Commentary: Targeting Behavior Change in Chronic Pain Treatment: A Clinical Perspective
In this chapter, Fordyce focuses on observable pain and well behaviors as treatment goals rather that the cure or management of pain. Fordyce’s work represented a paradigm shift in how we treat chronic pain and helped move the field beyond the disease model. This change of focus stimulated new treatment approaches and interdisciplinary programs for chronic pain and contributed to improved functional outcomes. Fordyce focuses specifically on four behavioral treatment goals: 1) pain signals or pain behavior, 2) functional impairment behavior, 3) healthcare utilization behavior and 4) effective well behavior. This commentary provides an overview of these goals and highlights some of the problems that have prevented more widespread application of these principles in clinical care.
Fordyce argues that operant pain behaviors should be the focus of treatment rather than pain per se or the presumed underlying cause of pain. He recognized the limitations of continuing to treat chronic pain as if it was acute, emphasizing that when pain continues for an extended period of time, there are ample opportunities for pain behaviors to come under the influence of environmental contingencies. Additionally, the problem initially triggering pain and pain behavior may no longer be the cause of continued pain and illness behavior. Pain may be maintained by muscle guarding, abnormal posturing, physical deconditioning, or an increased focus of attention on pain. In fact, there is increasing evidence that chronic pain produces central neural network changes in the brain, thus changing the nature of the pain problem and requiring a very different treatment approach [7,9]. Treatment goals therefore shift from fixing the pain generator and alleviating pain to the reduction of illness behavior and the increase of well behavior.
Fordyce’s clinical perspective has continued to underpin the operant approach applied to persons with chronic pain and disability, particularly in those who are referred to the interdisciplinary pain rehabilitation program at the Rehabilitation Institute of Washington (RIW). The typical referral is an individual who has been disabled for several years and who has had dozens of imaging studies, multiple specialist evaluations, and every diagnostic test imaginable, all in a quest to identify the cause of pain so it could be repaired. Typically they have had limited or no active treatments or attempts to alter their behavior. Physical therapy, if done at all, has been largely passive, using electrical stimulation, ultrasound, massage, and other passive modalities. Treatment usually has focused almost entirely on alleviating pain via surgery, medications, injections, and a variety of other palliative or passive treatments. Activity restrictions have been excessive and prolonged leading to profound deconditioning and disability.
This never ending search for the pain generator, combined with delayed active treatment, has probably been an important factor in leading to preventable long term disability in many individuals and greater costs for insurance carriers. Fordyce writes that “Early and effective treatment pays off financially as well as in other ways (p. 187).” The longer an injured worker remains off work, the greater the risk of long term disability. Those off work more than four weeks have a 20% chance of chronic disability [11]. For those off work more than two years with back pain, the probability of returning to work drops to almost zero [10]. Low back pain claims lasting longer than 12 months represent less than 5% of the claims, but account for 65% of the cost of all claims [6].
Despite the high risk of chronic disability noted above for those disabled more than two years, patients entering our interdisciplinary pain rehabilitation program—with Fordyce-consistent goals of improving function and well behaviors, decreasing pain behaviors, learning to self-manage pain and decrease use of healthcare, and return to gainful employment—demonstrate remarkable behavioral changes and most return to work following treatment. Unpublished outcome data from our program for 868 patients treated during 2006 to 2012 show that patients demonstrate an average 200% to 300% increase in various objective measures of flexibility, strength, endurance and functional activities and 98% of patients demonstrate the physical ability to return to full time employment by the end of treatment. Seventy-four percent of patients had either returned to work or were involved in vocational retraining within one year of treatment completion. For two years of available opioid use data (n5212), 82% of patients were taking daily opioids at the start of treatment, but only 18% were still using opioids at twelve week follow-up, and almost all of those were still completing a taper and using very low amounts of opioids (mean of 13.6 mg morphine daily). Patients also self-report significant decreases in disability, pain, depression, and pain-related fear. Many comment that they wish they had this active form of treatment earlier after the onset of pain as they perceive they could have avoided years of suffering and disability, and returned to their job before it was permanently lost.
FORDYCE’S FOUR TREATMENT GOALS
1. Reduction of Pain Signals or Pain Behavior
Although the focus of the book is primarily about dysfunctional operant pain behavior, Fordyce also discusses reducing respondent pain behavior. Many respondent pain behaviors are unhelpful after healing has occurred, and can produce harmful physical and social consequences. For example, guarding a painful limb can cause progressive loss of flexibility and strength, increased muscle tension, overuse injury in the contralateral limb, and ultimately increased pain and disability. Auditory or visual displays of respondent pain behavior can cause distress in loved ones, disapproval of an employer, dysfunction in relationships, and possibly prompt responses from others that further reinforce pain behaviors. It is common for patients to have more widespread body pain a year after injury than they had initially due to prolonged guarding, abnormal postures or movement patterns, and general deconditioning. Patients often limit physical activity, gain weight, and become at risk for other medical conditions such as hypertension or Type II diabetes.
Fordyce discusses how therapists can use a graded quota system and arrange contingencies so that reinforcement rather than pain follows movement or activity. His model has provided physical and occupational therapists with a strategy and rationale for getting patients, who are experiencing pain and who are fearful of movement, to engage in behaviors that will facilitate their recovery. Therapists trained in contingency management have a distinct advantage in helping patients recover function. Too many therapists otherwise focus on passive approaches and find it exceedingly difficult to increase functional behaviors in patients demonstrating respondent pain behavior. Progress often does not occur and patients are discharged prematurely because they could not improve.
Many patients referred to our operant treatment program have had physical therapy without significant improvement. Frequently therapy was discontinued because the patient had an increase in pain following movement. When the consequence of activity is pain, activity is punished and will likely decrease, and the patient becomes more fearful and avoidant of movement. If therapy does not follow an appropriate graded quota program, and a patient is asked to exercise to the point of increased pain or fear, it is not only the patient who will experience a negative consequence; the therapist may find that he or she has an unhappy, angry, frightened, and resistant patient who in turn punishes the therapist’s efforts to increase functional activity. They both experience failure and, if that continues, therapy will soon be discontinued. Some therapists view pain within a biomedical model and assume pain complaints reflect a physical problem that could be aggravated by activity. They will then likely stop treatment and send the patient back to his physician for further evaluation. For chronic pain, this is not likely to be of benefit as no treatable pain generator is likely to be identified. Consistent with Fordyce’s recommendations, we have found that when the therapist employs a quota system and the patient starts with a level of activity that is easily below what the patient can perform without significant pain or fear, then activity is reinforced and the patient is subsequently more willing to continue. Increases in activity are programmed at a rate that will allow success at each step. The patient, via a process of graded exposure, also progressively overcomes fear of movement and gains confidence. Although quota-based exercise therapy can yield positive improvements in functional activity, treatment gains are not always maintained once contingent reinforcement has been withdrawn and increases in specific exercises do not necessarily generalize to other activities [3]. Recognizing the lack of maintenance and generalization of improved function in patients treated in interdisciplinary pain rehabilitation programs, the State of Washington Department of Labor & Industries implemented policy to fund six months of follow-up treatment, both face-to-face and remote care, to promote maintenance of treatment gains and generalization of improved function to patients’ home environments.
2. Increasing Activity Level (Reduction of Functional Impairment)
Fordyce discusses the operant approach to increasing activity levels, noting that increased activity and functional behavior automatically limits the amount of activity avoidance or functional impairment allowed. That is, you cannot be active and lying on the couch at the same time. He emphasizes the importance of establishing clear behavioral goals that will continue to be reinforced in the patient’s natural environment and therefore be sustained. Increased activity level is more likely to be maintained after leaving treatment if it allows the patient to engage in highly reinforcing activity in her environment. Walking is a healthy activity, but if it is increased during treatment with the patient’s stated goals of going on enjoyable hikes and outings with the family, and if these recreational activities are part of the post-treatment plan, walking is more likely to be maintained after treatment ends.
Exposure therapy is a common component of interdisciplinary pain rehabilitation programs as a method to decrease pain-related fear and increase functional behavior. Kirsch et al. [8] reviewed data from various sources demonstrating how expectations are learned via observations and verbally provided information. For example, one can observe someone performing an activity followed by the display of pain behavior. It is not necessary to experience pain to vicariously learn that certain activities are likely to cause pain. If a physician tells a patient to avoid lifting, the patient will assume lifting is dangerous, or that lifting will increase pain, and will therefore avoid lifting.
Fordyce did not discount these learning processes. In fact, he demonstrated how subtle messages from physicians, such as saying “let pain be your guide” can change patient behavior via influencing their beliefs and fears about pain [5]. For example, if a physician recommends walking for a back pain problem, and suggests the patient begin a daily walking program, but then qualifies the recommendation by telling the patient “if it hurts, back off on the walking – let pain be your guide,” the patient may assume that walking that causes pain is dangerous. Why else would a doctor tell you to decrease an otherwise healthy activity? In trying to increase activity levels in patients with chronic pain, most clinicians know the effort required to counter all the messages patients have heard from physicians, therapists and family members such as “listen to your body,” “if you have pain you have overdone it,” or “pain is a warning to stop activity.” Fordyce knew well that patients learn from verbally provided information.
3. Reduction of Pain-Related Healthcare Utilization Behavior
Another goal of treatment is to reduce pain-related healthcare utilization. This makes sense financially, but Fordyce also rightly points out the risks to the patient of continued seeking of healthcare. It is not unusual for both the patient and physician to be operating out of a disease model. The patient wants a fix for his or her pain problem and the physician wants to offer some effective treatment. Just this attention from the physician can reinforce operant pain behavior, including healthcare utilization. Excessive seeking of healthcare can also lead to physician ordering of unnecessary and costly diagnostic studies, attempts to treat the pain generator with surgery or other pain alleviating invasive procedures, harmful medication regimens and debilitating restrictions of activity. This disease model approach continues to drive up the cost of healthcare for pain problems and has not improved outcomes or disability rates associated with persistent pain [1,2].
Fordyce notes that it is not only the patient, but also the physician, whose behavior can be influenced by environmental contingencies. In today’s U.S. healthcare environment, physicians are financially rewarded for doing more, especially more expensive diagnostic and treatment procedures. Financial incentives reward surgery, imaging and other diagnostic studies, injections, and other high priced procedures for pain control. Procedural pain clinics have increased in number, whereas interdisciplinary pain rehabilitation programs, employing the principles inspired by Fordyce’s work, despite their demonstrated efficacy, have been decreasing in number because they struggle to be financially viable, in part because insurance carriers are reluctant to reimburse multidisciplinary programs [7].
In the U.S., the Affordable Care Act, a federal statute enacted in 2010 to provide more affordable and better quality healthcare to a larger group of individuals with insurance, and to reduce overall costs to individuals and the government, will likely stimulate more care within Accountable Care Organizations (ACOs) by allowing Medicare to contract with ACOs. Provider groups will provide healthcare for defined groups of 5000 or more patients and be held accountable for quality and cost of care. The incentives are similar to HMOs; that is, to provide quality care in cost-efficient ways in order to keep patients healthy. This is a provider contingency management change of which Fordyce would approve. It can be hoped that incentivizing healthcare systems to have quality and cost-efficient outcomes will lead to fewer expensive invasive procedures for chronic pain and more emphasis on behavioral goals.
Fordyce discusses the topic of legitimizing retirement. He treated many patients with work injuries who were receiving treatment funded by the worker’s compensation system. He gives an example of a middle aged laborer with a back pain problem who can no longer perform heavy labor. The individual has limited intellectual potential for retraining but medically is capable of working at lighter levels of activity. If he has also been out of work for years, the options for future employment are likely quite limited. If the laborer is not legitimately retired, he may continue to seek healthcare, and potentially harmful or expensive treatments, in an attempt to legitimize his disability. Fordyce argues that it would be helpful for the healthcare system to legitimize this person’s retirement to protect him. He also notes that for decisions such as this, someone has to pay; in this case the worker’s compensation carrier will pay retirement benefits.
This construction laborer scenario is a familiar one and his limited return to work options represents one of the largest disincentives for recovery facing the patient. If he improves physically, he may have to accept an undesirable and low paying job, or perhaps not find any job and have no income. If he remains disabled, he may qualify for continued disability income that might pay more than he would earn if he returned to work. Although there may be some value in legitimizing retirement, as Fordyce says, someone has to pay and workers’ compensation carriers, for obvious financial reasons, will avoid funding retirement benefits if at all possible. The laborer will likely be offered retraining for a job, even it is for a job he does not consider desirable. If this retraining option is compared to unemployment with no income the laborer may be incentivized to succeed in rehabilitation and participate in retraining. Although there is not a good solution for this dilemma, Fordyce does point out the importance of recognizing the contingencies for patient, physician, and third party payer behavior. He later was less inclined to suggest pension and argued that permanent disability should be limited to those with objective medical findings causing irremediable impairment, and not awarded on the basis of pain complaints or limited performance of activities [4]. When objective medical evidence does not support disability status, he suggested patients be offered treatment and vocational rehabilitation assistance, but if they still fail to return to work, they should be considered unemployed rather than disabled, and not be continued on disability income.
In our clinic, we help injured workers identify a return to work goal that is acceptable in terms of status, suitability for the individual patient, and level of financial compensation. It is also helpful to highlight for the worker the value of being productive, socially involved with coworkers, and maintaining the potential to increase income over time versus being forever on a fixed disability income. To remove the potential financial reinforcement of pain behavior, it can help to clarify for the patient when the objective medical evidence does not support a disability pension, and he will therefore be expected to return to work in some capacity. The patient may then realize that well behaviors, rather than pain behaviors, are more likely to be reinforced.
This process of helping the injured worker recognize the positive consequences of attempting to return to work is made more difficult if the patient has been told by other providers that he will never work or function normally and that he should be pensioned. These messages from patients’ providers may create an expectation that physical activity, including work, will lead to negative consequences including increased pain, injury, and ultimately failure to be active and productive. While we attempt to make salient the benefits of working, the patient may be hearing conflicting messages from other providers or may have an attorney arguing the merits of a disability pension. If the patient perceives the rewards for continued disability as greater than the rewards of well behaviors, rehabilitation efforts are less likely to be successful.
4. Promotion and Maintenance of Effective Well Behavior
“Well behavior leading to aversive consequences will not long endure (p. 191).” Fordyce thoughtfully makes the point that it is not only important to decrease pain behaviors and increase well behaviors, but also to help establish skills and access to work or leisure environments in which well behaviors will be reinforced. This may involve assistance with improving job skills or facilitating job placement. Or it might involve goal setting to develop more rewarding leisure activities in retirement. It might also involve helping to remove some of the aversive consequences the patient has been able to avoid via pain behavior.
These are important issues to address if well behaviors are to be maintained in the patient’s natural environment, but often very difficult and time consuming problems to resolve. The clinician, as well as the patient, may have limited control over job-related issues, and the patient may have financial need to return to a hostile work environment. Similarly, it may be impossible to alter longstanding relationship dysfunction in which well behaviors are not reinforced. Patients returning to environments that are not reinforcing of positive activity and well behavior are at much greater risk of relapse. Nevertheless, efforts to establish environmental changes that will maintain well behavior are worth the effort.
In interdisciplinary pain rehabilitation programs, it is more feasible to address environmental issues that will facilitate reinforcement of well behaviors. Family members can participate in treatment so they recognize the improved functional abilities of the patient. They are encouraged to reinforce well behaviors and discouraged from being overly protective or solicitous. When a job is available to a patient, provider communication with the employer can help create an environment in which productive activity is reinforced.
A PERSONAL NOTE
I first read this book while working as a psychology trainee in a Veterans Administration inpatient pain management program based on the Fordyce model. My supervisor had traveled to Seattle to train with Bill, and subsequently started a pain management program based on operant principles. We followed the operant approach very closely and saw some truly amazing results. Seeing dramatic behavioral improvements in patients disabled for years with chronic pain solidified my interest in a career of treating chronic pain. I subsequently found myself in Seattle where I worked in programs based on an operant model. Although I did not work directly with Bill, I continued to learn from him and enjoyed seeing him socially. Prior to his death, Bill and his wife Lundy visited the pain management program I direct at Rehabilitation Institute of Washington to see that his work was alive and well, and continuing to help patients with chronic pain. His son David, a talented pain psychologist and neuropsychologist, is still working with us, helping to advance the work that Bill began.
A final observation is that Fordyce uses football players as examples in discussing how respondent pain behaviors can come under the control of environmental contingencies. This does not surprise me as Bill was an avid football fan and had season tickets to his beloved University of Washington Husky’s games for decades. Or perhaps he did not really enjoy football but attended every game in order to observe and study pain and well behaviors.
REFERENCES
1. Chou R, Loeser JD, Owens DK,Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine 2009;34:1066–77.
2. Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22:62–8.
3. Doleys DM, Crocker M, Patton D. Response of patients with chronic pain to exercise quotas. Phys Ther 1982;62: 1111–4.
4. Fordyce WE, editor. Back pain in the workplace: management of disability in nonspecific conditions: a report of the Task Force on Pain in the Workplace, Seattle: IASP Press, 1995.
5. Fordyce WE, Brockway JA, Bergman JA, Spengler D. Acute back pain: a control-group comparison of behavioral vs. traditional management methods. J Behav Med 1986;9:127–40.
6. Hashemi L, Webster BS, Clancy EA. Trends in disability duration and cost of workers’ compensation low back pain claims. (1988–1996). J Occup Environ Med 1998;40:1110–9.
7. IOM (Institute of Medicine). Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press, 2011.
8. Kirsch I, Lynn SJ, Vigorito M, Miller RR. The role of cognition in classical and operant conditioning. J Clin Psychol 2004;60:369–92.
9. Kuner R. Central mechanisms of neuropathic pain. Nature Med 2010;16:1258–66.
10. Spitzer WO, LeBlanc FE, Dupuis M, Abenhaim L, Belanger AY, Bombardier C, Cruess RL, Drouin G, Duval-Hesler N, Laflamme J, Lamoureux G, Nachemson A, Page JJ, Rossignol M, Salmi LR, Salois-Arsenault S, Suissa S, Wood-Dauphinee S. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine 1987;12:S1-S59.
11. Waddell G. The Back Pain Revolution. Edinburgh: Churchill Livingstone, 1998.
Commentary: On Not Treating the Experience of Pain Directly: Some Still Current Dimensions of Pain and Behavior *
Bill Fordyce was one of several psychologists who, in the 1950s and 1960s, began to apply the principles of behavior analysis to a wide range of clinical problems, often to patient groups that were intransigent to conventional biomedical treatment [22]. In 1968, three of these pioneers defined the challenges of applied behavior analysis in classic article ‘Some current dimensions of applied behavior analysis’ [2]. Revisiting the topic 20 years later Baer, Wolf, and Risley [3] observed that many of the issues discussed in 1968 were still current. On re-reading Fordyce’s text in Chapter 5, which I first encountered in the late 1970s, I was struck by the still contemporary resonance of his position.
It is remarkable that Fordyce essentially defined the focus of treatment and a broad set of outcomes for psychological interventions that have endured for 40 years. He eschewed interventions directly aimed at reducing the sensory-intensity discriminative experience of pain and, despite the inclusion of structured distraction techniques, broadly captured in the phrase ‘attention management’ [16] most psychological treatments present rationales that include a focus on at least one of three behavioral outcome domains defined by Fordyce: increasing activity, increasing well-behavior (return to work is emphasized in Fordyce’s account), and decreasing healthcare utilization. The first two of these could be broadly encompassed under the rubric of improved adaptation or coping. Indeed there are some well-structured and efficacious psychological programs explicitly badged as coping skills training. Several years of familiarity with a range of randomized controlled trials for cognitive behavior therapy for chronic pain [17] reveals one or two interesting generalizations.
INCREASING BEHAVIORAL ACTIVITY OFTEN LEADS TO REDUCTION IN REPORTS OF EXPERIENCED PAIN
In one sense this feature separates many psychological approaches to treatment from pharmacological and other biomedical interventions, where the primary aim is to reduce the sensory-intensity experience of pain by modulating some aspect of the neural substrate of the pain pathway. Fordyce discusses possible behavioral methods for achieving this in passing e.g. in a reference to biofeedback (p.179). In the historical context of the 1970s biofeedback appeared to be a promising technology that could modulate the presumed biological substrate that led to pain. Overall, I doubt if biofeedback lived up to its promise as a method for impacting the biological substrate of certain pain conditions. The problem of headache and tension headache reflects this. The ‘simple’ model was that headaches were attributable to sustained increase in muscle groups in the scalp and neck. Biofeedback targeting reduction in muscle activity should therefore, it was argued, reduce the frequency, intensity, and duration of headache. Evidence from treatment trials accrued in support of this conjecture, but other studies failed to find the predicted raised levels of muscle activity. The denouement of the hypothesis was an elegant experiment by Holroyd and his colleagues [10] in which all participants were led to believe that they were learning to reduce muscle activity via the medium of biofeedback. However, for half of the participants feedback was contingent on them increasing their muscle activity. In addition to this, the degree of success that the participants thought they were achieving was experimentally manipulated (high success vs. medium success). The results showed that regardless of the actual change in muscle activity participants who had been led to believe that they were highly successful in achieving reductions in muscle activity had a much greater improvement in their headache activity. Changes in muscle activity, the presumed substrate, were unrelated to symptomatic change. In the example of headache, biofeedback no longer appears to offer a specific behavioral method or ameliorating the presumed biological substrate of pain experience. It may still be used in treatment but it appears to be no more effective than any other psychological treatment aimed at improving generic self-regulatory skills and enhancing self-efficacy [9].
Despite eschewing the reduction of subjective pain experience as a therapeutic goal, most trials measure at least one aspect of it [24]. Moreover, there is consistent evidence that sensory intensity and the highly correlated affective components of pain experience are reduced by active treatment. This phenomenon is very clearly seen in a series of replicated single case studies examining the effectiveness of graded-exposure training for individuals with high levels of fear-avoidance – see chapter 7 in [23]. In this treatment protocol there is no attempt whatsoever to modify a person’s experience of the sensory-intensity dimension of pain. The focus of treatment is on the reduction of fear appraisals and increase in behavioral activity. Yet despite this many patients report considerable reduction in pain during treatment. Increasing behavioral activity often leads to reduction in experienced pain.
THE TENSION BETWEEN NOMOTHETIC AND IDIOGRAPHIC APPROACHES TO ASSESSING BEHAVIOR
When one examines the measures used to document the effectiveness of treatment over the past 30 years they have been heavily weighted towards using standardized questionnaire methodology. Summarized by sample mean and variance, the majority of measures are of cognitive and affective variables (coping, cognitive appraisal and emotional distress) and self-report measures of behavior indirectly measured as disability. It is hard to find a substantial set of trials with return to work as a primary outcome (notable exceptions are those from Nordic countries), and although trialists sometimes record healthcare use it appears not to have been used frequently enough to be consistently included in meta-analyses [24].
I suggest that conceptualization and measurement of ‘pain behavior’ remains a significant and, to a degree, an unresolved issue. Fordyce’s summary of pain behavior is shown in Table 1 alongside the 20 items from a recently developed self-report Pain Behavior Scale (PaB-SR) [4]. Inspection shows that it largely reflects Fordyce’s original scoping of the domain. In the intervening 40 years several attempts have been made to codify and measure pain behavior. These have broadly followed three strategies. The first, exemplified by Fordyce (see his appendix) is for behavioral counts of specified activity. Fordyce identifies broad three categories (sitting, walking and resting) as overall indices of activity for the patient to self-monitor. Elsewhere in his text there are examples of specific counts of behavior in controlled settings e.g. activity on an ergometer. The aim here is to capture the behavioral activity of an individual in context in a truly idiographic manner (i.e., irrespective of norms). This is perhaps a defining feature of the behavioral approach [11].
A second approach is exemplified by Keefe and Block’s direct observational procedure [12] in which participants are required to complete a standard repertoire of activities in a defined context. Trained observers encode a preset and predefined set of pain behaviors e.g. grimacing, guarding. The resulting data are behavioral counts in a controlled setting and the method has the advantage over simple self-monitoring in that reliability in the form of inter-observer agreement may be estimated. The methodological advantages come at the cost of increased resources needed to obtain the measures, and issues of generalization beyond the test environment. Checklists such as the University of Alabama (UAB) Pain Behavior Scale [20] and the Pain Behavior Checklist (PBCL) [13] offer an alternative observational scale to be completed by observers in settings where the activities performed by the patient are not prescribed. Thus, whereas it is possible to compare performance between individuals using Keefe and Block’s method, provided one accepts that the prescribed behavioral tasks are valid, it is more difficult to defend between-person comparisons using tools such as the UAB Pain Behavior Scale where the context varies.
TABLE 1 Pain Behavior Now and Then
Summary of Fordyce’s Original Conceptual Analysis | The 20 Items from the Pain Behaviors Self Report (PaB-SR) Scale. Taken from Table 5 in Cooke et al [4] |
1. Autonomic indicators–flushing, blushing 2. Nonverbal a. Paraverbal–groan, sigh b. Movement–guarding 3. Verbal reports 4. Requests for help 5. Functional limitations–restricted movements, interruption of normal activity | I bit or pursed my lips It showed on my face I asked for someone to help me I grimaced I avoided physical contact with others I groaned I told people I couldn’t do things with them I told people I couldn’t do my usual chores I drew my knees up I stayed very still My muscles tensed up I took medication for the pain I used pillows or other objects to get more comfortable I changed how I breathe I squirmed I lay down I took breaks I rubbed the site of the pain I talked about the pain I changed my posture |
The third approach is probably the most common and is underpinned by strong psychometric measurement models, either classical test theory or item response theory. In contrast to observational approaches, the psychometric approach is nomothetic. These models have impeccable mathematical pedigrees and are the bedrock of much measurement in psychology. There are three features of this approach that are worth contrasting with Fordyce’s behavioral approach. First, the development of these scales depends on the identification of items that share sufficient common variance to index a presumed underlying trait of pain behavior. Items that have meaning and may be clinically definitive for an individual will be discarded if they do not correlate sufficiently with a criterion of common variance. Items are excluded on psychometric grounds rather than their relevance for the individual. Second an individual is scaled with reference some position on the underlying scale referenced by the inherent variability in the scale not by reference to their performance in their unique behavioral world [8]. While the method allows us to measure differences in similarity (common items) between individuals it is not very sensitive to measuring difference in meaningful behavior within an individual either across settings or time; both these attributes are important in evaluating treatments. For the most part scales do not sample the function of the behavior or the context in which it occurs, both essential components of Fordyce’s analysis. This of course has implications for the use and interpretation of measurement in clinical settings, and especially in clinical trials. I venture to suggest, standardized measures, whatever their psychometric provenance and merits may obfuscate real effects, because in their construction items that may have relevance for individuals are culled to fit psychometric requirements. The function and context in which behaviors occur is, generally speaking, sacrificed for psychometric gain.
THE TRANS-DIAGNOSTIC NATURE OF PAIN
By happenstance, Cook et al [4] highlight another critical dimension of Fordyce’s thinking. Fordyce notes that ‘in the main, medicine and healthcare aim at identifying and treating disease and body damage states along type specialization lines’. The division here is between medical specialty, rheumatology, orthopedics, and so on, and thus between different disease states (diagnoses) each characterized by specific mechanisms responsible for the experience of pain. Fordyce notes that pain and behavior may cross specialty boundaries. We might argue that the psychological and behavioral phenomena associated with pain are orthogonal to medical diagnosis: in essence the processes are transdiagnostic [7]. Given the historical context in which Fordyce was writing I suspect that this was quite radical, and I contend that it remains an important position that still requires consideration. Earlier in Fordyce’s text he opens the Pandora’s Box of the relationship between personality and illness. In the years prior to Fordyce’s development of behavioral psychology, quantitative studies of personality and illness, informed by psychodynamic psychology, had been a major focus of enquiry. A popular and well-used text was Alexander’s psychodynamic-psychosomatic typology relating various unresolved and unconscious conflicts to specific disorders [1]. Within disorders such as headache (see early editions of Wolff’s Headache and other Head Pain) consideration is given to various psychological conflicts underlying a range of different headache types. This is not the place to review this approach in detail but in general such studies were scientifically limited by the observational methods and often contained sample biases. Studies on larger unbiased samples tended not to replicate the clinical-observational studies. Outside the explicit psychodynamic school the literature of the time is thick with studies of the personality of pain patients and the behemoth MMPI (Minnesota Multiphasic Personality Inventory) with 556 items was the measurement tool of choice. Drawing conclusions of a causal nature from these studies, which were predominantly cross-sectional, was of course, a fruitless exercise. Nevertheless, the belief that personality is associated with pain syndromes persists and can still be found in the occasional publication.
We should not confuse the issue of personality with other approaches to developing a typology of individuals’ responses to pain; an approach exemplified by Dennis Turk and his colleagues. Just after the publication of Behavioral Methods for Chronic Pain and Illness Turk et al developed the Multidimensional Pain Inventory (MPI) [14]. Originally the West-Haven Yale MPI (WHY-MPI; the choice of acronym was not accidental), the MPI has been used across several diagnostic categories e.g. fibromyalgia, arthritis, low back pain, temporomandibular joint dysfunction (TMJD), by several investigators in a range of settings across continents. Although there is some dispute about the exact number of patient clusters derived after multivariate analysis, three clusters regularly appear and broadly describe a range of adaptation to the experience of persistent pain. The point here is that the evidence from the MPI and similar studies of single measures of constructs, like catastrophizing and various instantiations of coping, is that they appear across medical diagnostic categories. Psychologically what is important is the experience of being molded by persistent pain not the specifics of a particular diagnosis; that is not to deny the fact that there can be marked behavioral differences between people with chronic pain: back pain may impair walking but not eating whereas the reverse is likely to be true in TMJD. From a behavioral point of view, one that I think Fordyce makes clear in his text, the essential issue is the function of behavior not its topology. So modifying walking and eating are manifestations of behavioral strategies to self-manage pain.
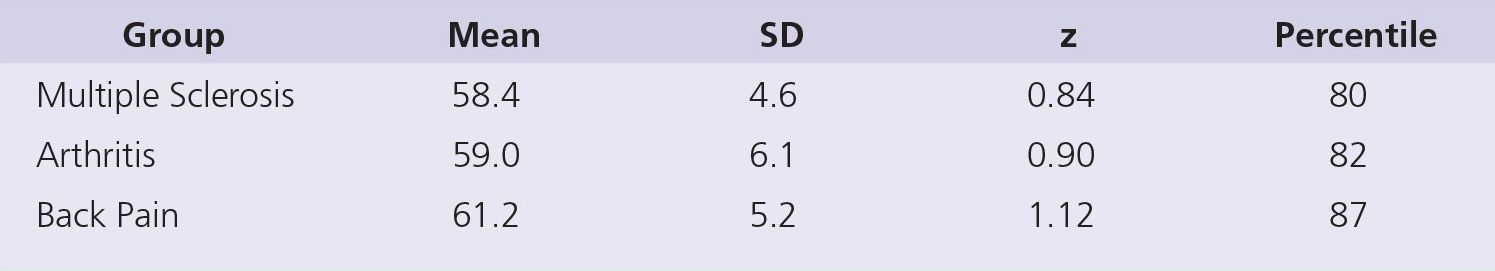
TABLE 2 Summary Data (Mean & SD) from Table 5 in Cook et al [4]. The z Score and Percentile Value for the Mean of Each Sample are Referenced to the Overall Scale Expressed as a T Score (M = 50, SD = 10). The total Sample Size for All Groups was n = 618
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





