Chapter 10 Cervical and Thoracic Discogenic Pain
Therapeutic Nonsurgical Options
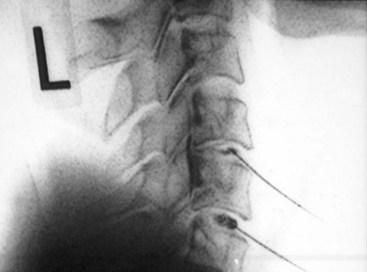
 Thoracic discography involves advancing the needle into the center of the disc on a course that bisects the two articulations of the head of the rib.
Thoracic discography involves advancing the needle into the center of the disc on a course that bisects the two articulations of the head of the rib.Cervical and Thoracic Discogenic Pain
Neck pain is a near ubiquitous complaint. Fortunately most neck pain is self-limited. Neck pain that limits activities is not uncommon, with 12-month prevalence estimates ranging from 2% to 11%.1 However, when neck pain becomes chronic, diagnosis of the pain generator may prove difficult. The source is more obvious when accompanied by radicular symptoms. The source of axial neck pain is often limited to myofascial, facetogenic, discogenic, and often a combination of all three.2 Posterior thorax pain is a much rarer entity than cervical and lumbar pain. A common cause of thoracic back pain is reflex muscle spasm radiating from an original lumbar pain source. Thoracic discs, facets, and myofascia are all possible sources of upper to midback pain. Of discogenic pain complaints 36% are of cervical origin, compared to only 4% in the thoracic regional. Obviously the remaining 62% involve the lumbar region.3,4
Clinical Presentation
Discogenic neck and upper back pain usually manifests in axial pain that may progress to involve radiculopathy. The disc may herniate, resulting in compression of the adjacent nerve root or cord segment. It may manifest an annular fissure (Fig. 10-1), resulting in chemical irritation of the adjacent nerve root or cord segment. The disc itself may prove painful, with neoinnervation of the annulus. History elements that suggest discogenic pain in the neck include pain with flexion, prolonged sitting, and protruded head positions. Physical examination findings that suggest cervical discogenic pain include decreased range of motion (ROM) and referred pain patterns (Fig. 10-2).5 If radiculopathy is present, compression tests such as the Spurling and shoulder abduction tests have a high specificity but low sensitivity.6 Sensory, motor, and reflex tests are helpful in cervical radiculopathy diagnosis. Myelopathic symptoms such as bowel/bladder changes, lower-extremity weakness, altered balance, and hyperreflexia point toward significant central disc herniation.
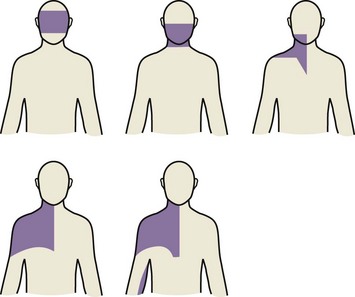
Fig. 10-1 Posterior view. Pain caused in varying distributions secondary to provocative cervical discography.
Adapted from Grubb SA et al: Cervical discography: clinical implications from 12 years of experience, Spine 25:1382-1389, 2000.