia.
 Water excretion in the kidney is regulated in the distal tubule and collecting ducts.
Water excretion in the kidney is regulated in the distal tubule and collecting ducts.
 Inappropriate water retention is the most common cause of hyponatremia.
Inappropriate water retention is the most common cause of hyponatremia.
 Altered mental status is commonly seen with extremes of sodium levels.
Altered mental status is commonly seen with extremes of sodium levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree