Ultrasound-Guided Saphenous Nerve Block of the Thigh, Knee, and Ankle
Part 1: Saphenous Nerve Block of the Thigh
Steven L. Orebaugh
Vihang D. Shah
Milena Moreno
Paul E. Bigeleisen
 Background and indications: Block of the saphenous nerve is useful for anesthesia and postoperative analgesia for foot and ankle procedures involving the medial dermatomes as well as surgery involving the medial aspect of the leg. Saphenous nerve block has been described using different approaches. Techniques for guiding the block have included sensory nerve stimulation, motor nerve stimulation (of adjacent femoral nerve branches), and surface landmarks alone. Described approaches include the perifemoral, subsartorial/adductor canal, medial femoral condylar, paravenous tibial condylar, and medial malleolar/cuTaneous.1,2 Ultrasonography allows increased precision for this block.
Background and indications: Block of the saphenous nerve is useful for anesthesia and postoperative analgesia for foot and ankle procedures involving the medial dermatomes as well as surgery involving the medial aspect of the leg. Saphenous nerve block has been described using different approaches. Techniques for guiding the block have included sensory nerve stimulation, motor nerve stimulation (of adjacent femoral nerve branches), and surface landmarks alone. Described approaches include the perifemoral, subsartorial/adductor canal, medial femoral condylar, paravenous tibial condylar, and medial malleolar/cuTaneous.1,2 Ultrasonography allows increased precision for this block. Anatomy: The saphenous nerve may be approached with ultrasound guidance at several different levels. The nerve may be difficult to locate distally because of its small size, and therefore, the block relies on identification of nearby anatomy.
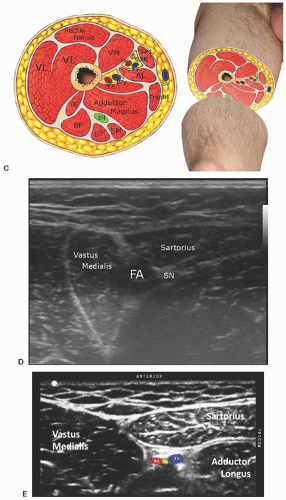
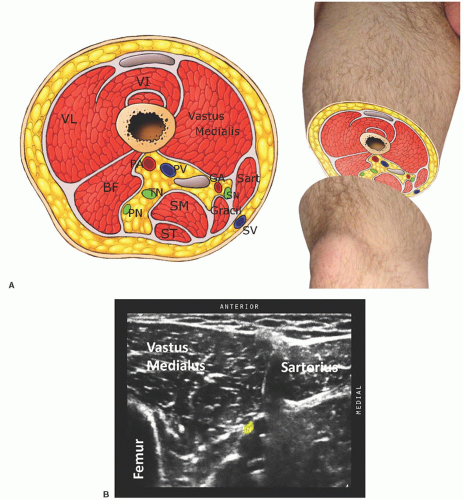
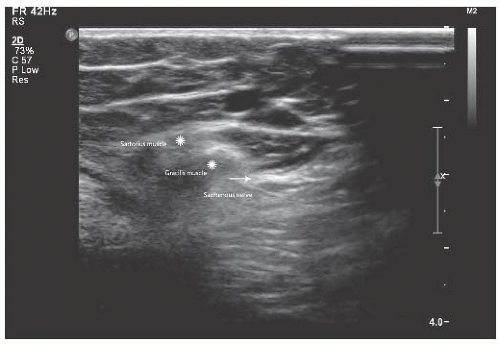
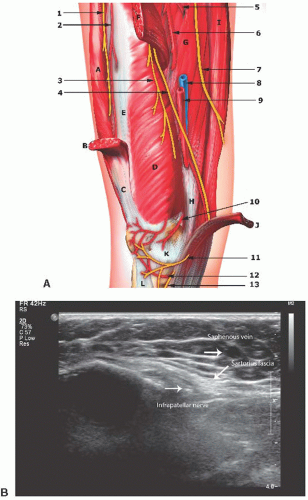
Anatomy: The saphenous nerve may be approached with ultrasound guidance at several different levels. The nerve may be difficult to locate distally because of its small size, and therefore, the block relies on identification of nearby anatomy.After the arborization of the femoral nerve at the femoral crease, the saphenous nerve runs distally with the femoral artery and vein, and, eventually joins the saphenous vein in the lower leg (Figs. 25.1 25.2, 25.3, 25.4, 25.5 and 25.6). Soon after leaving the femoral triangle, the nerve, artery, and vein dive deep through the adductor canal. Initially, the saphenous nerve is lateral to the artery. In the distal part of the adductor canal, just proximal to the adductor magnus muscle, the saphenous nerve traverses anteriorly over the femoral artery to then run along the medial side of the artery. The adductor canal is bounded anteriorly by the sartorius muscle, anterolaterally by the vastus medialis, and posteromedially by the adductor longus muscle.3 The nerve may be blocked at any point along this path by placing local anesthetic perivascularly or next to the nerve if it is visualized (Fig. 25.1). Distal to the adductor canal, the saphenous nerve resides below the sartorius and soon passes through the vastoadductor membrane, the fascial plane just deep to the sartorius muscle, and adjacent to the vastus medialis (Fig. 25.2). At this point, the nerve is ensconced in the connective tissue septum and runs with a small artery and vein, which may be visible on ultrasound with the color Doppler feature. The nerve, artery, and vein within this plane have been described as a “string of beads.”4 However, the individual structures are small and may require a very high-resolution transducer to distinguish. Local anesthetic may also be injected at this level to block the saphenous nerve. As the femoral artery and vein descend through the adductor hiatus to become the popliteal vessels, the saphenous nerve courses distally beneath the sartorius muscle. It passes medial to the knee joint,3 after which it runs in close juxtaposition to the saphenous vein, which may be identified on ultrasound to help guide the blockade of the nerve. In this position it is usually referred to as the infrapatellar nerve (IPN).
 Transducer: 25-mm linear transducer oscillating at 13 MHz (ankle or tibia) or 11-mm curved transducer oscillating at 6 to 10 MHz (thigh).
Transducer: 25-mm linear transducer oscillating at 13 MHz (ankle or tibia) or 11-mm curved transducer oscillating at 6 to 10 MHz (thigh). Figure 25.6. A: Anatomy of the saphenous nerve at the ankle. n., nerve; v., vein. B: Probe position for saphenous nerve at the ankle. C: Ultrasound of the saphenous nerve at the ankle. |
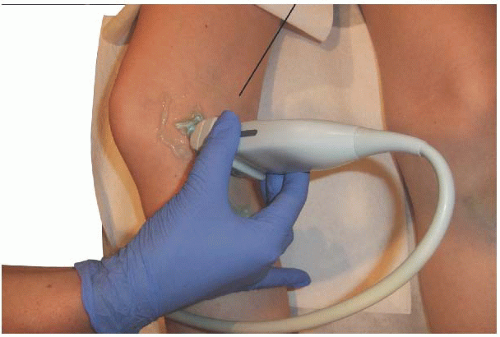
 Technique: Supplemental oxygen and monitors are applied to the patient. An appropriate marking is placed on the indicated extremity for confirmation, and a preprocedural “timeout” is performed at bedside. Mild sedation is administered to the patient. An antiseptic is utilized to prepare the skin over the block area. Peripheral nerve stimulation is not typically used for this block because there is no motor component.
Technique: Supplemental oxygen and monitors are applied to the patient. An appropriate marking is placed on the indicated extremity for confirmation, and a preprocedural “timeout” is performed at bedside. Mild sedation is administered to the patient. An antiseptic is utilized to prepare the skin over the block area. Peripheral nerve stimulation is not typically used for this block because there is no motor component.For the perivenous approach to the saphenous nerve in the upper leg, one should identify the saphenous vein and trace it to the level of the tibial tubercle. Lower approaches may allow branching to occur above the level of the block, resulting in incomplete anesthesia of the nerve. Once the vein is identified, the skin is anesthetized with 0.5 to 1 mL of lidocaine 1%, and the block needle is inserted through this site. Either an in-plane or out-of-plane technique is possible for any of the saphenous nerve block techniques. One advantage of the out-of-plane approach is that only one injection site is used because the needle’s angle of insertion can be changed using the same entry point. In either case, ultrasound guidance is used to guide the tip of the needle to a perivenous position (Fig. 25.1), and 2 to 3 mL of local anesthetic is injected on each side. Completely surrounding the vein with local anesthetic is desirable because the nerve is frequently not well distinguished. Two injections may be required to accomplish this.
In the midthigh approach, the ultrasound probe is placed over the femoral artery at the midthigh, and the vessels are followed distally toward the adductor canal. The saphenous nerve is contiguous to the artery and usually visible on ultrasound (Fig. 25.1). Just distal to the entry of the femoral vessels into the adductor canal, the vastoadductor membrane is visible as a fascial plane deep to the sartorius and along the medial edge of the vastus medialis. More distally, this membrane contains both the saphenous nerve and an accompanying small vein and artery, giving the appearance of a string of beads.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree