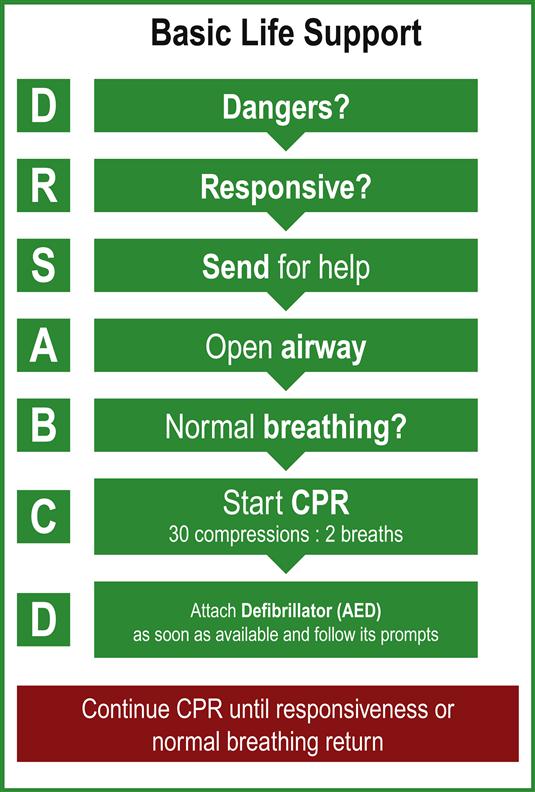
Edited by Anthony Brown Stephen A Bernard and Sameer Pathan Basic Life Support (BLS) aims to maintain respirations and circulation in the cardiac arrest victim. BLS involves a major focus on cardiopulmonary resuscitation (CPR) with minimal use of ancillary equipment. It includes chest compressions with or without rescue breathing and defibrillation with a manual or semiautomated external defibrillator (SAED). BLS can be successfully performed immediately by any rescuer with little or no training and, in the out-of-hospital cardiac arrest (OHCA), BLS has proven value in the survival of neurologically intact victims [1–3]. This chapter outlines an approach to BLS that can be delivered by any rescuer, while awaiting the arrival of emergency medical services (EMS) or medical expertise able to provide Advanced Life Support (ALS) (see Chapter 1.2). The series of linked actions for a victim of sudden cardiac arrest is known as the ‘Chain of Survival’ [4]. The first steps are early recognition of those at risk of or in active cardiac arrest and an immediate call to activate help from the emergency medical services. This is followed by early commencement of CPR with an emphasis on chest compressions and rapid defibrillation, which significantly improves the chances of survival from ventricular fibrillation (VF) in OHCA [1–3]. Cardiopulmonary resuscitation plus defibrillation within 3–5 min of collapse following VF in OHCA can produce survival rates as high as 49–75% [5–7]. Each minute of delay before defibrillation reduces the probability of survival to hospital discharge by 10–12% [2,3]. The final links in the Chain of Survival are effective Advanced Life Support and a new focus (5th link) on integrated post-resuscitation care, targeted at optimizing and preserving cardiac and cerebral function [8–10]. Any guidelines for BLS must be evidence based and consistent across a wide range of providers. Many countries have established national committees to advise community groups, ambulance services and the medical profession on appropriate BLS guidelines. Table 1.1.1 shows the national associations that made up the International Liaison Committee on Resuscitation (ILCOR) in 2010. The ILCOR group meets every 5 years to review the BLS and ALS guidelines and to evaluate the scientific evidence that may lead to changes. The next scheduled update is in 2015. Table 1.1.1 Membership of the International Liaison Committee on Resuscitation (ILCOR) 2010 American Heart Association (AHA) European Resuscitation Council (ERC) Heart and Stroke Foundation of Canada (HSFC) Resuscitation Council of Southern Africa (RCSA) Australian and New Zealand Committee on Resuscitation (ANZCOR) InterAmerican Heart Foundation (IAHF) Resuscitation Council of Asia (RCA) The most recent revision of the BLS guidelines occurred in 2010 and followed a comprehensive evaluation of the scientific literature for each aspect of BLS. Evidence evaluation worksheets were developed and were then considered by ILCOR (available at http://circ.ahajournals.org/content/122/16_suppl_2/S606.full.pdf). The final recommendations were published in late 2010 [11]. Subsequently, each national committee endorsed the guidelines with minor regional variations to take into account local practices. The recommendations of the Australian Resuscitation Council (ARC) combined with the New Zealand Resuscitation Council (NZRC) on BLS were co-published in 2010 (available at http://www.resus.org.au/policy/guidelines/ and http://www.nzrc.org.nz/ respectively) [12]. A flowchart for the initial evaluation and provision of BLS for the collapsed patient is shown in Figure 1.1.1. This is based on a DRSABCD approach that includes Dangers?; Responsive?; Send for help; open Airway; normal Breathing? start CPR; and attach Defibrillator. This process therefore covers the recognition that a patient has collapsed and is unresponsive, with a safe approach checking for danger and immediately sending for help to activate the emergency medical response team. This is followed by opening the airway and briefly checking for abnormal or absent breathing, with rapid commencement of chest compressions with breaths if the pulse is absent. A defibrillator is attached as soon as it is available and prompts followed if it is automatic or semiautomatic. A significant change to the adult BLS in the ILCOR 2010 resuscitation guidelines was the recommendation for a CAB (Compressions, Airway, Breathing) sequence instead of an ABC (Airway, Breathing, Compressions) sequence. This was aimed at minimizing any delay to initiate chest compressions, particularly when sudden collapse is witnessed and of likely cardiac origin. Thus, rescuers of adult cardiac arrest victims should begin resuscitation with 30 compressions followed by two breaths, rather than opening the airway and delivering breaths first (that wastes valuable time) [11]. ILCOR 2010 also mentions that, for unresponsive adults and children, the airway may be opened using the head tilt–chin lift manoeuvre when assessing breathing or giving ventilations. There are, however, regional variations in the interpretation and incorporation of opening the airway within the BLS algorithm. In the European Resuscitation Council (ERC) and the Australian Resuscitation Council (ARC) with the New Zealand Resuscitation Council (NZRC) algorithm, opening the airway comes before assessment of breathing followed by compression if required. This effectively preserves the ABC sequence to avoid confusion, whereas the ILCOR 2010 guidelines and the American Heart Association (AHA) Resuscitation Guidelines 2010 recommend following a CAB sequence. The ILCOR 2010 universal BLS algorithm with ARC and NZRC considerations is discussed in the remainder of this chapter. As the patient is being approached, the rescuer should immediately consider any dangers that may be associated with the collapse of the patient. For example, the patient may have been electrocuted and there is a substantial risk of death to the rescuer if the power source is not switched off prior to patient contact. There may also be significant danger from injury from a passing vehicle in the case of a motor vehicle collision where a patient is unconscious, as well as the potential for fire. Therefore, unless the patient is entrapped, an unconscious patient should be carefully extricated from a vehicle prior to the arrival of emergency medical services, taking care to minimize movement of the spine. The risk of injury from fire or explosion is considered to exceed the risk of moving an unconscious patient prior to immobilization of the cervical spine with a collar. A patient who has collapsed in a confined space raises the possibility of poisoning with a toxic gas such as carbon monoxide. Do not enter the scene until it is declared safe by emergency services, usually the fire brigade. Likewise, the potential for hazardous agent release must be considered if multiple victims are present, such as an organophosphate causing multiple collapses and cardiac arrest. In this setting, rescuers must not enter the area and should await the arrival of EMS with a specialist Hazmat team to declare the area safe. The patient who has collapsed is rapidly assessed to determine whether there is unconsciousness and absence of normal breathing, indicating possible cardiorespiratory arrest. This is assessed by a gentle ‘shake and shout’ and observation of the patient’s response, rather than looking specifically for signs of life (that was deemed potentially confusing). Unresponsive patients should then be assessed for absent or inadequate breathing. Lay rescuers should suspect cardiac arrest if the patient is unresponsive to ‘shake and shout’ and immediately telephone the EMS (‘call first’). Lay rescuers should then follow the advice given by a dispatcher to provide BLS care. A trained rescuer or healthcare providers may check for unresponsiveness and abnormal breathing at the same time and then activate the EMS or cardiac arrest team. Alternatively, healthcare rescuers may commence resuscitation focusing on the airway for approximately 2 minutes before calling the EMS (‘CPR first’), when the collapse is due to suspected airway obstruction (choking) or inadequate ventilation (drowning, hanging, etc.). Make an assessment of breathing if a patient has collapsed and is apparently unconscious [12]. Place the patient supine if face down. A trained lay rescuer or healthcare rescuer may open the airway using the head tilt–chin lift manoeuvre when assessing breathing or giving ventilations, taking care not to move the neck in a suspected trauma case. Adequate respiration is assessed by visually inspecting the movement of the chest wall rise and listening for upper airway sounds. Occasional deep (agonal gasps) respirations may continue for a few minutes after the initial collapse in cases of cardiac arrest. These respirations are not considered to represent normal breathing. Cardiopulmonary resuscitation (CPR) is required if the patient is found to have inadequate or absent breathing on initial assessment. If the initial assessment of an unconscious patient reveals adequate respiration, turn the victim on his/her side and maintain in the semi-prone recovery position. Make constant checks to ensure continued respiration while awaiting the arrival of the EMS. Current recommendations for the untrained lay rescuer is that he or she should not attempt to palpate for a pulse, as a pulse check is inaccurate in this setting [11]. A healthcare provider should take no more than 10 seconds to check for a pulse. If the rescuer does not definitely feel a pulse within 10 seconds, chest compressions should be started immediately. The prior ABC sequence of BLS meant that chest compressions were often delayed while the rescuer opened the airway, positioned the patient, retrieved a barrier device or gave mouth-to-mouth expired air resuscitation (EAR) breaths as two initial ‘rescue breaths’. These are difficult and challenging to an untrained lay rescuer and result in significant delay in starting chest compressions, or worse still, not attempting CPR at all. Therefore, in the CAB sequence of BLS, the assessment is limited to checking for response and breathing and management starts with delivering 30 chest compressions. All lay rescuers (trained or untrained) and healthcare rescuers should begin CPR if the victim is unresponsive and not breathing (ignoring occasional agonal gasps). Place the patient supine on a firm surface, such as a backboard, hard mattress or even the floor, to optimize the effectiveness of chest compressions. The emphasis is on delivering high-quality chest compressions: rescuers should push hard to a depth of at least 5 cm (or 2 inches) at a rate of at least 100 compressions per minute, allowing full chest recoil and minimizing interruptions in chest compressions [11]. Hence the maxim: ‘push hard, push fast, allow complete recoil and minimize interruptions’. There is still ongoing debate as to whether external chest compressions generate blood flow via a ‘cardiac pump’ mechanism or a ‘thoracic pump’ mechanism. Whatever the predominant mechanism of blood flow, owing to the relative rigidity of the chest wall, chest compressions result in around 20% of normal cardiac output in the adult. Rescuers trained to provide ventilation should give two rescue breaths after each 30 compressions, for a compression–ventilation ratio of 30:2. In untrained rescuers, ‘compression-only’ CPR is recommended where rescuers are unable or unwilling to perform mouth-to-mouth breaths (‘standard’ CPR). This ‘compression-only’ CPR technique is also recommended when EMS dispatchers are providing telephone advice to the untrained rescuer. Healthcare professionals as well as lay rescuers are often uncomfortable doing mouth-to-mouth ventilations with an unknown victim of cardiac arrest. This should not, however, prevent them from carrying out ‘Hands only’ or ‘Chest compression only’ CPR. Compression only CPR by lay rescuers still improves survival over no CPR at all. In addition, there is growing evidence to support compression only CPR being as effective as conventional CPR, particularly when sudden collapse is witnessed and of likely cardiac origin [13–18]. In support of ‘Hands only’ or ‘Chest compression only’ CPR is that if the airway is open, passive chest recoil during the relaxation phase of the chest compressions does also provide some air exchange. However, during prolonged CPR supplementary oxygen with assisted ventilation will be necessary. The precise interval during which the performance of compression only CPR is acceptable is currently unknown. Interestingly, no prospective adult cardiac arrest study has demonstrated that lay rescuer conventional CPR provides a better outcome than compression only CPR prior to EMS arrival. It is reasonable to open the airway using the head tilt–chin lift manoeuvre when assessing breathing or giving ventilations in an unresponsive adult or child. Solid material in the oropharynx should be removed with a careful sweep of a finger if inspection of the airway reveals visible foreign material or vomitus in the upper airway. Take particular care not to cause pharyngeal trauma or propel material further down into the lower airway and not to be bitten! If a victim suspected of a foreign body airway obstruction (FBAO) can cough, encourage him or her to cough and expel it out. If the cough is ineffective and the patient is conscious, give him/her up to 5 back blows with the heel of the hand and then up to 5 chest thrusts at the same compression point as in CPR, but sharper and slower. These techniques may be alternated, but make certain to call for EMS. A num- ber of manoeuvres have been proposed to clear the airway if it is completely obstructed by a foreign body. In many countries, abdominal thrusts are still endorsed as the technique of choice (Heimlich manoeuvre). However, as this technique is associated with life-threatening complications, such as intra-abdominal injury, it is no longer recommended by the ARC or NZRC. Instead, the preferred technique for clearing an obstructed airway is by alternating back blows and/or chest thrusts. Simple airway equipment may be used as an adjunct to EAR, when cardiac arrest occurs in a medical facility. These include a simple face-mask, or bag/valve/mask ventilation, with or without an oropharyngeal Guedel airway. This equipment has the advantage of familiarity, decreases the risk of cross-infection, is aesthetically more appealing and may deliver additional oxygen, but does require prior training [19]. Whichever technique of assisted ventilation is used, the adequacy of the tidal volume is assessed by a rise of the victim’s chest, delivered over one second. There is insufficient evidence to support or refute the use of a titrated oxygen concentration or constant 21% oxygen (room air), compared with 100% oxygen during adult cardiac arrest. Current guidelines during adult cardiac arrest therefore support the use of any of expired air ventilation, bag/valve/mask using air, or up to 100% oxygen if available [11]. As soon as a defibrillator arrives, the electrode pads are attached to the victim and the device switched on. Self-adhesive defibrillation pads have practical benefits over paddles for routine monitoring and defibrillation. They are safe, effective and now preferred to standard defibrillation paddles but, in all cases, the safety of rescuers and other team members is still paramount on shock delivery. When using a semiautomatic external defibrillator, the rescuer follows the voice instruction ‘stand clear’ and ‘press the button’ when asked to deliver the shock, if this is indicated. When using a manual defibrillator, the healthcare rescuer must personally select the desired energy level and deliver a shock after recognizing a shockable rhythm (VF or pulseless VT). Irrespective of the resultant rhythm, chest compressions must be resumed immediately after each shock to minimize the ‘no-flow’ time; that is the time during which compressions are not delivered, for example during any rhythm analysis. Strategies to reduce the delay between stopping chest compressions and the delivery of a shock, the ‘pre-shock pause’, must also be kept to an absolute minimum to improve the chances of shock success [20,21]. Even a 5–10 second delay will reduce the chances of the shock being successful [22–24]. All modern defibrillators are now biphasic rather than monophasic and are more effective in terminating ventricular arrhythmias at lower energy levels [25,26]. However, there is still no randomized study that shows superiority in terms of neurological survival or survival to hospital discharge. If a shock is not indicated, the rescuer should immediately resume CPR at a 30:2 compression–ventilation ratio and wait for EMS arrival or for the victim to start to recover. The semiautomatic external defibrillator is now considered part of BLS. SAED devices are extremely accurate in diagnosing ventricular fibrillation or ventricular tachycardia. SAEDs are simple, safe and effective when used by either lay rescuers or healthcare professionals (in or out of hospital) [27]. A systematic review assessing the risk of SAED use to the rescuers reported 29 adverse events associated with defibrillation [28], but none have been published since 1997 [29]. SAEDs have been shown to be an effective part of the BLS programme in public places, such as airports [6], sport facilities, offices, aircraft [30,31], and in casinos [7], where minimally trained rescuers are on the scene quickly for a witnessed cardiac arrest. Lay rescuer AED programmes by police officers as first responders have achieved reported survival rates as high as 49–74% [32,33]. Recent data from national studies in Japan and the USA [34,35] showed that where an AED was available, victims were defibrillated sooner and had a better chance of survival. Finally, an SAED may be placed in the home of a patient who is at increased risk of sudden cardiac arrest, for use by a relative who might witness the event. However, a recent study that enrolled 7001 patients concluded that survival rates from sudden cardiac arrest at home were not increased, even when a defibrillator was available in the home [36]. Patients at highest immediate risk of unexpected cardiac arrest may have an implantable cardioverter defibrillator (ICD) inserted which, on sensing a shockable rhythm, will discharge approximately 40 J through an internal pacing wire embedded in the right ventricle. Although most patients with an implanted defibrillator remain conscious during defibrillation, CPR should be commenced if the patient fails to respond to the ICD counter shocks and becomes unconscious. In such cases, any intermittent firing of the implanted defibrillator presents no additional risk to bystanders or medical personnel. However, wearing gloves and minimizing contact with the patient while the device is discharging is prudent. The five links in the ‘Chain of Survival’ BLS for a patient with sudden cardiac arrest include the following: Cardiac arrest may be presumed if the adult victim is unresponsive and not breathing normally (ignoring occasional gasps) without assessing for a pulse. A trained rescuer may open the airway using the head tilt–chin lift manoeuvre as part of the breathing assessment, but the lay/untrained rescuer should waste no time to initiate chest compressions. Rescuers should activate help/the EMS system and start chest compressions immediately. If a lone healthcare rescuer responds to suspected asphyxia or respiratory-related cardiac arrest (e.g. immersion or drowning), it is still reasonable for the healthcare rescuer to provide 2 minutes CPR before leaving the victim alone to activate EMS. All rescuers, whether trained or not, should at least provide chest compressions to a victim of cardiac arrest, with a strong emphasis on delivering high quality chest compressions. Trained rescuers should also provide 2 rescue breath ventilations after each 30 chest compressions at a ratio of 30:2, that is to deliver 5 cycles each 2 minutes. The compression rate should be at least 100 per minute and a depth of at least 5 cm (or 2 inches). All BLS guidelines encourage the use of an SAED by lay rescuers in cardiac arrest, maintaining chest compressions while charging the defibrillator to minimize any pre-shock pause. Basic Life Support care should be continued until advanced help arrives, the victim starts to wake or the rescuer becomes exhausted and the situation is considered hopeless. John E Maguire
Resuscitation
1.1 Basic Life Support
Introduction
Chain of Survival
Development of protocols
Revision of the BLS guidelines, 2010
Australian Resuscitation Council (ARC) and New Zealand Resuscitation Council (NZRC) BLS guidelines
DRSABCD approach to Basic Life Support
Change to the adult BLS in 2010
Regional variations
Check for dangers
Collapse in a confined space
Check for response and send for help
Assessment of airway, breathing and circulation
Cardiopulmonary resuscitation
Management
Chest compressions
‘Cardiac pump’ or a ‘thoracic pump’ mechanism
Chest compressions with ventilation
Chest compression only CPR
Passive chest recoil
Airway and breathing
Foreign body airway obstruction
Airway obstruction manoeuvres
Airway equipment
Defibrillation
Shock delivery
Minimizing interruptions to chest compressions
Semiautomatic external defibrillator
Lay rescuer/non-medical personnel and public access SAED
Home access SAED
Implantable cardioverter defibrillator and CPR
Basic Life Support (BLS) summary
 Immediate recognition of the emergency and activation of help/the EMS system
Immediate recognition of the emergency and activation of help/the EMS system
 Early CPR with an emphasis on chest compressions
Early CPR with an emphasis on chest compressions
 Earliest use of defibrillation
Earliest use of defibrillation
 Effective Advanced Life Support
Effective Advanced Life Support
1.2 Advanced Life Support
1. Resuscitation