Ultrasound-Guided Pudendal Nerve Block
Rachael Seib
Philip Peng
 Background and indications: Pudendal neuralgia refers to chronic pelvic pain where pain is experienced in the regions innervated by the pudendal nerve,1 specifically the clitoris, penis, and perianal area.1, 2and 3 Its prevalence is estimated at approximately 1% of the general population,4 with a female to male preponderance of 2.5:1.5 The pain is typically burning or tingling in cHaracter, and it affects either the entire area supplied by the pudendal nerve or only a particular branch.6 Classically, the pain is exacerbated by sitting and alleviated when pressure is removed from the nerve, as in sTanding or lying on the unaffected side.7 Anecdotally, the pain is better with sitting on a toilet seat versus a chair.6 Although the cause of pudendal neuralgia is often not readily identifiable, risk factors include bicycle riding, vaginal delivery, countertraction devices in orthopedic surgery, pelvic trauma, and certain kinds of athletic activity.8, 9, 10, 11and 12 A pudendal nerve block is an imporTant tool in the diagnosis of this condition and may also serve therapeutic value.
Background and indications: Pudendal neuralgia refers to chronic pelvic pain where pain is experienced in the regions innervated by the pudendal nerve,1 specifically the clitoris, penis, and perianal area.1, 2and 3 Its prevalence is estimated at approximately 1% of the general population,4 with a female to male preponderance of 2.5:1.5 The pain is typically burning or tingling in cHaracter, and it affects either the entire area supplied by the pudendal nerve or only a particular branch.6 Classically, the pain is exacerbated by sitting and alleviated when pressure is removed from the nerve, as in sTanding or lying on the unaffected side.7 Anecdotally, the pain is better with sitting on a toilet seat versus a chair.6 Although the cause of pudendal neuralgia is often not readily identifiable, risk factors include bicycle riding, vaginal delivery, countertraction devices in orthopedic surgery, pelvic trauma, and certain kinds of athletic activity.8, 9, 10, 11and 12 A pudendal nerve block is an imporTant tool in the diagnosis of this condition and may also serve therapeutic value. Anatomy: The pudendal nerve contains both motor and sensory fibers.13 Its sensory fibers supply the clitoris, penis, vulva, and perianal area, and its motor fibers supply the external anal sphincter and deep muscles of the urogenital triangle.14,15 It is formed from the anterior rami of the second, third, and fourth sacral nerves.13 Exiting the pelvis through the greater sciatic foramen,16 the pudendal nerve is accompanied by the internal pudendal artery on its medial side (Fig. 49.1). At the level of the ischial spine, the nerve is situated between the sacrospinous and sacrotuberous ligaments in what is referred to as the interligamentous plane.17,18 At this level, 30% to 40% of pudendal nerves will be two- or three-trunked.15,19
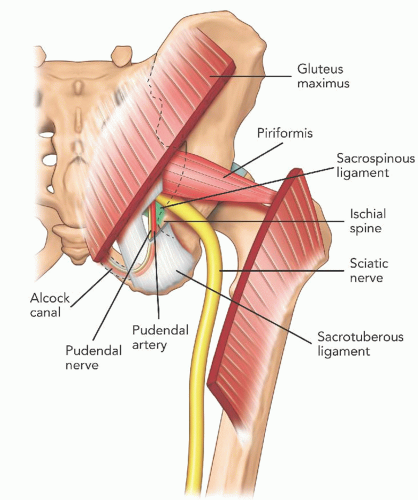
Anatomy: The pudendal nerve contains both motor and sensory fibers.13 Its sensory fibers supply the clitoris, penis, vulva, and perianal area, and its motor fibers supply the external anal sphincter and deep muscles of the urogenital triangle.14,15 It is formed from the anterior rami of the second, third, and fourth sacral nerves.13 Exiting the pelvis through the greater sciatic foramen,16 the pudendal nerve is accompanied by the internal pudendal artery on its medial side (Fig. 49.1). At the level of the ischial spine, the nerve is situated between the sacrospinous and sacrotuberous ligaments in what is referred to as the interligamentous plane.17,18 At this level, 30% to 40% of pudendal nerves will be two- or three-trunked.15,19Within the interligamentous plane, the pudendal artery is located lateral to the pudendal nerve in the vast majority of cases (76% to 100%).20 Following its passage between the two ligaments, the pudendal nerve travels anteriorly to enter the pelvis through Alcock canal.15,19,21 Alcock canal (also known as the pudendal canal) is a fascial tunnel created by the duplication of the obturator internus muscle under the plane of the levator ani muscle on the lateral wall of the ischiorectal fossa (Fig. 49.2).22 At the level of Alcock canal or just subsequent to it, the pudendal nerve sprouts three terminal branches: the dorsal nerve of the clitoris, the inferior rectal nerve, and the perineal nerve, providing the sensory branches to the skin of the perianal area, labia majora, and clitoris, respectively (Fig. 49.2).5
The path of the pudendal nerve, sandwiched between the sacrotuberous and the sacrospinous ligaments at one end and within Alcock canal at the other, makes it susceptible to entrapment.1,23 Furthermore, the course of the dorsal nerve of the penis under the subpubic arc exposes the nerve in cyclists to compression by the nose of the saddle of a bicycle.24 The configuration of the nerve in the pelvis also makes it susceptible to stretch during vaginal delivery.25
Although the best imaging technique for Alcock canal is computed tomography scan,18 ultrasound is useful in imaging the interligamentous plane at the ischial spine level. To reveal the structures at this level, the key is to recognize the ischial spine (Fig. 49.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree