INCIDENCE AND EPIDEMIOLOGY OF STROKE
In the United States, stroke is ranked as the fourth major cause of death after heart disease, cancer, and chronic lower respiratory disease (Centers for Disease Control and Prevention [CDC], 2014). A historical perspective provides a context for considering the rankings. Stroke moved from second to third as the major cause of mortality in 1937, although stroke mortality was stable from 1930 to 1960 at 175.0 per 100,000. A decline in mortality ensued from 1960 to the 2000s. By 2008, the age-adjusted annual death rate from stroke was 40.6 per 100,000, a clear three-fourths less than during the period of 1931 to 1960 (Towfighi & Saver, 2011). The total stroke mortality in the United States declined from a high of 214,000 in 1937 to 134,000 in 2008 (CDC, 2014). Concurrently, the National Center for Health Statistics revised their methodology for counting chronic lower respiratory disease (CLRD) deaths to include deaths due to pneumonia, influenza, and bronchitis in the CLRD category. This change resulted in a sharp increase in the number of deaths from 2007 to 2008 in the CLRD category. The increase in CLRD coupled with a decrease in stroke deaths resulted in the shifting of the rank of third to fourth for stroke mortality.
In a 2014 statement from the American Heart Association/American Stroke Association concerning factors influencing the decline in stroke mortality, the following conclusions were drawn.
The decline in stroke mortality is real and represents a major public health and clinical medicine success story. The repositioning of stroke from third to fourth leading cause of death is the result of true mortality decline and not an increase in mortality from chronic lung disease, which is now the third leading cause of death in the United States. There is strong evidence that the decline can be attributed to a combination of interventions and programs based on scientific findings and implemented with the purpose of reducing stroke risks, the most likely being the improved control of hypertension. Thus, research studies and the application of their findings in developing intervention programs have improved the health of the population. The continued application of aggressive evidence-based public health programs and clinical interventions is expected to result in further declines in stroke mortality. (Lackland et al., 2014, p. 315)
Regardless of changes in the methods of counting deaths, the data show a decline in stroke that can be explained as result of improvement in the management of the risk factors of hypertension and smoking. Although this is encouraging, there are still almost 800,000 Americans who sustain a stroke each year; there is much left to be done in the primary and secondary prevention of stroke.
The American Heart Association Statistical Update for 2014 provides information about stroke, which is summarized as follows (Go et al., 2013).
● Each year in the United States, 795,000 people have a first or recurrent stroke. Approximately 610,000 of these are first strokes, and 185,000 are recurrent strokes.
● The classification of stroke includes 87% ischemic, 10% intercerebral hemorrhagic, and 3% subarachnoid hemorrhage.
● On a yearly basis, 55,000 more women than men have a stroke.
● Women have a higher lifetime risk of stroke than men among those 55 to 75 years of age, with a one in five chance for women as compared to one in six for men.
● About 6.8 million Americans 20 years of age and older have had a stroke.
● African Americans’ risk of a first stroke is nearly twice that of Caucasians; African Americans are more likely to die following a stroke than Caucasians (Rogers et al., 2012).
● Risk of stroke in Hispanics falls between that of Caucasians and African Americans.
In summary, stroke is ranked the fourth cause of death in the United States. Stroke is both an acute and a chronic health problem that has a major impact on individuals, families, and the health care system. Although much progress has been made in understanding the pathophysiology, diagnosis, and treatment of stroke, there is still much to be learned. The high incidence of stroke in African Americans and Hispanics is still to be elucidated to better prevent and treat stroke in the future.
 EVOLVING DEFINITIONS OF STROKE
EVOLVING DEFINITIONS OF STROKE
Although the global impact of stroke is well recognized, and the science in elucidating the pathophysiology of cerebrovascular disease has made remarkable progress, the term stroke is not defined consistently in clinical practice, in research, and in the population assessment and surveillance of stroke nor is it reflective of 21st century knowledge. With this background in mind, the American Heart Association (AHA) and the American Stroke Association (ASA) convened an expert panel to update the definition of stroke for the 21st century (Sacco et al., 2013). Both the definition and terms used to define and describe stroke have evolved over time. Recent advancements in imaging technology enhance the basic understanding of the pathophysiology of stroke, and other scientific advancements have warranted a critical review for relevance to the 21st century.
First called apoplexy by Hippocrates about 400 BC, the term stroke was introduced in 1689 by William Cole. Along the way, the term cerebrovascular accident (CVA) emerged, although in the last few decades, stroke has become the accepted term. An understanding that the acute nontraumatic brain injury called stroke was a heterogeneous presentation of signs and symptoms perhaps added to the confusion around a definition. The addition of the term transient ischemic attack in the late 1950s was a response to the work of C. Miller Fisher, which described the temporary episodes of brain and eye ischemia (Fisher, 1958; Mohr, 2004). In 1975, an Ad Hoc Committee on Cerebrovascular Disease published the following definition: “Transient ischemic attacks are episodes of temporary and focal dysfunction of vascular origin, which are variable in duration, commonly lasting from 2 to 15 minutes, but occasionally lasting as long as a day (24 hours). They leave no persistent neurological deficit” (p. 567). Of particular interest was that the 24-hour time frame was arbitrarily chosen based on consensus rather than scientific data. As noted by Sacco et al. (2013), when this definition of transient ischemic attack (TIA) was formulated, neither diagnostic procedures that could determine the presence of brain infarction were available nor were effective treatments for brain ischemia established. This definition of TIA was universally used until the beginning of the 21st century when accumulating data from scientific discoveries and diagnostic imaging prompted interest in revising definitions.
In 2002, an expert committee (Albers et al., 2002) proposed a new definition: “A TIA is a brief episode of neurologic dysfunction caused by focal brain or retinal ischemia, with clinical symptoms typically lasting less than one hour, and without evidence of acute infarction” (p. 1715). Easton et al. (2009) chaired an expert committee of the AHA/ASA, which published a scientific statement defining TIA and recommending evaluation. The definition proposed was “transient ischemic attack (TIA) is a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction” (p. 2276). Of note is that the duration of the event was removed. The International Classification of Diseases (ICD) system, owned by the World Health Organization (WHO), aims to standardize diagnostic classification for most diseases. The most current version is the ICD-10; it is the foundation for ICD-10-Clinical Modification (CM) or ICD-10-CM. According the preface to the ICD-10-CM for FY 2015, the ICD-10-CM is the United States’ clinical modification of the WHO’s ICD-10. The term “clinical” is used to emphasize the modification’s intent which is to serve as a useful tool in the area of classification of morbidity data for indexing of health records, medical care review, and ambulatory and other health care programs, as well as for basic health statistics (CDC, 2015). The 11th revision of the ICD, along with its clinical modification (ICD-11-CM), is scheduled for release in 2017. The current ICD-1-CM classifies cerebrovascular disorders chiefly as TIA, cerebral ischemic stroke, intercerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH).
The WHO definition of stroke is a “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, with symptoms lasting 24 hours or longer or leading to death, with no apparent cause other than of vascular origin” (Aho et al., 1980, p. 114). By comparing this definition to TIA, which is defined as lasting less than 24 hours, patients with stroke symptoms caused by subdural hemorrhage, tumors, poisoning, or trauma are excluded. This definition, first introduced in 1970, is still found in the WHO website.
 UPDATED DEFINITION OF STROKE FOR THE 21ST CENTURY
UPDATED DEFINITION OF STROKE FOR THE 21ST CENTURY
“An Updated Definition of Stroke for the 21st Century: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association” (Sacco et al., 2013) incorporates 21st century science and knowledge amassed from research and technological advances in diagnostic imaging. The following is the 2013 definition of stroke from AHA/ASA (Sacco et al., 2013, p. 2066). The reader is directed to this 2013 document for more detailed information about the subtypes of stroke included in the new definition. The term stroke is broadly defined to include all of the following:
Definition of central nervous system (CNS) infarction: CNS infarction is brain, spinal cord, or retinal cell death attributable to ischemia based on the following:
1. Pathological, imaging, or other objective evidence of cerebral, spinal cord, or retinal focal ischemic injury in a defined vascular distribution; or
2. Clinical evidence of cerebral, spinal cord, or retinal focal ischemic injury based on symptoms persisting ≥24 hours or until death, and other etiologies excluded. (Note: CNS infarction includes hemorrhagic infarctions, types I and II.)
Definition of ischemic stroke: An episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infarction. (Note: Evidence of CNS infarction is defined above.)
Definition of silent CNS infarction: Imaging or neuropathological evidence of CNS infarction, without a history of acute neurological dysfunction attributable to the lesion.
Definition of intracerebral hemorrhage: A focal collection of blood within the brain parenchyma or ventricular system that is not caused by trauma. (Note: Intracerebral hemorrhage includes parenchymal hemorrhages after CNS infarction, types I and II.)
Definition of stroke caused by intracerebral hemorrhage: Rapidly developing clinical signs of neurological dysfunction attributable to a focal collection of blood within the brain parenchyma or ventricular system that is not caused by trauma.
Definition of silent cerebral hemorrhage: A focal collection of chronic blood products within the brain parenchyma, subarachnoid space, or ventricular system on neuroimaging or neuropathological examination that is not caused by trauma and without a history of acute neurological dysfunction attributable to the lesion.
Definition of subarachnoid hemorrhage: Bleeding into the subarachnoid space (the space between the arachnoid membrane and the pia mater of the brain or spinal cord).
Definition of stroke caused by subarachnoid hemorrhage: Rapidly developing signs of neurological dysfunction and/or headache because of bleeding into the subarachnoid space (the space between the arachnoid membrane and the pia mater of the brain or spinal cord), which is not caused by trauma.
Definition of stroke caused by cerebral venous thrombosis: Infarction or hemorrhage in the brain, spinal cord, or retina because of thrombosis of a cerebral venous structure. Symptoms or signs caused by reversible edema without infarction or hemorrhage do not qualify as stroke.
Definition of stroke, not otherwise specified: An episode of acute neurological dysfunction presumed to be caused by ischemia or hemorrhage, persisting ≥24 hours or until death, but without sufficient evidence to be classified as one of the above.
 IMPLICATIONS OF THE UPDATED DEFINITIONS FOR STROKE
IMPLICATIONS OF THE UPDATED DEFINITIONS FOR STROKE
The updated definition of stroke is congruent with the science, technology, and knowledge of the 21st century as of 2013. As science, technology, and clinical knowledge continue to develop, there will no doubt be revisions to this definition in the future. But for now, the updated definitions have implications in the areas of clinical practice, education, research, and health policy.
Clinical Practice
In clinical practice, the focus for any type of acute stroke syndromes continues to be on rapid clinical and diagnostic assessment/evaluation and rapid treatment. Because stroke is a heterogeneous diagnosis, the clinician must rapidly sort through ischemic versus hemorrhagic etiology as well as the specific form of ischemic or hemorrhagic origin of the problem in order to select the appropriate treatment plan. Time is critical to preserve cerebral tissue as well as to reverse ischemia in potentially salvable tissue. Contemporary imaging techniques have provided a cadre of diagnostic tools that not only help to differentiate stroke mimics from stroke but also provide anatomic, temporal, and other characteristics about ischemia and pathophysiological responses to a stroke event. Computed tomography (CT) scans can quickly differentiate a hemorrhagic stroke from an ischemic stroke. A magnetic resonance imaging (MRI) scan is useful to differentiate stroke mimics such as migraines and brain tumors from ischemic and hemorrhagic stroke. Special techniques such as an MRI diffusion-weighted imaging (DWI) provide information about the timeline of the stroke which highlights tissue changes from minutes to days (Furlan, Marchal, Viader, Derlon, & Baron, 1996; Olivot & Albers, 2010). Multimagnetic resonance angiography, DWI, fluid attenuated inversion recovery (FLAIR), and perfusion-weighted MRI are useful diagnostics to detect “mismatch” areas which identify areas of potentially reversible ischemia known as the penumbra. Doppler imaging of the blood vessels in the neck and other vascular imaging procedures provide information about patency and structure of cerebral vessels (Chalela et al., 2007). A detailed discussion of diagnostics is found in Chapter 5, Diagnostic Testing in Stroke.
Diagnostics also create gray areas for clinicians to consider. For example, what should be done when small infarcts or microhemorrhagic areas are noted on a scan without the presence of clinical signs or symptoms in the patient? These areas are currently identified as silent areas but can also be considered markers of cerebrovascular disease, albeit noted in an asymptomatic patient. The current recommendation is that the patient should be followed, assessed, and managed for vascular risk factors as strategies for stroke prevention (Sacco et al., 2013).
The rapid development of science, technology, and clinical knowledge about stroke and research has provided the evidence from professional organizations such as AHA and ASA to develop clinical practice evidence-based guidelines to promulgate best practice for stroke patients. Clinical facilities have used the guidelines to develop their own algorithms and protocols to guide the care and management of the stroke patients that they serve. Clinicians must understand the methodological developmental process for guidelines in order to be informed consumers of guidelines. For example, questions to be answered include the following: “What is the strength of the evidence used to develop the guidelines?” “Are the guideline based on evidence or consensus?” and “How is bias addressed in the process of guidelines development?” There are models available to evaluate guidelines which should be used to determine the strength and quality of guidelines.
Education
The updated definition of stroke is a major change reflective of current science, technology, and knowledge with significant implications for practice, research, and health policy. How are all clinicians who care for stroke patients informed of changing best practices regardless if they practice in urban and rural settings or academic or nonacademic centers? It is well known that change is a complex process that takes time. The usual routes for dissemination of professional information are publications, presentations, conferences, clinical practice guidelines, and other forms of educational methods such as webinars. However, to change practice in any setting, it takes change agents and champions to lead the change process. Leadership from professional organizations can help to promote dissemination of information and translation into practice to improve the outcomes for stroke patients through recommended effective strategies.
Research
Clear and consistent definitions of stroke, its subtypes, TIAs, and silent infarctions are critical for the interpretation of data from clinical trials, administrative stroke databases, and epidemiology in defining populations (Sacco et al., 2013). Operational definitions clarify variable attributes and suggest measurement criteria for variables and how the data can be recorded. The updates definition refocuses the former interest in time of development of symptoms to one of brain imaging tissue–based characteristics of ischemia and markers. The focus on brain imaging also influences the design of clinical investigations. For example, an appreciation of silent markers of asymptomatic cerebral infarction or microhemorrhagic areas noted on cerebral imaging broadens the scope of types of investigations to include prevention and longitudinal outcomes over multiple time points. Both documented strokes and asymptomatic silent markers provide opportunity for primary and secondary preventive strategies to be tested (Furie et al., 2011). The updated definitions of stroke have significant impact on stroke research for the future.
Health Policy
The change in the definition of stroke expands the scope of inclusion in the category of stroke. As a result, the disease prevalence will increase, but the mortality rate will most likely fall because milder forms of stroke will be included. When a definition of a disease is updated, the time of the definition change must be clearly noted for tracking of the disease over time for accurate interpretation of data and trends (Teutsch, 2010). With the updating of the definition of stroke, it will result in reclassification of stroke cases in incidence, prevalence, and mortality. In addition, the new definition has implications for public health, including surveillance and reporting, national and international statistics, disease classification coding systems, and existing health surveys (Sacco et al., 2013, p. 2081). Data collected through surveillance and registries will be different with the updated definition. This change will need to be taken in account when databases are mined for elucidating of trends and making projections for the future. This will also be an important consideration for researchers.
In summary, the updated definitions of stroke have a profound impact and ramifications for practice, education, research, and health policy especially how prevalence, incidence, and mortality are calculated and interpreted. It will be important to bear in mind when the redefinitions occurred and when it was incorporated into practice, education, research, and health policy arenas.
 STROKE BURDEN AND SURVEILLANCE
STROKE BURDEN AND SURVEILLANCE
Stroke Burden
The word burden means bearing of a heavy load. The concept of burden has been applied to multiple dimensions of health care at both the individual and population level such as treatment, family, disease, and economic burdens. Disease burden include incidence (yearly rate of onset, age of onset) and prevalence (the portion of the population found to have a condition). Treatment burden has been defined as “the self-care practices that patients with chronic illness must perform to respond to the requirements of their healthcare providers, as well as the impact that these practices have on patient functioning and well-being” (Gallacher et al., 2013, p. 1). As the level of treatment burden increases, patients may find it more difficult to adhere to the treatment plan, which can lead to poorer outcomes. The added “workload” of illness places demands on the patient’s time and energy for activities such as medical appointments, diagnostic testing, and taking medications as well as self-care aspects of self-monitoring (e.g., blood pressure, blood glucose), dietary modifications, and exercise (Gallacher et al., 2013). Care is complex and multidimensional especially in chronic illness management, and burden is an integral part of the trajectory.
Almost half of stroke survivors have residual deficits including weakness or cognitive dysfunction 6 months after a stroke (Kelly-Hayes et al., 2003). The impact of the workload on the patient and family affects the patient’s behavior and cognitive, physical, and psychological well-being (Eton et al., 2012; Shippee, Shah, May, Mair, & Mantori, 2009). Patients respond in different ways to what may appear as a similar burden to the outside observer so that a patient-centered approach is needed to appreciate the individual response, impact, and needs of each patient. With a chronic illness of a family member, the added burden on the family for caregiving, assistance with both activities of daily living (ADLs) as well as instrumental ADLs, redistribution of roles and responsibilities, and financial impact, the burden of a disease entity such as stroke is great. Treatment burden can also be viewed at the population level of the impact for needed health care and treatment on the health care resources at the local, national, or international level. The true impact of stroke must be viewed not only in terms of incidence and mortality rates but also from the lens of disability. Disability often persists for a long time and sometimes permanently after stroke (Norrving & Kissela, 2013).
Disease burden is the impact of a health problem and can be measured in terms of mortality, morbidity, treatment burden, economic burden, and other indicators. It is often quantified in terms of quality-adjusted life years (QALYs) or disability-adjusted life years (DALYs), both of which quantify the number of years lost due to disease. One DALY can be thought of as 1 year of healthy life lost, and the overall disease burden can be thought of as a measure of the gap between current health status and the ideal health status where the individual lives to old age and is free from disease and disability (Prüss-Üstün & Corvalán, 2006).
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD), published in 2010, reported that stroke was the second most common cause of death and the third most common cause of DALYs worldwide (Lozano et al., 2012). The study reported that although stroke mortality rates and mortality-to-incidence ratios have decreased in the past two decades, the global burden of stroke from a perspective of the absolute number of people affected every year, stroke survivors, related deaths, and DALYs lost are great and increasing, with most of the burden in low-income and middle-income countries. The investigators also reported that if these trends in stroke incidence, mortality, and DALYs continue, by 2030, there will be almost 12 million stroke deaths, 70 million stroke survivors, and more than 200 million DALYs lost globally as a result of stroke (Feigin et al., 2013). The human, health care resources, and economic burden of stroke is significant, but the projections for the future global burden are staggering and fall short of available health care resources.
Surveillance
From the perspective of public health, surveillance is the ongoing systematic collection, analysis, and interpretation of data, closely integrated with the timely dissemination of these data to those responsible for preventing and controlling disease and injury (Thacker & Berkelman, 1988). Public health surveillance is a tool to estimate the health status and behavior of the populations served by state agencies, federal health agencies, and ministries of health. Surveillance can directly measure actual activity in areas of interest within a population. It is, therefore, useful to measure both the need for interventions and the effects of interventions. The purpose of surveillance is to provide information to empower decision makers to make informed decisions. According to Mukherjee and Patil (2011), effective surveillance systems are most helpful when the health concern of interest is both a major public health problem and one that is thought to be preventable or modifiable.
At a basic level, all stroke surveillance systems should include data about incidence, case fatality, and mortality. More advanced systems include data on modalities of treatment, pre- and poststroke functional activity, categories of stroke, use of resources, access to care, and cost (Mukherjee & Patil, 2011). Unfortunately, even simple measures are not collected by many regions and countries, resulting in voids in data. In addition, storage of collected data may be an obstacle because of the lack of relational databases so that one database cannot be integrated with other databases. In creating stroke registries or other databases, it is important to have established common standards to address storage and integration of data for use at the population level. Need for surveillance and registries are critical for accurate data and data mining for research. Careful consideration of variables including how they are defined, operationalized, measured, and recorded is needed for standardization that will be useful for comparisons. Methods for extraction of clinical data from registries and combining those data with information-rich population data in a unified data stream are goals for the future. The AHA’s Get With The Guidelines database is an ongoing, continuous quality improvement program that collects concurrent and retrospective patient-level adherence data within U.S. hospitals. The Get With The Guidelines database measures hospitals’ adherence to secondary prevention guidelines (pharmacological and lifestyle interventions) for coronary artery disease, heart failure, and stroke (AHA, 2014). The contributions of data from facilities throughout the United States have made this a unique database for investigation of quality and quality improvement.
In summary, the burden of stroke can be considered at the individual and population level as well local, national, or global level. It is clear that stroke will continue to be a major health problem around the globe for the foreseeable future. Surveillance data are critical for monitoring population shifts and forecasting trends. As noted earlier, effective surveillance systems are most helpful when the health concern of interest is both a major public health problem and one that is thought to be preventable or modifiable. Stroke, in many cases, is preventable and modifiable. Efforts at prevention interventions to reduce the burden of stroke are being addressed.
 PREVENTION OF STROKE
PREVENTION OF STROKE
Prevention is classified into primary prevention and secondary prevention. Primary prevention of stroke and TIAs is directed at prevention of a first-time stroke. Secondary prevention of stroke and TIAs is directed at prevention of another stroke in persons who have had a stroke or who are experiencing TIAs. Both primary and secondary prevention will be addressed from the population and individual level and role of the interprofessional team.
From a global perspective, the INTERSTROKE study published in 2010 (O’Donnell et al., 2010) investigated risk factors for first-time acute stroke (e.g., all types of stroke) in 22 countries to set an agenda for targeted improvement. The five risk factors identified that contributed 80% to stroke risk were hypertension, smoking, waist-to-hip ratio, diet, and physical activity. Another 10% of stroke risk was due to diabetes mellitus, alcohol abuse, psychosocial factors (e.g., stress, depression), cardiac causes (i.e., atrial fibrillation, previous myocardial infarction, valvular heart disease), and ratio of apolipoprotein B to apolipoprotein A1 (O’Donnell et al., 2010). The response of the WHO was to propose five key components for stroke care that included the following: (1) primary care assessment and management of cardiovascular risk and TIA, (2) secondary prevention strategies, (3) education of the public and health care providers about stroke prevention and management, (4) access to stroke care and rehabilitation services, and (5) community and family support for patients with stroke and their caregivers (Mendis, 2010). In addition, the WHO has suggested a stepwise approach to stroke surveillance using standardized tools for data collection as a means to monitor progress (Norrving & Kissela, 2013). The INTERSTROKE study and the initiatives of the WHO applied to all forms of strokes.
Recent reports also indicate that in the last 40 years, there has been a shift in rates of stroke around the globe from the economically developed nations to the low- and middle-income countries. The rate of stroke has declined in the economically developed nations, whereas the rate has increased in the low- to middle-income countries. In addition, the rates of disability and mortality are about 10 times greater in medically underserved regions compared to the most developed countries due to a lack of services and other resources to treat the continuum of stroke needs (Norrving & Kissela, 2013). Many organizations are developing public health approaches to address the maldistribution of stroke services directed at decreasing stroke rates and improving patient outcomes for stroke patients. A combination of preventive measures, access to care, and treatment resources are being addressed comprehensively.
Moving from a global focus to a U.S. focus for stroke prevention, AHA/ASA have taken the lead in the development of evidence-based clinical practice guidelines for stroke including the prevention of stroke. Because of the complexity of the processes of developing guidelines and the needed resources, some organizations such as AHA and ASA are collaborating to support the development of high-quality guidelines. In addition, other organizations provide endorsements of published guidelines, further adding to the credibility of the product.
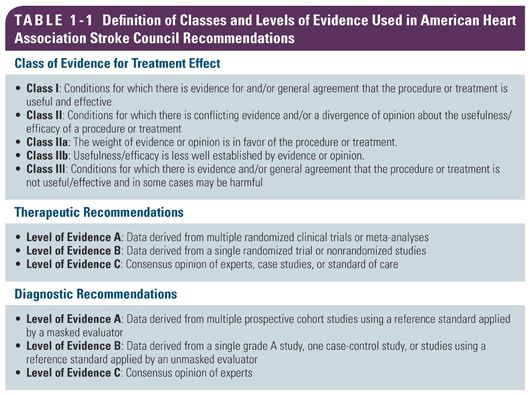
In order to help health professionals and others to determine quality of guidelines, rating systems have been established to rate the strength and quality of the evidence used in writing guidelines. There are a number of tools available to rate the strength of evidence. For example, AHA/ASA uses a two-dimensional classification system, which includes an estimate of certainty of treatment effect and size of treatment effect (Table 1-1). This is the criteria that AHA/ASA expert panels employ in the evaluation of evidence when developing guidelines. Other organizations employ other grading systems. In most instances, a description of the scope and methodology used in the development of the guidelines is provided, which includes a description of the search strategy used for the literature review (e.g., inclusion/exclusion criteria, time period of literature included, types of studies included), internal peer review process, qualifications of the expert panel members, and any potential conflict of interest that would suggest bias of any panel member. The reader can then better judge the rigor of the process and credibility of the guidelines.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


