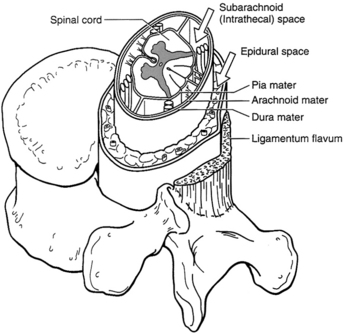
PROCEDURE 101 Epidural catheters are used to provide regional anesthesia and analgesia by delivering medications directly into the epidural space surrounding the spinal cord. Medications injected into the epidural space are capable of providing dose-related site-specific anesthesia and analgesia. Epidural catheters can be used effectively for short-term (e.g., acute, obstetric, postoperative, trauma) or long-term (e.g., chronic, advanced cancer) pain management.7,20 • State boards of nursing may have detailed guidelines involving epidural analgesia. Each institution that provides this therapy also has policies and guidelines pertaining to epidural therapy. It is important that the nurse is aware of state guidelines and institution policies. • The nurse must have an understanding of the principles of aseptic technique.13,22,23,27 • The epidural catheter placement and the continuing pain management of the patient should be under the supervision of an anesthesiologist, nurse anesthetist, or acute pain service to ensure positive patient outcomes.2,12 • The spinal cord and brain are covered by three membranes, collectively called the meninges. The outer layer is the dura mater. The middle layer is the arachnoid mater, which lies just below the dura mater and, with the dura, forms the dural sac. The innermost layer is the pia mater, which adheres to the surface of the spinal cord and the brain. The cerebrospinal fluid (CSF) circulates in the subarachnoid space, which is also called the intrathecal space.29 • The epidural space lies between the dura mater and the bone and ligaments of the spinal canal (Fig. 101-1). • The epidural space (potential space) contains fat, large blood vessels, connective tissue, and spinal nerve roots. • Analgesia via an epidural catheter may be given with a continuous, intermittent, or patient-controlled epidural analgesia (PCEA) pump system.17,29 • A variety of medication options are available, including local anesthetics, opiates, mixtures of local anesthetics and opiates, α2-adrenergic agonists (e.g., clonidine), and other agents.13,17 All medications should be preservative-free for epidural administration.4,7,12,13 • The pharmacology of agents given for epidural analgesia, including side effects and duration of action, must be understood.22 • Knowledge of the signs and symptoms of profound motor and sensory blockade or overmedication is essential. Intravenous (IV) access, IV volume loading, and immediate availability of an opioid antagonist and vasopressors are necessary.4,12,22 • According to the American Pain Society (APS), the most common reason for unrelieved pain in hospitals is the failure of staff to routinely and adequately assess pain and pain relief. Many patients silently tolerate unrelieved pain if not specifically asked about it.1 • The Agency for Health Care Policy and Research (AHCPR) urges healthcare professionals to accept the patient’s self-report as “the single most reliable indicator of the existence and intensity” of pain. Behavioral observations are unreliable indicators of pain levels.1 • Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1,7 • No matter how successfully or deftly conducted, surgical operations produce tissue trauma. Trauma caused by surgery or injury initiates a series of biochemical events that release numerous endogenous chemicals, which potentiate mediators of inflammation and pain.16 • Pain is just one response to the trauma of surgery. In addition to pain, the substances released from injured tissue evoke stress hormone responses in the patient. Such responses promote pain transmission, breakdown of body tissues, increased metabolic rate, blood clotting, water retention, and impaired immune function and trigger a fight-or-flight alarm reaction with autonomic nervous system stimulation features (e.g., rapid pulse).1,4,13 • The psychologic effects of pain include depression, anxiety, and other negative emotions.1,6,7 • The patient may attempt to “splint” the injured site, resulting in shallow breathing and cough suppression followed by retained pulmonary secretions and pneumonia.12,13 Unrelieved pain also may delay the return of normal gastric emptying and cause development of an ileus, impairment of bowel function, and reductions in respiratory tidal volumes, all of which may predispose patients in pain to infection after surgery.7,8,19,30 • Epidural analgesia provides a number of well-documented advantages in the postoperative period, including attenuation of the surgical/trauma stress response, excellent analgesia, earlier extubation, less sedation, decreased incidence of pulmonary complications, earlier return of bowel function, decreased deep venous thrombosis, earlier ambulation, earlier discharge from high-acuity units,12,14,20,30 and possibly shorter hospital stays.20,32 • One epidural catheter kit or the following supplies: • One introducer stabilizing catheter guide • One screw-cap Luer-Lok catheter • One screw-cap Luer-Lok catheter connector • One 0.2 × m epidural flat filter • Topical skin antiseptic, as prescribed (e.g., 2% chlorhexidine non–alcohol-based preparation) • Sterile gloves, face masks with eye shields, sterile gowns • 20 mL normal saline solution • 5 to 10 mL local anesthetic as prescribed (e.g., 1% lidocaine; local infiltration) • 5 mL local anesthetic as prescribed to establish the block • Test dose (e.g., 3 mL 2% lidocaine with epinephrine, 1:200,000)
Epidural Catheters: Assisting with Insertion and Pain Management
PREREQUISITE NURSING KNOWLEDGE
EQUIPMENT
 One 25-gauge, ⅝-inch (0.5 × 16 mm) injection needle
One 25-gauge, ⅝-inch (0.5 × 16 mm) injection needle
 One 23-gauge, 1¼-inch (0.6 × 30 mm) injection needle
One 23-gauge, 1¼-inch (0.6 × 30 mm) injection needle
 One 18-gauge, 1½-inch (1.2 × 40 mm) injection needle
One 18-gauge, 1½-inch (1.2 × 40 mm) injection needle
 One Luer-Lok loss-of-resistance syringe
One Luer-Lok loss-of-resistance syringe
 One 18-gauge, 3¼-inch (1.3 × 80 mm) epidural needle (pink)
One 18-gauge, 3¼-inch (1.3 × 80 mm) epidural needle (pink)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


101: Epidural Catheters: Assisting with Insertion and Pain Management